Improving Vascular Maturation Using Non-Coding Rnas Increases Anti-Tumor Effect of Chemotherapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mir-190 Enhances Endocrine Therapy Sensitivity by Regulating SOX9
Yu et al. Journal of Experimental & Clinical Cancer Research (2019) 38:22 https://doi.org/10.1186/s13046-019-1039-9 RESEARCH Open Access miR-190 enhances endocrine therapy sensitivity by regulating SOX9 expression in breast cancer Yue Yu1,2,3,4, Wen Yin1,2,3,4, Zhi-Hao Yu1,2,3,4, Yan-Jun Zhou1,2,3,4, Jiang-Rui Chi1,2,3,4, Jie Ge1,2,3,4 and Xu-Chen Cao1,2,3,4* Abstract Background: Breast cancer is the most common cancer among women worldwide, and approximately 70% of breast cancers are hormone receptor-positive and express estrogen receptor-α (ERα) or/and progesterone receptor. Therapies targeting ERα have been successfully used in patients with ERα+ breast cancer. However, intrinsic or acquired resistance to anti-estrogen therapy presents a major challenge. The Wnt/β-catenin signaling pathway regulates various processes that are important for cancer progression, and emerging evidences have shown a close interaction between Wnt/β-catenin and ERα signaling. miR-190 is also involved in ER signaling and our previous study indicated that miR-190 suppresses breast cancer metastasis. Methods: The effect of miR-190 on breast cancer anti-estrogen sensitivity was investigated both in vitro and in vivo. The protein expression levels and localization were analyzed by western blotting and immunofluorescence, respectively. Chromatin immunoprecipitation and dual-luciferase reporter assays were used to validate the regulation of the zinc-finger E-box binding homeobox 1/ ERα-miR-190-SRY-related high mobility group box 9 (ZEB1/ERα-miR-190-SOX9) axis. Results: miR-190 increased the anti-estrogen sensitivity of breast cancer cells both in vitro and in vivo. -

Cldn19 Clic2 Clmp Cln3
NewbornDx™ Advanced Sequencing Evaluation When time to diagnosis matters, the NewbornDx™ Advanced Sequencing Evaluation from Athena Diagnostics delivers rapid, 5- to 7-day results on a targeted 1,722-genes. A2ML1 ALAD ATM CAV1 CLDN19 CTNS DOCK7 ETFB FOXC2 GLUL HOXC13 JAK3 AAAS ALAS2 ATP1A2 CBL CLIC2 CTRC DOCK8 ETFDH FOXE1 GLYCTK HOXD13 JUP AARS2 ALDH18A1 ATP1A3 CBS CLMP CTSA DOK7 ETHE1 FOXE3 GM2A HPD KANK1 AASS ALDH1A2 ATP2B3 CC2D2A CLN3 CTSD DOLK EVC FOXF1 GMPPA HPGD K ANSL1 ABAT ALDH3A2 ATP5A1 CCDC103 CLN5 CTSK DPAGT1 EVC2 FOXG1 GMPPB HPRT1 KAT6B ABCA12 ALDH4A1 ATP5E CCDC114 CLN6 CUBN DPM1 EXOC4 FOXH1 GNA11 HPSE2 KCNA2 ABCA3 ALDH5A1 ATP6AP2 CCDC151 CLN8 CUL4B DPM2 EXOSC3 FOXI1 GNAI3 HRAS KCNB1 ABCA4 ALDH7A1 ATP6V0A2 CCDC22 CLP1 CUL7 DPM3 EXPH5 FOXL2 GNAO1 HSD17B10 KCND2 ABCB11 ALDOA ATP6V1B1 CCDC39 CLPB CXCR4 DPP6 EYA1 FOXP1 GNAS HSD17B4 KCNE1 ABCB4 ALDOB ATP7A CCDC40 CLPP CYB5R3 DPYD EZH2 FOXP2 GNE HSD3B2 KCNE2 ABCB6 ALG1 ATP8A2 CCDC65 CNNM2 CYC1 DPYS F10 FOXP3 GNMT HSD3B7 KCNH2 ABCB7 ALG11 ATP8B1 CCDC78 CNTN1 CYP11B1 DRC1 F11 FOXRED1 GNPAT HSPD1 KCNH5 ABCC2 ALG12 ATPAF2 CCDC8 CNTNAP1 CYP11B2 DSC2 F13A1 FRAS1 GNPTAB HSPG2 KCNJ10 ABCC8 ALG13 ATR CCDC88C CNTNAP2 CYP17A1 DSG1 F13B FREM1 GNPTG HUWE1 KCNJ11 ABCC9 ALG14 ATRX CCND2 COA5 CYP1B1 DSP F2 FREM2 GNS HYDIN KCNJ13 ABCD3 ALG2 AUH CCNO COG1 CYP24A1 DST F5 FRMD7 GORAB HYLS1 KCNJ2 ABCD4 ALG3 B3GALNT2 CCS COG4 CYP26C1 DSTYK F7 FTCD GP1BA IBA57 KCNJ5 ABHD5 ALG6 B3GAT3 CCT5 COG5 CYP27A1 DTNA F8 FTO GP1BB ICK KCNJ8 ACAD8 ALG8 B3GLCT CD151 COG6 CYP27B1 DUOX2 F9 FUCA1 GP6 ICOS KCNK3 ACAD9 ALG9 -

Differential Gene Expression in the Skin of Xiphophorus
DIFFERENTIAL GENE EXPRESSION IN THE SKIN OF XIPHOPHORUS MACULATUS JP 163 B IN RESPONSE TO FULL SPECTRUM (10,000 K) FLUORESCENT LIGHT by Kaela Caballero, B.S. A thesis submitted to the Graduate Council of Texas State University in partial fulfillment of the requirements for the degree of Master of Science with a Major in Biochemistry August 2015 Committee Members: Ronald Walter, Chair Rachell Booth Steven Whitten COPYRIGHT by Kaela L. Caballero 2015 FAIR USE AND AUTHOR’S PERMISSION STATEMENT Fair Use This work is protected by the Copyright Laws of the United States (Public Law 94-553, section 107). Consistent with fair use as defined in the Copyright Laws, brief quotations from this material are allowed with proper acknowledgment. Use of this material for financial gain without the author’s express written permission is not allowed. Duplication Permission As the copyright holder of this work I, Kaela L. Caballero, authorize duplication of this work, in whole or in part, for educational or scholarly purposes only. DEDICATION To my parents and family, who have always supported and encouraged me, my education and my coffee addiction. And to Max, my study buddy; where you have gone, there is no need for coffee fueled late nights. Rest in peace. ACKNOWLEDGEMENTS This work could not have been accomplished without the support and mentorship that I have received throughout my life from family, teachers, mentors and friends. It is impossible to name everyone here, but I would like to use a few lines to thank those that have helped me achieve my goals. Thank you to Dr. -

Siah - a Promising Anti-Cancer Target
Author Manuscript Published OnlineFirst on March 1, 2013; DOI: 10.1158/0008-5472.CAN-12-4348 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Siah - a promising anti-cancer target Christina SF Wong1 and Andreas Möller1 1 Tumour Microenvironment Laboratory, Queensland Institute of Medical Research, 300 Herston Road, Herston, Queensland 4006, Australia. Corresponding Author: Andreas Möller ([email protected]) Running title: Siah and Cancer Keywords: Siah1, Siah2, E3 Ubiquitin ligases, Cancer Potential conflict of interest: The authors declare no conflict of interest. Word count: Abstract: 100 words; Text: 2590 words; Number of Figures: 1; Number of Tables: 1 1 Downloaded from cancerres.aacrjournals.org on September 29, 2021. © 2013 American Association for Cancer Research. Author Manuscript Published OnlineFirst on March 1, 2013; DOI: 10.1158/0008-5472.CAN-12-4348 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Abstract: Siah ubiquitin ligases play important roles in a number of signaling pathways involved in the progression and spread of cancer in cell-based models but their role in tumor progression remains controversial. Siah proteins have been described to be both oncogenic as well as tumor-suppressive in a variety of patient cohort studies and animal cancer models. This review collates the current knowledge of Siah in cancer progression and identifies potential methods of translation of these findings into the clinic. Furthermore, key experiments needed to close the gaps in our understanding of the role Siah proteins play in tumor progression are suggested. 2 Downloaded from cancerres.aacrjournals.org on September 29, 2021. -

Plasma Cells in Vitro Generation of Long-Lived Human
Downloaded from http://www.jimmunol.org/ by guest on September 24, 2021 is online at: average * The Journal of Immunology , 32 of which you can access for free at: 2012; 189:5773-5785; Prepublished online 16 from submission to initial decision 4 weeks from acceptance to publication November 2012; doi: 10.4049/jimmunol.1103720 http://www.jimmunol.org/content/189/12/5773 In Vitro Generation of Long-lived Human Plasma Cells Mario Cocco, Sophie Stephenson, Matthew A. Care, Darren Newton, Nicholas A. Barnes, Adam Davison, Andy Rawstron, David R. Westhead, Gina M. Doody and Reuben M. Tooze J Immunol cites 65 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription http://www.jimmunol.org/content/suppl/2012/11/16/jimmunol.110372 0.DC1 This article http://www.jimmunol.org/content/189/12/5773.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2012 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 24, 2021. The Journal of Immunology In Vitro Generation of Long-lived Human Plasma Cells Mario Cocco,*,1 Sophie Stephenson,*,1 Matthew A. -

The Microtubule-Binding and Coiled-Coil Domains of Kid Are
© 2016. Published by The Company of Biologists Ltd | Journal of Cell Science (2016) 129, 3609-3619 doi:10.1242/jcs.189969 RESEARCH ARTICLE The microtubule-binding and coiled-coil domains of Kid are required to turn off the polar ejection force at anaphase Shou Soeda1,2,3,4,*, Kaori Yamada-Nomoto1,5,* and Miho Ohsugi1,2,3,*,‡ ABSTRACT throughout mitosis. In addition, the forces generated on the Mitotic chromosomes move dynamically along the spindle chromosome arms contribute to the congression and alignment of microtubules using the forces generated by motor proteins such as the chromosomes during prometaphase and metaphase. The chromokinesin Kid (also known as KIF22). Kid generates a polar chromokinesin Kid (also known as KIF22) is a plus end-directed ejection force and contributes to alignment of the chromosome arms motor protein characterized by a DNA-binding domain (Tokai et al., during prometaphase and metaphase, whereas during anaphase, 1996). During prometaphase and metaphase, Kid is implicated in Kid contributes to chromosome compaction. How Kid is regulated chromosome congression and alignment through generation of a and how this regulation is important for chromosome dynamics remains polar ejection force (PEF) on the chromosome arms (Brouhard and unclear. Here, we address these questions by expressing mutant Hunt, 2005), although the degree of the physiological importance of forms of Kid in Kid-deficient cells. We demonstrate that Cdk1-mediated Kid-mediated PEF varies among species and cell types. Kid in Xenopus phosphorylation of Thr463 is required to generate the polar ejection has been shown to be essential for metaphase chromosome Xenopus force on Kid-binding chromosomes, whereas dephosphorylation alignment in egg extract; however, there is no evidence of of Thr463 prevents generation of the ejection force on such the involvement of Kid in chromosome congression in mouse chromosomes. -

Protein Symbol Protein Name Rank Metric Score 4F2 4F2 Cell-Surface
Supplementary Table 2 Supplementary Table 2. Ranked list of proteins present in anti-Sema4D treated macrophage conditioned media obtained in the GSEA analysis of the proteomic data. Proteins are listed according to their rank metric score, which is the score used to position the gene in the ranked list of genes of the GSEA. Values are obtained from comparing Sema4D treated RAW conditioned media versus REST, which includes untreated, IgG treated and anti-Sema4D added RAW conditioned media. GSEA analysis was performed under standard conditions in November 2015. Protein Rank metric symbol Protein name score 4F2 4F2 cell-surface antigen heavy chain 2.5000 PLOD3 Procollagen-lysine,2-oxoglutarate 5-dioxygenase 3 1.4815 ELOB Transcription elongation factor B polypeptide 2 1.4350 ARPC5 Actin-related protein 2/3 complex subunit 5 1.2603 OSTF1 teoclast-stimulating factor 1 1.2500 RL5 60S ribomal protein L5 1.2135 SYK Lysine--tRNA ligase 1.2135 RL10A 60S ribomal protein L10a 1.2135 TXNL1 Thioredoxin-like protein 1 1.1716 LIS1 Platelet-activating factor acetylhydrolase IB subunit alpha 1.1067 A4 Amyloid beta A4 protein 1.0911 H2B1M Histone H2B type 1-M 1.0514 UB2V2 Ubiquitin-conjugating enzyme E2 variant 2 1.0381 PDCD5 Programmed cell death protein 5 1.0373 UCHL3 Ubiquitin carboxyl-terminal hydrolase isozyme L3 1.0061 PLEC Plectin 1.0061 ITPA Inine triphphate pyrophphatase 0.9524 IF5A1 Eukaryotic translation initiation factor 5A-1 0.9314 ARP2 Actin-related protein 2 0.8618 HNRPL Heterogeneous nuclear ribonucleoprotein L 0.8576 DNJA3 DnaJ homolog subfamily -

Supplementary Information Figure S1
Supplementary Information Figure S1 Figure S2 a Figure S2 b Figure S3 Table S1 Gene transcripts involved in angiogenesis and significantly affected by two HDACi(SAHA and ES8). Table S2 Gene transcripts involved in angiogenesis and significantly affected by DAC and ES8 but not by SAHA. Table S3. List of angiogenesis associated genes that are concomitantly affected by DAC, SAHA and ES8. Table S4. Gene transcripts significantly affected by ES8 but not by either SAHA or DAC and involved in angiogenesis. Symbol Gene name Type(s) Fold change DNER Delta/notch-like EGF related receptor TMR (Trans membrane receptor) 13.3 TMOD1 Tropomodulin 1 Enzyme 4.9 PCSK1 Proprotein convertase subtilisin/kexin type 1 Peptidase 3.8 STMN2 Stathmin-like 2 Other 3.4 PTGS1 Prostaglandin-endoperoxide synthase 1 Enzyme 3.4 (prostaglandin g/h synthase and cyclooxygenase) ITGB3 Integrin, beta 3 (platelet glycoprotein iiia, TMR 3.2 antigen cd61) HSD17B2 Hydroxysteroid (17-beta) dehydrogenase 2 Enzyme 3.1 FTH1 Ferritin, heavy polypeptide 1 Enzyme 3.1 ALDOC Aldolase c, fructose-bisphosphate Enzyme 2.9 HOXB5 Homeobox b5 TR(Transcription regulator) 2.8 PALLD Palladin, cytoskeletal associated protein Other 2.4 SLIT2 Slit homolog 2 (drosophila) Other 2.3 NPTX2 Neuronal pentraxin ii Other 2.2 HOXB4 Homeobox b4 TR 2.2 RGS2 Regulator of g-protein signaling 2, 24kda Other 2.2 IGFBP2 Insulin-like growth factor binding protein 2, Other 2.2 36kda SFRP1 Secreted frizzled-related protein 1 TMR 2.2 CCL20 Chemokine (c-c motif) ligand 20 Cytokine 2.1 TXNIP Thioredoxin interacting protein -

A.1 Primer Sequences Used for SYBR Green Real Time RT-PCR
Supplemental data: A.1 Primer sequences used for SYBR Green real time RT-PCR Table A.1: Primer sequences used for quantitative SYBR Green real time RT-PCR for validation of genes putatively differentially expressed in MDA-MB-468 cells depending on HER2 expression. Gene Accession Primer sequence (5´3´) product # HDACfor GACTTCTACCAACCCACGTGCA NM_004964 HDACrev TTCAACGCATTCCCCATGC API5for TCCAGGGTAAAACGGGTGAG NM_006595 API5rev CAACGACTTTAATCTTGTTCTCTTCTGT ANXA4for GCTCTGCTGGCTATAGTAAAGTGCA NM_001153 ANXA4rev CGAGAAACCATCACTCTGATGAGG DTX4for GCATTCAGGGACCGGAACAC XM_166213 DTX4rev CACGAGCAGCAGCTTCAGAACTT HIF1Afor GATGAAAGAATTACCGAATTGATGG NM_181054 HIF1Arev GTCCTGTGGTGACTTGTCCTTTAGT NR4A2for CGCGGAGAACTCCTAAGGAGG NM_173171 NR4A2rev AACACAAGGCATGGCTTCAGC ZNF165for CCTATGGGACTGTGATAATGAGAGTG NM_003447 ZNF165rev CCAGCTTTGGCATGGATCTACT P4HBfor TCCTCTTTAAGAAGTTTGATGAAGGC NM_000918 P4HBrev CTGTCTGCTCGGTGAACTCGAT TOB1for TGTGTTTGCAGCCTATGGAGG NM_005749 TOB1rev AACAGGCTGGAATTGCTGGTTA SPINT2for GTGCCACTGTCACAGAGAATGC NM_021102 SPINT2rev TTCTGGGAGCACTTGGGACA BHLHB2for CACGGAGACCTACCAGGGATG NM_003670 BHLHB2rev TTGTAGGTCTCCTTGCTGTCCTC BCL2L2for GATGGTGGCCTACCTGGAGA NM_004050 BCL2L2rev AGAGCTGTGAACTCCGCCCA RARRES1for ACTTCTTCAACTTCCGGTCCG NM_206963 RARRES1rev CACCTTCCTGAAGTAAAGACTCTGG SCDfor GCTTCGAAACCGCAGTCCTC NM_005063 SCDrev TAGGAGCTAGAGATATCGTCCTGCA ELF3for GCCATGAGGTACTACTACAAACGG NM_004433 ELF3rev ACTCTGGAGAACCTCTTCCTCCT CHD3for AGGAAGACCAAGACAACCAGTCAG NM_005852 CHD3rev TGACTGTCTACGCCCTTCAGGA S100A14for kind gift of Dr. C. Kerkhoff, Experimental -

Tubular P53 Regulates Multiple Genes to Mediate AKI
BASIC RESEARCH www.jasn.org Tubular p53 Regulates Multiple Genes to Mediate AKI † † † † † Dongshan Zhang,* Yu Liu,* Qingqing Wei, Yuqing Huo, Kebin Liu, Fuyou Liu,* and † Zheng Dong* *Departments of Emergency Medicine and Nephrology, Second Xiangya Hospital, Central South University, Changsha, Hunan, China; and †Department of Cellular Biology and Anatomy, Vascular Biology Center and Department of Biochemistry and Molecular Biology, Georgia Regents University and Charlie Norwood Veterans Affairs Medical Center, Augusta, Georgia ABSTRACT A pathogenic role of p53 in AKI was suggested a decade ago but remains controversial. Indeed, recent work indicates that inhibition of p53 protects against ischemic AKI in rats but exacerbates AKI in mice. One intriguing possibility is that p53 has cell type-specific roles in AKI. To determine the role of tubular p53, we generated two conditional gene knockout mouse models, in which p53 is specifically ablated from proximal tubules or other tubular segments, including distal tubules, loops of Henle, and medullary collecting ducts. Proximal tubule p53 knockout (PT-p53-KO) mice were resistant to ischemic and cisplatin nephrotoxic AKI, which was indicated by the analysis of renal function, histology, apoptosis, and inflammation. However, other tubular p53 knockout (OT-p53-KO) mice were sensitive to AKI. Mechanis- tically, AKI associated with the upregulation of several known p53 target genes, including Bax, p53- upregulated modulator of apoptosis-a, p21, and Siva, and this association was attenuated in PT-p53-KO mice. In global expression analysis, ischemic AKI induced 371 genes in wild-type kidney cortical tissues, but the induction of 31 of these genes was abrogated in PT-p53-KO tissues. -
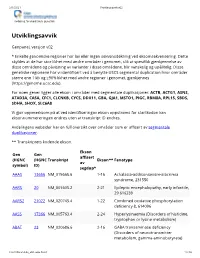
Utviklingsavvik V02
2/1/2021 Utviklingsavvik v02 Avdeling for medisinsk genetikk Utviklingsavvik Genpanel, versjon v02 * Enkelte genomiske regioner har lav eller ingen sekvensdekning ved eksomsekvensering. Dette skyldes at de har stor likhet med andre områder i genomet, slik at spesifikk gjenkjennelse av disse områdene og påvisning av varianter i disse områdene, blir vanskelig og upålitelig. Disse genetiske regionene har vi identifisert ved å benytte USCS segmental duplication hvor områder større enn 1 kb og ≥90% likhet med andre regioner i genomet, gjenkjennes (https://genome.ucsc.edu). For noen gener ligger alle ekson i områder med segmentale duplikasjoner: ACTB, ACTG1, ASNS, ATAD3A, CA5A, CFC1, CLCNKB, CYCS, DDX11, GBA, GJA1, MSTO1, PIGC, RBM8A, RPL15, SBDS, SDHA, SHOX, SLC6A8 Vi gjør oppmerksom på at ved identifiseringav ekson oppstrøms for startkodon kan eksonnummereringen endres uten at transkript ID endres. Avdelingens websider har en full oversikt over områder som er affisert av segmentale duplikasjoner. ** Transkriptets kodende ekson. Ekson Gen Gen affisert (HGNC (HGNC Transkript Ekson** Fenotype av symbol) ID) segdup* AAAS 13666 NM_015665.6 1-16 Achalasia-addisonianism-alacrimia syndrome, 231550 AARS 20 NM_001605.2 2-21 Epileptic encephalopathy, early infantile, 29 616339 AARS2 21022 NM_020745.4 1-22 Combined oxidative phosphorylation deficiency 8, 614096 AASS 17366 NM_005763.4 2-24 Hyperlysinaemia (Disorders of histidine, tryptophan or lysine metabolism) ABAT 23 NM_020686.6 2-16 GABA transaminase deficiency (Disorders of neurotransmitter metabolism, gamma-aminobutyrate) -

Astrocytes Close the Critical Period for Visual Plasticity
bioRxiv preprint doi: https://doi.org/10.1101/2020.09.30.321497; this version posted October 2, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 Astrocytes close the critical period for visual plasticity 2 3 Jérôme Ribot1‡, Rachel Breton1,2,3‡#, Charles-Félix Calvo1, Julien Moulard1,4, Pascal Ezan1, 4 Jonathan Zapata1, Kevin Samama1, Alexis-Pierre Bemelmans5, Valentin Sabatet6, Florent 5 Dingli6, Damarys Loew6, Chantal Milleret1, Pierre Billuart7, Glenn Dallérac1£#, Nathalie 6 Rouach1£* 7 8 1Neuroglial Interactions in Cerebral Physiology, Center for Interdisciplinary Research in 9 Biology, Collège de France, CNRS UMR 7241, INSERM U1050, Labex Memolife, PSL 10 Research University Paris, France 11 12 2Doctoral School N°568, Paris Saclay University, PSL Research University, Le Kremlin 13 Bicetre, France 14 15 3Astrocytes & Cognition, Paris-Saclay Institute for Neurosciences, CNRS UMR 9197, Paris- 16 Saclay University, Orsay, France 17 18 4Doctoral School N°158, Sorbonne University, Paris France 19 20 5Commissariat à l’Energie Atomique et aux Energies Alternatives (CEA), Département de la 21 Recherche Fondamentale, Institut de biologie François Jacob, MIRCen, and CNRS UMR 22 9199, Université Paris-Saclay, Neurodegenerative Diseases Laboratory, Fontenay-aux-Roses, 23 France 24 25 6Institut Curie, PSL Research University, Mass Spectrometry and Proteomics Laboratory, 26 Paris, France 27 28 7Université de Paris, Institute of