Inhibiting the Breakdown of Endogenous Opioids and Cannabinoids to Alleviate Pain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Perioperative Opioid-Sparing Analgesia Strategies for Enhanced Recovery After Surgery
Perioperative Opioid-Sparing Analgesia Strategies for Enhanced Recovery After Surgery T. Anthony Anderson, MD PhD Associate Professor Department of Anesthesiology, Perioperative and Pain Medicine Lucile Packard Children's Hospital Stanford Stanford University School of Medicine International Society for Anaesthetic Pharmacology 2018 Annual Meeting Disclosures • I have no relevant relationships to disclose Learning Objectives After this lecture, the listener should be able to: • Identify risks associated with the perioperative use of opioids • Determine opioid-sparing systemic pharmacologic analgesics options • Organize a perioperative analgesic plan to decrease postoperative pain, reduce opioid use, hasten recovery, and improve patient safety Paradigm Shift Surgical Considerations Optimize Co-Morbidities Baseline Pain & Opioid Use Regional techniques Non-pharmacologic Non-opioid Opioids Reasons to Reduce Peri-operative Opioid Use • Relapse risk in patients with a history of opioid use disorder • Improved post-operative recovery • Acute risks • Chronic risks Opioid Use Disorder Relapse • In 2016, 1.8 million people had prescription pain medication use disorder, 5.5% of population • High risk group • Poor evidence for pain management options • Perioperative exposure to relapse triggers: – Stress – Agent of abuse Ward EN, Quaye AN, Wilens TE. Opioid Use Disorders: Perioperative Management of a Special Population. Anesth Analg. 2018 Aug;127(2):539-547. Briand LA, Blendy JA. Molecular and genetic substrates linking stress and addiction. Brain Res. 2010 Feb 16;1314:219-34. ERAS Colorectal Surgery • 13 major perioperative categories • 3 rely heavily on opioid reduction – Multimodal, opioid-sparing pain management – PONV prevention – Ileus reduction • ERAS protocols reduce – Length of hospital stay – Costs – Minor complications Carmichael JC, Keller DS, Baldini G, Bordeianou L, Weiss E, Lee L, Boutros M, McClane J, Feldman LS, Steele SR. -

Original Article Anesthetic Effect of Propofol Combined with Remifentanil and Propofol Combined with Ketamine in Ophthalmic Surgery
Int J Clin Exp Med 2019;12(7):9387-9392 www.ijcem.com /ISSN:1940-5901/IJCEM0079428 Original Article Anesthetic effect of propofol combined with remifentanil and propofol combined with ketamine in ophthalmic surgery Xiaofeng Yi1*, Yanbing Zhang1*, Limin Jin1, Xinjing Yang2 Departments of 1Anesthesia Surgery, 2Emergency ICU, First Affiliated Hospital of Soochow University, Suzhou 215000, Jiangsu, China. *Equal contributors. Received May 10, 2018; Accepted December 7, 2018; Epub July 15, 2019; Published July 30, 2019 Abstract: Propofol combined with ketamine has been used for anesthesia in the past. Remifentanil presented a good analgesic effect, rapid onset, short half-life, and a high clearance rate. Propofol combined with remifentanil also shows good effects in the clinic. This study compared the effect and safety of propofol combined remifentanil and propofol combined ketamine in pediatric eye surgery. Pediatric patients that received eye surgery in our hospital were selected and randomly divided into two groups, the experimental group (n=30), in which patients received pro- pofol combined with remifentanil anesthesia and control group (n=30), and the group receiving propofol combined with ketamine anesthesia. The curative effect, FCO2, SPO2, MAP, HR, anesthesia complications, operation time, recovery time, and leaving PACU time were compared. The rate of good anesthesia was 93.33% in the experimental group, which was significantly higher than control (P < 0.05). FCO2 at 2 and 5 minutes after anesthesia, preopera- tive, intraoperative, and postoperative elevated, while SPO2, MAP, and HR decreased (P < 0.05). The experimen- tal group showed smaller fluctuation range than the control. The rate of Nausea (6.67%), vomiting (3.33%), and somnolence (10%) in the experimental group was significantly lower than control (P < 0.05). -

Federal Register/Vol. 85, No. 36/Monday, February 24, 2020
10466 Federal Register / Vol. 85, No. 36 / Monday, February 24, 2020 / Notices Controlled substance Drug code Schedule Alphamethadol ................................................................................................................................................................. 9605 I Benzethidine .................................................................................................................................................................... 9606 I Betacetylmethadol ........................................................................................................................................................... 9607 I Clonitazene ...................................................................................................................................................................... 9612 I Diampromide ................................................................................................................................................................... 9615 I Diethylthiambutene .......................................................................................................................................................... 9616 I Dimethylthiambutene ....................................................................................................................................................... 9619 I Ketobemidone ................................................................................................................................................................. -

United States Patent (10) Patent No.: US 7,351,739 B2 H0 Et Al
US00735.1739B2 (12) United States Patent (10) Patent No.: US 7,351,739 B2 H0 et al. (45) Date of Patent: Apr. 1, 2008 (54) BIOACTIVE COMPOUNDS AND METHODS 5,354,556. A 10/1994 Sparks et al. OF USES THEREOF 5,360,716 A 1 1/1994 Ohmoto et al. 5,426,181 A 6/1995 Lee et al. (75) Inventors: Chi-Tang Ho, East Brunswick, NJ 5,436,154 A 7/1995 Barbanti et al. (US); Naisheng Bai, Highland Park, NJ 36 A 1. Rht (US); Zigang Dong, Rochester, MN I - w uosianu (US); Ann M. Bode, Cannon Falls, MN 5,523,209 A 6/1996 Ginsberg et al. s s s 5,578,704 A 11/1996 Kim et al. (US); Slavik Dushenkov, Fort Lee, NJ 5,589,570 A 12/1996 At al. (US) 5,591,767 A 1/1997 Mohr et al. 5,610,279 A 3, 1997 Brockhaus et al. (73) Assignees: Wellgen, Inc., New Brunswick, NJ 5,639,476 A 6/1997 OShlack et al. (US); The Regents of the University 5,644,034 A 7/1997 Rathjen et al. of Minnesota, Minneapolis, MN (US); 5,652,109 A 7, 1997 Kim et al. Rutgers, the State University of New 3. g 3. it al. Jersey, New Brunswick, NJ (US) 5,658,746W - W A 8/1997 CoanC. C. eta. al. (*) Notice: Subject to any disclaimer, the term of this 5,665,393 A 9, 1997 Chen et al. patent is extended or adjusted under 35 (Continued) U.S.C. 154(b) by 0 days. -

Characterisation and Partial Purification of a Novel Prohormone Processing Enzyme from Ovine Adrenal Medulla
Volume 246, number 1,2, 44-48 FEB 06940 March 1989 Characterisation and partial purification of a novel prohormone processing enzyme from ovine adrenal medulla N. Tezapsidis and D.C. Parish Biochemistry Group, School of Biological Sciences, University of Sussex, Falmer, Brighton, Sussex, England Received 3 January 1989 An enzymatic activity has been identified which is capable of generating a product chromatographically identical with adrenorphin from the model substrate BAM 12P. This enzyme was purified by gel filtration and ion-exchange chromatog- raphy and characterised as having a molecular mass between 30 and 45 kDa and an acidic pL The enzyme is active at the acid pH expected in the secretory vesicle interior and is inhibited by EDTA, suggesting that it is a metalloprotease. This activity could not be mimicked by incubation with lysosomal fractions and it meets the criteria to be considered as a possible prohormone processing enzyme. Prohormone processing; Adrenorphin; Secretory vesiclepurification 1. INTRODUCTION The purification of an endopeptidase responsi- ble for the generation of adrenorphin was under- Active peptide hormones are released from their taken, using the ovine adrenal medulla as a source. precursors by endoproteolytic cleavage at highly Adrenorphin is known to be located in the adrenal specific sites. The commonest of these is cleavage medulla of all species so far investigated [6]. at pairs of basic residues such as lysine and Secretory vesicles (also known as chromaffin arginine [1,2]. However another common class of granules) were isolated as a preliminary purifica- processing sites are known to be at single arginine tion step, since it is known that prohormone pro- residues, adjacent to a proline [3]. -

Information to Users
The direct and modulatory antinociceptive actions of endogenous and exogenous opioid delta agonists Item Type text; Dissertation-Reproduction (electronic) Authors Vanderah, Todd William. Publisher The University of Arizona. Rights Copyright © is held by the author. Digital access to this material is made possible by the University Libraries, University of Arizona. Further transmission, reproduction or presentation (such as public display or performance) of protected items is prohibited except with permission of the author. Download date 04/10/2021 00:14:57 Link to Item http://hdl.handle.net/10150/187190 INFORMATION TO USERS This ~uscript }las been reproduced from the microfilm master. UMI films the text directly from the original or copy submitted. Thus, some thesis and dissertation copies are in typewriter face, while others may be from any type of computer printer. The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleedthrough, substandard margins, and improper alignment can adversely affect reproduction. In the unlikely. event that the author did not send UMI a complete mannscript and there are missing pages, these will be noted Also, if unauthorized copyright material had to be removed, a note will indicate the deletion. Oversize materials (e.g., maps, drawings, charts) are reproduced by sectioning the original, beginnjng at the upper left-hand comer and contimJing from left to right in equal sections with small overlaps. Each original is also photographed in one exposure and is included in reduced form at the back of the book. Photographs included in the original manuscript have been reproduced xerographically in this copy. -

Enkephalin Degradation in Serum of Patients with Inflammatory Bowel Diseases
Pharmacological Reports 71 (2019) 42–47 Contents lists available at ScienceDirect Pharmacological Reports journal homepage: www.elsevier.com/locate/pharep Original article Enkephalin degradation in serum of patients with inflammatory bowel diseases a, a b Beata Wilenska *, Dagmara Tymecka , Marcin Włodarczyk , b c Aleksandra Sobolewska-Włodarczyk , Maria Wisniewska-Jarosinska , d e b a,d, Jolanta Dyniewicz , Árpád Somogyi , Jakub Fichna , Aleksandra Misicka * a Faculty of Chemistry, Biological and Chemical Research Centre, University of Warsaw, Warszawa, Poland b Department of Biochemistry, Medical University of Lodz, Łódz, Poland c Department of Gastroenterology, Medical University of Lodz, Łódz, Poland d Department of Neuropeptides, Mossakowski Medical Research Centre Polish Academy of Science, Warszawa, Poland e Campus Chemical Instrumentation Centre (CCIC), The Ohio State University, Columbus, OH, USA A R T I C L E I N F O A B S T R A C T Article history: Background: Inflammatory bowel diseases (IBD) are a group of chronic and recurrent gastrointestinal Received 18 April 2018 disorders that are difficult to control. Recently, a new IBD therapy based on the targeting of the Received in revised form 10 June 2018 endogenous opioid system has been proposed. Consequently, due to the fact that endogenous Accepted 1 August 2018 enkephalins have an anti-inflammatory effect, we aimed at investigating the degradation of serum Available online 2 August 2018 enkephalin (Met- and Leu-enkephalin) in patients with IBD. Methods: Enkephalin degradation in serum of patients with IBD was characterized using mass Keywords: spectrometry methods. Calculated half-life (T1/2) of enkephalins were compared and correlated with the Inflammatory bowel diseases disease type and gender of the patients. -

Behavioral and Brain Sciences Plasticity: Implications for Opioid
Behavioral and Brain Sciences http://journals.cambridge.org/BBS Additional services for Behavioral and Brain Sciences: Email alerts: Click here Subscriptions: Click here Commercial reprints: Click here Terms of use : Click here Plasticity: Implications for opioid and other pharmacological interventions in specific pain states Anthony H. Dickenson Behavioral and Brain Sciences / Volume 20 / Issue 03 / September 1997, pp 392 403 DOI: null, Published online: 08 September 2000 Link to this article: http://journals.cambridge.org/abstract_S0140525X97241488 How to cite this article: Anthony H. Dickenson (1997). Plasticity: Implications for opioid and other pharmacological interventions in specific pain states. Behavioral and Brain Sciences,20, pp 392403 Request Permissions : Click here Downloaded from http://journals.cambridge.org/BBS, IP address: 144.82.107.43 on 10 Aug 2012 BEHAVIORAL AND BRAIN SCIENCES (1997) 20, 392±403 Printed in the United States of America Plasticity: Implications for opioid and other pharmacological interventions in specific pain states Anthony H. Dickenson Department of Pharmacology, University College London, London WC1E 6BT, United Kingdom Electronic mail: anthony.dickenson6ucl.ac.uk Abstract: The spinal mechanisms of action of opioids under normal conditions are reasonably well understood. The spinal effects of opioids can be enhanced or reduced depending on pathology and activity in other segmental and nonsegmental pathways. This plasticity will be considered in relation to the control of different pain states using opioids. The complex and contradictory findings on the supraspinal actions of opioids are explicable in terms of heterogeneous descending pathways to different spinal targets using multiple transmitters and receptors ± therefore opioids can both increase and decrease activity in descending pathways. -

(12) United States Patent (10) Patent No.: US 8,501450 B2 N-N-1
USOO85O145OB2 (12) United States Patent (10) Patent No.: US 8,501450 B2 Lin et al. (45) Date of Patent: Aug. 6, 2013 (54) HEPATITIS CVIRUS VARIANTS (56) References Cited (75) Inventors: Chao Lin, Winchester, MA (US); Tara U.S. PATENT DOCUMENTS Kieffer, Brookline, MA (US); 4,835,168 A 5/1989 Paget, Jr. et al. Christoph Sarrazin, Saarland (DE); 5,484.801 A 1/1996 Al-RaZZak et al. Ann Kwong, Cambridge, MA (US) 5,631,128 A 5/1997 Kozal et al. 5,807,876 A 9, 1998 Armistead et al. 5,866,684 A 2f1999 Attwood et al. (73) Assignee: Vertex Pharmaceuticals Incorporated, 5.948,436 A 9, 1999 Al-Razzak et al. Cambridge, MA (US) 5.990,276 A 1 1/1999 Zhang et al. 6,018,020 A 1/2000 Attwood et al. (*) Notice: Subject to any disclaimer, the term of this 6,037,157 A 3/2000 Norbeck et al. patent is extended or adjusted under 35 6,054,472 A 4/2000 Armistead et al. U.S.C. 154(b) by 521 days. (Continued) (21) Appl. No.: 12/718,340 FOREIGN PATENT DOCUMENTS WO WO92fO3918 A1 3, 1992 (22) Filed: Mar. 5, 2010 WO WO94f1443.6 A1 T 1994 (65) Prior Publication Data (Continued) US 2011/0244549 A1 Oct. 6, 2011 OTHER PUBLICATIONS Timm, J., et al., 2007. “Human leukocyte antigen-associated Related U.S. Application Data sequence polymorphisms in Hepatitis C Virus reveal reproducible (62) Division of application No. 1 1/599,162, filed on Nov. immune responses and constraints on viral evolution'. -
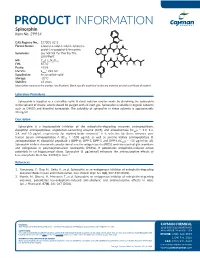
PRODUCT INFORMATION Spinorphin Item No
PRODUCT INFORMATION Spinorphin Item No. 29914 NH CAS Registry No.: 137201-62-8 Formal Name: L-leucyl-L-valyl-L-valyl-L-tyrosyl-L- O H O N prolyl-L-tryptophyl-L-threonine N OH O N H Synonyms: Leu-Val-Val-Tyr-Pro-Trp-Thr, O OH H LVVYPWT O O N MF: C45H64N8O10 N N O FW: 877.0 H H NH2 Purity: ≥95% UV/Vis.: λmax: 222 nm Supplied as: A crystalline solid Storage: -20°C OH Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Spinorphin is supplied as a crystalline solid. A stock solution may be made by dissolving the spinorphin in the solvent of choice, which should be purged with an inert gas. Spinorphin is soluble in organic solvents such as DMSO and dimethyl formamide. The solubility of spinorphin in these solvents is approximately 30 mg/ml. Description Spinorphin is a heptapeptide inhibitor of the enkephalin-degrading enzymes aminopeptidase, dipeptidyl aminopeptidase, angiotensin-converting enzyme (ACE), and enkephalinase (IC50s = 3.3, 1.4, 2.4, and 10 µg/ml, respectively, for monkey brain enzymes).1 It is selective for these enzymes over human serum aminopeptidase A (IC50 = >100 µg/ml), as well as porcine kidney aminopeptidase B, aminopeptidase M, dipeptidyl peptidase 1 (DPP-1), DPP-2, DPP-3, and DPP-4 (IC50s = >55 µg/ml for all). Spinorphin inhibits chemotaxis, production of reactive oxygen species (ROS), and exocytosis of glucuronidase and collagenase in polymorphonuclear neutrophils (PMNs). It potentiates enkephalin-induced action potentials in rat hippocampal slices. -

Stems for Nonproprietary Drug Names
USAN STEM LIST STEM DEFINITION EXAMPLES -abine (see -arabine, -citabine) -ac anti-inflammatory agents (acetic acid derivatives) bromfenac dexpemedolac -acetam (see -racetam) -adol or analgesics (mixed opiate receptor agonists/ tazadolene -adol- antagonists) spiradolene levonantradol -adox antibacterials (quinoline dioxide derivatives) carbadox -afenone antiarrhythmics (propafenone derivatives) alprafenone diprafenonex -afil PDE5 inhibitors tadalafil -aj- antiarrhythmics (ajmaline derivatives) lorajmine -aldrate antacid aluminum salts magaldrate -algron alpha1 - and alpha2 - adrenoreceptor agonists dabuzalgron -alol combined alpha and beta blockers labetalol medroxalol -amidis antimyloidotics tafamidis -amivir (see -vir) -ampa ionotropic non-NMDA glutamate receptors (AMPA and/or KA receptors) subgroup: -ampanel antagonists becampanel -ampator modulators forampator -anib angiogenesis inhibitors pegaptanib cediranib 1 subgroup: -siranib siRNA bevasiranib -andr- androgens nandrolone -anserin serotonin 5-HT2 receptor antagonists altanserin tropanserin adatanserin -antel anthelmintics (undefined group) carbantel subgroup: -quantel 2-deoxoparaherquamide A derivatives derquantel -antrone antineoplastics; anthraquinone derivatives pixantrone -apsel P-selectin antagonists torapsel -arabine antineoplastics (arabinofuranosyl derivatives) fazarabine fludarabine aril-, -aril, -aril- antiviral (arildone derivatives) pleconaril arildone fosarilate -arit antirheumatics (lobenzarit type) lobenzarit clobuzarit -arol anticoagulants (dicumarol type) dicumarol -

Cardioprotective Properties of Opioid Receptor Agonists in Rats with Stress-Induced
Cardioprotective Properties of Opioid Receptor Agonists in Rats with Stress-Induced Cardiac Injury Ekaterina S. Prokudinaa B, Leonid N. Maslova* A, D, E, F, Natlia V. Naryzhnayaa B,G, Sergey Yu. Tsibulnikova B,C,E, Yury B. Lishmanova,b D, John E. Madias PhD c D,E, Peter R. Oeltgen PhD d D,E aLaboratory of Experimental Cardiology, Cardiology Research Institute, Tomsk National Research Medical Center, Russian Academy of Sciences 634012 Tomsk, Russia. bLaboratory of Nuclear Medicine, National Research Tomsk Polytechnic University, Tomsk, Russia. cIcahn School of Medicine at Mount Sinai, and the Division of Cardiology, Elmhurst Hospital Center, New York, New York, USA. dDepartment of Pathology, University of Kentucky College of Medicine, Lexington, KY, USA * Correspondence: Leonid N. Maslov, MD, PhD, DSci, Professor of Pathological Physiology Laboratory of Experimental Cardiology, Federal State Budgetary Scientific Institution «Research Institute for Cardiology», Kyevskaya 111A, 634012 Tomsk, Russia Tel. +7 3822 262174 E-mail address: [email protected] Short title: Stress cardiomyopathy and opioid receptors Summary Purpose The objectives of this study were to investigate the role of endogenous opioids in the mediation of stress-induced cardiomyopathy (SIC), and to evaluate which opioid receptors regulate heart resistance to immobilization stress. Methods Wistar rats were subjected to 24 h 1 immobilization stress. Stress-induced heart injury was assessed by 99mTc-pyrophosphate accumulation in the heart. The opioid receptor (OR) antagonists (naltrexone, NxMB - naltrexone methyl bromide, MR 2266, ICI 174.864) and agonists (DALDA, DAMGO, DSLET, U-50,488) were administered intraperitoneally prior to immobilization and 12 h after the start of stress. In addition, the selective µ OR agonists PL017 and DAMGO were administered intracerebroventricularly prior to stress.