LONELY PLANET Loneliness Is More Than Psychic Pain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mar.-Apr.2020 Highlites
Prospect Senior Center 6 Center Street Prospect, CT 06712 (203)758-5300 (203)758-3837 Fax Lucy Smegielski Mar.-Apr.2020 Director - Editor Municipal Agent Highlites Town of Prospect STAFF Lorraine Lori Susan Lirene Melody Matt Maglaris Anderson DaSilva Lorensen Heitz Kalitta From the Director… Dear Members… I believe in being upfront and addressing things head-on. Therefore, I am using this plat- form to address some issues that have come to my attention. Since the cost for out-of-town memberships to our Senior Center went up in January 2020, there have been a few miscon- ceptions that have come to my attention. First and foremost, the one rumor that I would definitely like to address is the story going around that the Prospect Town Council raised the dues of our out-of-town members because they are trying to “get rid” of the non-residents that come here. The story goes that the Town Council is trying to keep our Senior Center strictly for Prospect residents only. Nothing could be further from the truth. I value the out-of-town members who come here. I feel they have contributed significantly to the growth of our Senior Center. Many of these members run programs here and volun- teer in a number of different capacities. They are my lifeline and help me in ways that I could never repay them for. I and the Town Council members would never want to “get rid” of them. I will tell you point blank why the Town Council decided to raise membership dues for out- of-town members. -

Emergency! FREE REGISTRY SERVICE
FINAL-1 Sat, Dec 30, 2017 5:14:57 PM Your Weekly Guide to TV Entertainment for the week of January 6 - 12, 2018 OLD FASHIONED SERVICE Emergency! FREE REGISTRY SERVICE Connie Britton, Angela Bassett and Peter Krause star in “9-1-1” Massachusetts’ First Credit Union When tragedy strikes, police officer Athena Located at 370 Highland Avenue, Salem John Doyle Grant (Angela Basset, “What’s Love Got to Do St. Jean's Credit Union INSURANCEDoyle Insurance AGENCY With It,” 1993), paramedic Bobby Nash (Peter 3 x 3 Voted #1 1 x 3 Krause, “Six Feet Under”) and other first re- Serving over 15,000 Members • A Part of your Community since 1910 Insurance sponders answer the call in “9-1-1,” airing Agency Wednesday, Jan. 10, on Fox. The new drama Supporting over 60 Non-Profit Organizations & Programs from the creators of “Glee” and “American Serving the Employees of over 40 Businesses Horror Story” follows first responders as they Auto • Homeowners • Business • Life Insurance struggle to balance their high pressure careers 978.219.1000 www.stjeanscu.com 978-777-6344 with their personal lives. Offices also located in Lynn, Newburyport & Revere Federally Insured by NCUA www.doyleinsurance.com FINAL-1 Sat, Dec 30, 2017 5:14:58 PM 2 • Salem News • January 6 - 12, 2018 First responders struggle to save the day and themselves in Fox’s ‘9-1-1’ By Kyla Brewer ment deal with 20th Century Fox work, Bassett is best known for Resnick in 2016. In addition to her feld,” “Cybill” and “Sports Night” TV Media Studios. -
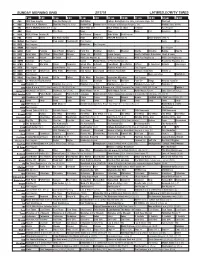
Sunday Morning Grid 2/17/19 Latimes.Com/Tv Times
SUNDAY MORNING GRID 2/17/19 LATIMES.COM/TV TIMES 7 am 7:30 8 am 8:30 9 am 9:30 10 am 10:30 11 am 11:30 12 pm 12:30 2 CBS CBS News Sunday Face the Nation (N) Bull Riding College Basketball Ohio State at Michigan State. (N) PGA Golf 4 NBC Today in L.A. Weekend Meet the Press (N) (TVG) Hockey Day Hockey New York Rangers at Pittsburgh Penguins. (N) Hockey: Blues at Wild 5 CW KTLA 5 Morning News at 7 (N) Å KTLA News at 9 KTLA 5 News at 10am In Touch Paid Program 7 ABC News This Week News News News Paid American Paid 9 KCAL KCAL 9 News Sunday (N) Joel Osteen Jentzen Mike Webb Paid Program 1 1 FOX Planet Weird Fox News Sunday News PBC Face NASCAR RaceDay (N) 2019 Daytona 500 (N) 1 3 MyNet Paid Program Fred Jordan Freethought Paid Program News Paid 1 8 KSCI Paid Program Buddhism Paid Program 2 2 KWHY Paid Program Paid Program 2 4 KVCR Paint Painting Joy of Paint Wyland’s Paint This Painting Kitchen Mexican Martha Christina Baking How To 2 8 KCET Zula Patrol Zula Patrol Mixed Nutz Edisons Curios -ity Biz Kid$ Grand Canyon Huell’s California Adventures: Huell & Louie 3 0 ION Jeremiah Youseff In Touch Paid NCIS: Los Angeles Å NCIS: Los Angeles Å NCIS: Los Angeles Å NCIS: Los Angeles Å 3 4 KMEX Conexión Paid Program Fútbol Fútbol Mexicano Primera División (N) República Deportiva (N) 4 0 KTBN Jeffress Win Walk Prince Carpenter Intend Min. -

Lee Rose Designs
Lee Rose Designs ENTERTAINMENT LIGHTING DESIGN (818) 495-5556 [email protected] leerosedesigns.com For over 45 years, Lee Rose has been designing lighting for television, film, music and theater. Starting in theater, then moving on to touring concert lighting, Lee moved into television and film lighting in the mid-1980’s. From 1984 until 1998, Lee was a partner in Ocean, Rose & Associates, a film and video lighting design firm located in Hollywood. Then in 1998 became a partner in Design Partners, Inc., an award winning association of lighting designers and directors of photography. Now after 18 years Lee is moving on again to start his own firm Lee Rose Designs. Lee has been twice nominated for Emmy Awards for his work with Yanni, including the "Yanni: Live at the Acropolis" concert at the nearly 1500 year old Herod Atticus theatre. He was again nominated for his lighting design work on "Yanni: Tribute", a show that featured concerts taped at the Taj Mahal, in Agra India and The Forbidden City in Beijing China. In addition Lee was awarded Lighting Dimensions "Lighting Designer of the Year" for his lighting design work on that project. Lee’s lighting design work has been seen in feature films including “Southland Tales”, “Bringing Down the House”, "Vanilla Sky" and “Almost Famous”. His television lighting design work is seen on the Chelsea Lately and comedy specials with Eddie Griffin, Nick Cannon and Christopher Titus and annual events such as The Jerry Lewis MDA Telethon, The Daytime Emmy Awards and Revolver’s Golden Gods Awards. Since 1985, Lee has designed the lighting for the music for “Dick Clark’s New Years’ Rockin Eve. -
Fall Course Listing Here
FALL QUARTER 2021 COURSE OFFERINGS September 20–December 12 1 Visit the UCLA Extension’s UCLA Extension Course Delivery Website Options For additional course and certificate information, visit m Online uclaextension.edu. Course content is delivered through an online learning platform where you can engage with your instructor and classmates. There are no C Search required live meetings, but assignments are due regularly. Use the entire course number, title, Reg#, or keyword from the course listing to search for individual courses. Refer to the next column for g Hybrid Course a sample course number (A) and Reg# (D). Certificates and Courses are taught online and feature a blend of regularly scheduled Specializations can also be searched by title or keyword. class meetings held in real-time via Zoom and additional course con- tent that can be accessed any time through an online learning C Browse platform. Choose “Courses” from the main menu to browse all offerings. A Remote Instruction C View Schedule & Location Courses are taught online in real-time with regularly scheduled class From your selected course page, click “View Course Options” to see meetings held via Zoom. Course materials can be accessed any time offered sections and date, time, and location information. Click “See through an online learning platform. Details” for additional information about the course offering. Note: For additional information visit When Online, Remote Instruction, and/or Hybrid sections are available, uclaextension.edu/student-resources. click the individual tabs for the schedule and instructor information. v Classroom C Enroll Online Courses are taught in-person with regularly scheduled class meetings. -

FOR IMMEDIATE RELEASE Los Angeles, CA, April 3, 2020 Howie
FOR IMMEDIATE RELEASE Los Angeles, CA, April 3, 2020 Howie Mandel and ePlay Announce Breakout the Masks Charity and Outbreak Mini-Game Responding to urgent needs related to the Coronavirus Pandemic, the new social and ePlay mobile game campaign will raise money for healthcare and front line workers ePlay Digital Inc. (CSE:EPY), together with comedian, host and producer Howie Mandel, are thrilled to announce Breakout the Masks Charity Campaign and the Howie’s Games project launching today. Working together with non-profit partner, Direct Relief, sports and entertainment mobile game developer ePlay, and Howie Mandel are launching the first in a series of mobile games that allow users to play games to help supply necessary equipment to assist with the Coronavirus outbreak. The Breakout the Masks Charity Campaign was co-created by Mandel to get much-needed masks and Personal Protective Equipment (PPE) to doctors, nurses, and front line workers. Mandel is a well-known germaphobe and well-practiced social-distancer, who’s commitment to Breakout the Masks is instrumental to help show others ways to deal with and overcome anxiety every day. It’s more important than ever to be extra safe with hand-washing and social distancing, but also to learn how to have fun and laugh despite anxieties. “I have spent most of my life in fear of a disease outbreak like COVID-19,” says Howie Mandel. “Let’s work, and play, together, while in self-isolation and keeping social distance, to ensure front line workers - doctors, nurses, and other healthcare workers - are safe, so that they can keep us safe.” Donations to Break out the Masks can be made at www.howiesgames.com and 100% of monies collected from the game, weekly challenges, and the site go to getting doctors, nurses, and front line workers N95 face masks, portable ventilators, gloves, and other PPE to protect from spreading the virus. -

Guantanamo Gazette
Guantanamo Gazette NO (q -- U.S. Navy's only shore-based daily newspaper -- p r , ROICC awards, supervises N and provides policy guidance W EBay News for all contract construction that takes place on base Editor's Note -- This article S takes a close look at the personnel and function of the office of the Guantanamo Bay history. Resident Officer In Charge of Construction. Twenty-six years ago, on Sept. 27, 1961, the Morin Center was By JOSN J.D. Parks dedicated. The center was named after BM2 William Morin, Many new construction projects are Congressional Medal of Honor underway on the base, and contract recipient who, while serving construction companies complete the aboard USS Marblehead, disabled work. 27 contact mines in Guantanamo But who decides what company gets Bay on July, 27, 1898. the contract, and administers the project once the contract is awarded? The office of the Resident Keys Officer In Charge of Construction lost (ROICC) is responsible for A set of keys on a silver key construction contracts on the base. chain was lost at McCalla Hangar "We award, supervise, and provide during quarters today. If found, policy guidance for contract call Robin at 4442 during working construction on the base," Lt. Ondr. hours, or 2217, GHT room 310, Mike Oakes, ROICC, said, adding, after working hours. "The work orders are submitted and the funding is provided by the individual groups or departments. Housing inspections "The biggest projects we have underway now are the senior bachelor Project Planning -- Jack Neill (left), chief engineer officers' at the office of Housing inspections will be quarters, chiefs' barracks the Resident Officer In Charge of Construction (ROICC) and Ensign Eric Dan- and Leeward barracks renovation conducted by the NAVSTA Fire feld, assistant ROICC, discuss a project with a contractor. -

Howie Mandel to Perform at Silver Creek Event Center on Saturday
FOR IMMEDIATE RELEASE HOWIE MANDEL TO PERFORM AT SILVER CREEK EVENT CENTER, FOUR WINDS NEW BUFFALO, ON SATURDAY, APRIL 13 Tickets go on sale Friday, January 18 NEW BUFFALO, Mich. – January 14, 2019 – The Pokagon Band of Potawatomi Indians’ Four Winds® Casinos are pleased to announce Howie Mandel will make a stop at Silver Creek® Event Center on Saturday, April 13, 2019 at 9 p.m. Tickets prices for the show start at $39 plus applicable fees and can be purchased beginning Friday, January 18 at 11 a.m. ET by visiting FourWindsCasino.com, or by calling (800) 745-3000. Hotel rooms are available on the night of the Howie Mandel performance and can be purchased with event tickets. Howie Mandel has remained a constant force in show business for more than 30 years. Mandel currently serves as executive producer and host of the game show “Deal or No Deal,” which returned with new episodes in December 2018 on CNBC. He can also be seen as a judge on the global winter edition of the series, “America’s Got Talent: The Champions,” airs Mondays on NBC. Mandel has served as a judge for nine seasons on NBC’s hit summer talent competition series, “America’s Got Talent,” which recently wrapped its milestone 13th season. Mandel will also release his first solo special in 20 years “Howie Mandel Presents Howie Mandel at the Howie Mandel Comedy Club” on Showtime on Friday, January 18th. His additional work as a host, actor, and/or executive producer include “Take It All” and “Howie Do It” for NBC, “Deal With It” for TBS and “Mobbed” for Fox. -
COMING EVENTS Tuesday, September 1, 2015
Page 8A East Oregonian COMING EVENTS Tuesday, September 1, 2015 TUESDAY, SEPT. 1 WRQ 3XEOLF /LEUDU\ 3 ( *ODG\V $YH ton-)UHHZatHU. )ooG anG FUaIt YHnGoUV. tKoVH XnGHU 0. 3ooO, SX]]OHV, FUaItV, PRESCHOOL STORY TIME, 10:30-11 .QRZ WKH GHDGOLQHV IRU HQUROOPHQW DQG MEDICARE 101, 10 a.m. to noon, 1-3-3 . VnaFNV, 6HFonG 7LmH $UoXnG tKULIt VtoUH DP 6WDQ¿HOG 3XEOLF /LEUDU\ 10 : DVN TXHVWLRQV DERXW FRYHUDJH ¿QDQFLDO 8matLOOa 3XEOLF /LEUaU\, 00 6L[tK 6t. MEDICARE 101, - S.m., 3HnGOH- a.m. to 1 S.m. )oU 0HaOV 2n :KHHOV, &RH $YH 1--1 DVVLVWDQFH IUDXG SURWHFWLRQ DQG PRUH .noZ tKH GHaGOLnHV IoU HnUoOOmHnt anG ton 3XEOLF /LEUaU\, 0 6.:. 'oULon $YH. FaOO 1--1. 1--101 . BOARDMAN SENIOR MEAL SER- )UHH EXU 5693 UHTXLUHG 00--13 aVN TXHVtLonV aEoXt FoYHUaJH, ¿nanFLaO .noZ tKH GHaGOLnHV IoU HnUoOOmHnt anG MEDICARE 101, - S.m., 3oUt oI RU VKLEDRUHJRQ#RUHJRQJRY VICE, 1 QRRQ %RDUGPDQ 6HQLRU &HQWHU aVVLVtanFH, IUaXG SUotHFtLon anG moUH. aVN TXHVtLonV aEoXt FoYHUaJH, ¿nanFLaO 0oUUoZ :HOO 6SLnJV FonIHUHnFH Uoom, 100 7DWRQH 6W &RVWV IRU VHQLRUV RU PENDLETON KNITTING GROUP, )UHH, EXU 5693 UHTXLUHG. 00--13 aVVLVtanFH, IUaXG SUotHFtLon anG moUH. 0aULnH 'ULYH, %oaUGman. .noZ tKH IRU DGXOWV 1-1-3 SP 3URGLJDO 6RQ %UHZHU\ 3XE 30 oU VKLEa.oUHJon#oUHJon.JoY )UHH, EXU 5693 UHTXLUHG. 00--13 GHaGOLnHV IoU HnUoOOmHnt anG aVN TXHV- 6( &RXUW $YH 1--030 oU VKLEa.oUHJon#oUHJon.JoY tLonV aEoXt FoYHUaJH, ¿nanFLaO aVVLV- HERMISTON SENIOR MEAL SER- PRESCHOOL STORY TIME, 10:1 PENDLETON EAGLES BINGO, :30- a.m., 3HnGOHton 3XEOLF /LEUaU\, 0 6.:. -

THE NATIONAL ACADEMY of TELEVISION ARTS & SCIENCES ANNOUNCES the 36Th ANNUAL DAYTIME ENTERTAINMENT EMMY® AWARD NOMINATIONS
THE NATIONAL ACADEMY OF TELEVISION ARTS & SCIENCES ANNOUNCES The 36th ANNUAL DAYTIME ENTERTAINMENT EMMY ® AWARD NOMINATIONS Daytime Emmy Awards to Be Telecast August 30th, 2009 On The CW Television Network at 8:00 p.m. (ET) from The Historic Orpheum Theatre in Los Angeles Sesame Street to Receive Lifetime Achievement Award for 40 Years of Educational Television NATAS Celebrates Nominees with Good Housekeeping at the Hearst Tower New York – May 14, 2009 – The National Academy of Television Arts & Sciences (NATAS) today announced the nominees for the 36th Annual Daytime Entertainment Emmy ® Awards. Nine major categories were announced this morning on “The Today Show,” including the host of the telecast, Vanessa Williams, recording and television star, currently seen on the hit show, “Ugly Betty.” The show will be telecast on the CW Television Network on Sunday, August 30 th , 2009 from the historic Orpheum Theatre in Los Angeles, CA. A complete list of all nominees is available on today.msnbc.msn.com and on emmyonline.tv. The nine categories announced on the Today show were: Outstanding Drama Series Outstanding Lead Actor in a Drama Series Outstanding Lead Actress in a Drama Series Outstanding Supporting Actor in a Drama Series Outstanding Supporting Actress in a Drama Series Outstanding Talk Show/Entertainment Outstanding Talk Show/Informative Outstanding Talk Show Host Outstanding Morning Program Lifetime Achievement Award The show is a unique partnership between NATAS, Associated Television International (ATI), The CW Network and MGM Worldwide Television, which is handling distribution of the telecast. Good Housekeeping is the official print partner of the Daytime Emmy Awards. -

The National Academy of Television Arts & Sciences
THE NATIONAL ACADEMY OF TELEVISION ARTS & SCIENCES ANNOUNCES The 36th ANNUAL DAYTIME ENTERTAINMENT EMMY ® AWARD NOMINATIONS Daytime Emmy Awards to Be Telecast August 30th, 2009 On The CW Television Network at 8:00 p.m. (ET) from The Historic Orpheum Theatre in Los Angeles Sesame Street to Receive Lifetime Achievement Award for 40 Years of Educational Television NATAS Celebrates Nominees with Good Housekeeping at the Hearst Tower New York – May 14, 2009 – The National Academy of Television Arts & Sciences (NATAS) today announced the nominees for the 36th Annual Daytime Entertainment Emmy ® Awards. Nine major categories were announced this morning on “The Today Show,” including the host of the telecast, Vanessa Williams, recording and television star, currently seen on the hit show, “Ugly Betty.” The show will be telecast on the CW Television Network on Sunday, August 30 th , 2009 from the historic Orpheum Theatre in Los Angeles, CA. A complete list of all nominees is available on today.msnbc.msn.com and on emmyonline.tv. The nine categories announced on the Today show were: Outstanding Drama Series Outstanding Lead Actor in a Drama Series Outstanding Lead Actress in a Drama Series Outstanding Supporting Actor in a Drama Series Outstanding Supporting Actress in a Drama Series Outstanding Talk Show/Entertainment Outstanding Talk Show/Informative Outstanding Talk Show Host Outstanding Morning Program Lifetime Achievement Award The show is a unique partnership between NATAS, Associated Television International (ATI), The CW Network and MGM Worldwide Television, which is handling distribution of the telecast. Good Housekeeping is the official print partner of the Daytime Emmy Awards. -

Laugh Fa C Tory
The Kings of Ktown is a stand up comedy special featuring Danny Cho, Walter Hong and Paul “PK” Kim. Kings of Ktown Each comedian will deliver their views on culture, race, family and OVERVIEW livin’ like a King in Koreatown in front of a live audience on July 2nd at the World Famous Laugh Factory in Hollywood. The live show will be filmed as a 1 hour special and will feature them performing stand up comedy as well as behind the scenes footage of the comics backstage, partying in Ktown and promoting the special. WWW.KINGSOFKTOWN.COM 2015 ALL RIGHTS RESERVED - CONFIDENTIAL DOCUMENT OVERVIEW Kings of Ktown stand Up Comedy show + 1 Hour special DVD film taping WHEN Thursday July 2nd, 2015 Showtime: 10 PM WHERE World Famous Laugh Factory 8001 Sunset Blvd Hollywood, CA ATTENDANCE Hosted by: Dumbfoundead Expected attendance: 300 (Limited invitations to: celebrity guests, tastemakers, industry folks, guestlist, & sponsors) WWW.KINGSOFKTOWN.COM 2015 ALL RIGHTS RESERVED - CONFIDENTIAL DOCUMENT AUDienCe AUDIENCE According to 2010 Census, approximately 1.7 million people of Korean descent reside in the U.S., making it the country with the second largest Korean population living outside Korea Asian Americans have $718 Billion in buying power Over 19 Million in the APA Community living in the U.S. Asian Americans are digital pioneers and the leading segment of online shoppers. APA have the highest mobile internet usage on social networks. WWW.KINGSOFKTOWN.COM 2015 ALL RIGHTS RESERVED - CONFIDENTIAL DOCUMENT EMOGRAPHIC D tArget DemogrApHiC - Korean & Asian Pacific -American Community - Tastemakers heavily influenced by social media - Males & Females - 18-35 age segment - Young, tech savvy, that own a smartphone, purchase products online, and are connected to the internet - Have a Bachelor’s degree - Average salary $60K per year WWW.KINGSOFKTOWN.COM 2015 ALL RIGHTS RESERVED - CONFIDENTIAL DOCUMENT AST Danny Cho C Danny Cho is an Asian American comedian/actor.