Immunotherapy and Vaccination in Surgically Resectable Non-Small Cell Lung Cancer (NSCLC)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Phase 3, Randomized, Double-Blind Study of Adjuvant Cemiplimab Versus Placebo Post-Surgery and Radiation in Patients With
433 A Phase 3, Randomized, Double-Blind Study of Adjuvant Cemiplimab Versus Placebo Post-Surgery and Radiation in Patients with High-Risk Cutaneous Squamous Cell Carcinoma (CSCC) Danny Rischin,1 Matthew G. Fury,2 Israel Lowy,2 Elizabeth Stankevich,3 Siyu Li,2 Hyunsil Han,2 Sandro V. Porceddu4 1Department of Medical Oncology, Peter MacCallum Cancer Centre, Melbourne, Australia; 2Regeneron Pharmaceuticals, Inc., Tarrytown, NY, USA; 3Regeneron Pharmaceuticals, Inc., Basking Ridge, NJ, USA; 4School of Medicine, University of Queensland, Herston, Queensland, Australia; Department of Radiation Oncology, Princess Alexandra Hospital, Woolloongabba, Queensland, Australia. Background Figure 1. C-POST study design Table 2. Key exclusion criteria • Squamous cell carcinoma arising from non-cutaneous sites Summary Cutaneous squamous cell carcinoma (CSCC) Patients with high-risk CSCC often experience relapse with Surgery, with high-risk • Concurrent malignancy other than localized CSCC and/or history of • CSCC is the second most common skin cancer with an estimated features on surgical locoregional recurrence or distant metastases despite initial malignancy other than localized CSCC within 3 years of date of • 1 pathology report incidence of around 1 million cases per year in the US. Worldwide, randomization, except for tumors with negligible risk of metastasis treatment with surgery and post-operative radiation. reports show an annual rise in incidence of 3–7% in most countries.2 350 mg cemiplimab Optional cemiplimab re-treatment after disease recurrence -

Libtayo® (Cemiplimab-Rwlc)
Libtayo® (cemiplimab-rwlc) (Intravenous) Document Number: IC-0398 Last Review Date: 06/01/2021 Date of Origin: 10/30/2018 Dates Reviewed: 11/2018, 03/2019, 06/2019, 09/2019, 12/2019, 03/2020, 6/2020, 12/2020, 03/2021, 06/2021 I. Length of Authorization Coverage will be provided for six months and may be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [NDC Unit]: • Libtayo 350 mg/7 mL single-use vial: 1 vial per 21 days B. Max Units (per dose and over time) [HCPCS Unit]: • 350 billable units every 21 days III. Initial Approval Criteria1 Coverage is provided for the following conditions: • Patient is at least 18 years of age; AND Universal Criteria 1 • Patient has not received previous therapy with a programmed death (PD-1/PD-L1)-directed therapy (e.g., avelumab, pembrolizumab, atezolizumab, durvalumab, nivolumab, dostarlimab, etc.), unless otherwise specified; AND • Used as a single-agent therapy; AND • Patient has not received previous therapy with a cytotoxic T-lymphocyte antigen 4 (CTLA-4) targeting agent (e.g., ipilimumab, etc.) within the 4 weeks prior to therapy; AND Cutaneous Squamous Cell Carcinoma (CSCC) † 1-5 • Patient has nodal or distant metastatic disease, locally advanced disease, inoperable or not fully resectable regional disease, or regional recurrence; AND • Patient is not a candidate for curative surgery or curative radiation therapy Basal Cell Carcinoma (BCC) † 1,2,6 • Patient has locally advanced OR nodal, regional, or distant metastatic disease; AND Proprietary & Confidential © 2021 Magellan Health, -

Northwest Medical Benefit Formulary (List of Covered Drugs) Please Read
Northwest Medical Benefit Formulary (List of Covered Drugs) Please Read: This document contains information about the drugs we cover when they are administered to you in a Participating Medical Office. What is the Kaiser Permanente Northwest Medical Benefit Formulary? A formulary is a list of covered drugs chosen by a group of Kaiser Permanente physicians and pharmacists known as the Formulary and Therapeutics Committee. This committee meets regularly to evaluate and select the safest, most effective medications for our members. Kaiser Permanente Formulary The formulary list that begins on the next page provides information about some of the drugs covered by our plan when they are administered to you in a Participating Medical Office. Depending on your medical benefits, you may pay a cost share for the drug itself. The first column of the chart lists the drug’s generic name. The second column lists the brand name. Most administered medications and vaccines are only available as brand name drugs. Contraceptive Drugs and Devices Your provider may prescribe as medically necessary any FDA-approved contraceptive drug or device, including those on this formulary, which you will receive at no cost share. Last Updated 09/01/2021 Generic Name Brand Name Clinic Administered Medications (ADMD) ABATACEPT ORENCIA ABOBOTULINUM TOXIN A DYSPORT ADALIMUMAB HUMIRA ADO-TRASTUZUMAB EMTANSINE KADCYLA AFAMELANOTIDE ACETATE SCENESSE AFLIBERCEPT EYLEA AGALSIDASE BETA FABRAZYME ALDESLEUKIN PROLEUKIN ALEMTUZUMAB LEMTRADA ALGLUCOSIDASE ALFA LUMIZYME ARALAST, GLASSIA, -
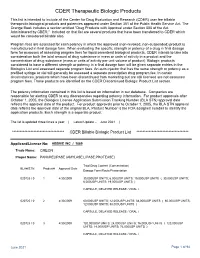
CDER Therapeutic Biologic Products List
CDER Therapeutic Biologic Products This list is intended to include all the Center for Drug Evaluation and Research (CDER) user fee billable therapeutic biological products and potencies approved under Section 351 of the Public Health Service Act. The Orange Book includes a section entitled "Drug Products with Approval under Section 505 of the Act Administered by CBER." Included on that list are several products that have been transferred to CDER which would be considered billable also. Program fees are assessed for each potency in which the approved (non-revoked, non-suspended) product is manufactured in final dosage form. When evaluating the specific strength or potency of a drug in final dosage form for purposes of assessing program fees for liquid parenteral biological products, CDER intends to take into consideration both the total amount of drug substance in mass or units of activity in a product and the concentration of drug substance (mass or units of activity per unit volume of product). Biologic products considered to have a different strength or potency in a final dosage form will be given separate entries in the Biologics List and assessed separate program fees. An auto-injector that has the same strength or potency as a prefilled syringe or vial will generally be assessed a separate prescription drug program fee. In certain circumstances, products which have been discontinued from marketing but are still licensed are not assessed program fees. Those products are identified on the CDER Discontinued Biologic Product List section. The potency information contained in this list is based on information in our database. -

Developmental Therapeutics Immunotherapy
DEVELOPMENTAL THERAPEUTICS—IMMUNOTHERAPY 2500 Oral Abstract Session Clinical activity of systemic VSV-IFNb-NIS oncolytic virotherapy in patients with relapsed refractory T-cell lymphoma. Joselle Cook, Kah Whye Peng, Susan Michelle Geyer, Brenda F. Ginos, Amylou C. Dueck, Nandakumar Packiriswamy, Lianwen Zhang, Beth Brunton, Baskar Balakrishnan, Thomas E. Witzig, Stephen M Broski, Mrinal Patnaik, Francis Buadi, Angela Dispenzieri, Morie A. Gertz, Leif P. Bergsagel, S. Vincent Rajkumar, Shaji Kumar, Stephen J. Russell, Martha Lacy; Mayo Clinic, Rochester, MN; The Ohio State University, Columbus, OH; Mayo Clinic, Scottsdale, AZ; Division of Hematology, Mayo Clinic, Roches- ter, MN; Vyriad and Mayo Clinic, Rochester, MN Background: Oncolytic virotherapy is a novel immunomodulatory therapeutic approach for relapsed re- fractory hematologic malignancies. The Indiana strain of Vesicular Stomatitis Virus was engineered to encode interferon beta (IFNb) and sodium iodine symporter (NIS) to produce VSV-IFNb-NIS. Virally en- coded IFNb serves as an index of viral proliferation and enhances host anti-tumor immunity. NIS was in- serted to noninvasively assess viral biodistribution using SPECT/PET imaging. We present the results of the phase 1 clinical trial NCT03017820 of systemic administration of VSV-IFNb-NIS among patients (pts) with relapsed refractory Multiple Myeloma (MM), T cell Lymphoma (TCL) and Acute myeloid Leu- 9 kemia (AML). Methods: VSV-IFNb-NIS was administered at 5x10 TCID50 (50% tissue culture infec- 11 tious dose) dose level 1 to dose level 4, 1.7x10 TCID50. The primary objective was to determine the maximum tolerated dose of VSV-IFNb-NIS as a single agent. Secondary objectives were determination of safety profile and preliminary efficacy of VSV-IFNb-NIS. -

Libtayo® (Cemiplimab-Rwlc)
Libtayo® (cemiplimab-rwlc) (Intravenous) -E- Document Number: IC-0473 Last Review Date: 07/01/2021 Date of Origin: 07/01/2019 Dates Reviewed: 07/2019, 10/2019, 01/2020, 04/2020, 07/2020, 10/2020, 01/2021, 04/2021, 07/2021 I. Length of Authorization Coverage will be provided for six months and may be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [NDC Unit]: • Libtayo 350 mg/7 mL single-use vial: 1 vial per 21 days B. Max Units (per dose and over time) [HCPCS Unit]: 350 billable units every 21 days III. Initial Approval Criteria 1 Coverage is provided for the following conditions: • Patient is at least 18 years of age; AND Universal Criteria 1 • Patient has not received previous therapy with a programmed death (PD-1/PD-L1)-directed therapy (e.g., avelumab, pembrolizumab, atezolizumab, durvalumab, nivolumab, dostarlimab, etc.), unless otherwise specified; AND • Used as single-agent therapy; AND • Patient has not received previous therapy with a cytotoxic T-lymphocyte antigen 4 (CTLA-4) targeting agent (e.g., ipilimumab, etc.) within the 4 weeks prior to therapy; AND • Patient does not have a history of a solid organ transplant; AND Cutaneous Squamous Cell Carcinoma (CSCC) † 1-5 • Patient has nodal or distant metastatic disease, locally advanced disease, inoperable or not fully resectable regional disease, or regional recurrence; AND • Patient is not a candidate for curative surgery or curative radiation therapy Basal Cell Carcinoma (BCC) † 1,2,6 • Patient has locally advanced OR nodal, regional, or distant metastatic disease; AND Moda Health Plan, Inc. Medical Necessity Criteria Page 1/10 Proprietary & Confidential © 2021 Magellan Health, Inc. -

Immunotherapy Update Review of Immune Checkpoint Inhibitor and CAR T-Cell Therapy Adverse Effects and Treatments
Cancer immunotherapy update Review of immune checkpoint inhibitor and CAR T-cell therapy adverse effects and treatments. By Victoria L. Anderson, MSN, CRNP, FAANP, and Leslie Smith, MSN, RN, AOCNS, APRN-CNS BECAUSE cancer treatment (surgery, radia- ments—immune checkpoint inhibitors and CNE tion, and chemotherapy) frequently fails, chimeric antigen receptor (CAR) T-cell thera- 1.5 contact hours research ers began asking why patients’ im- py—their immune-related adverse effects, mune systems don’t respond to cancer cells and treatment options. By understanding LEARNING like they do to bacteria and viruses. Under how these treatments work and their possible OBJECTIVES normal conditions, T lymphocytes (T-cells) adverse effects, nurses can better educate pa- 1. Describe how bind to a tumor cell via programmed cell tients and intervene quickly when necessary. immune check- death protein 1 (PD-1) and programmed point inhibitors death ligand 1 (PD-L1) receptors and then Immune checkpoint inhibitors and chimeric send signals that recruit antigen-presenting Immune checkpoint inhibitors (CTLA-4, PD-1, antigen recep- cells (APCs) that attach to the T-cells via and PD-L1) have emerged as potential targets tor (CAR) T-cell the cytotoxic T lympho cyte antigen-4 (CT- in the development of new cancer drugs. therapy work. LA-4) binding arm. Next, a series of cy- 2. Discuss adverse tokines (such as gamma interferon, inter- CTLA-4 inhibitors effects related leukin 12 and B7) work to kill the T-cell and Immune tolerance is the process described to immune the tumor cell through apoptosis (cell by Schwartz as an “anticipatory organ” that checkpoint in- death). -

Picture As Pdfoctober 2020: Reminder Specific Medications
OCTOBER 2020: REMINDER SPECIFIC MEDICATIONS REQUIRE PRIOR AUTHORIZATION As a part of our continuous efforts to improve the quality of care for our members, Highmark Health Options wanted to send a reminder about the prior authorization process for the following medications. Failure to obtain authorization will result in a claim denial. The prior authorization process applies to all Highmark Health Options Members. Medical necessity criteria for each of the medications listed below are outlined in the specific medication policies available online. To access Highmark Health Options’ medical policies, please paste the following link in your internet browser: https://www.highmarkhealthoptions.com/providers/medication-information.html. PROCEDURE CODES REQUIRING AUTHORIZATION DRUG NAME CODE DESCRIPTION HCPCS DE Medicaid Injection, abatacept, 10 mg (code may be used for Medicare when drug administered under J0129 11/4/2019 the direct supervision of a physician, not for abatacept (Orencia) use when drug is self administered aflibercept (Eylea) Injection, aflibercept, 1 mg J0178 10/1/2018 agalsidase beta (Fabrazyme) Injection, agalsidase beta, 1 mg J0180 6/3/2019 alemtuzumab (Lemtrada) Injection, alemtuzumab, 1 mg J0202 11/4/2019 alglucosidase alfa (Lumizyme) Injection, alglucosidase alfa, (lumizyme), 10 mg J0221 10/1/2018 aprepitant (Cinvanti) Injection, aprepitant, 1 mg J0185 11/4/2019 asparaginase (Erwinaze) Injection, asparaginase (erwinaze), 1,000 iu J9019 11/4/2019 atezolizumab (Tecentriq) Injection, atezolizumab, 10 mg J9022 11/4/2019 Axicabtagene -

Chemotherapy Protocol SKIN CANCER Cemiplimab (350Mg)
Chemotherapy Protocol SKIN CANCER Cemiplimab (350mg) Regimen • Skin – Cemiplimab (350mg) Indication • Metastatic or locally advanced cutaneous squamous cell carcinoma in patients who are not candidates for curative surgery or curative radiation. Toxicity Drug Adverse Effect Immune-related reactions including pneumonitis, colitis, hepatitis, hypothyroidism and hyperthyroidism. Fatigue, rash, pruritis, Cemiplimab muscular skeletal pain, arthralgia, central nervous system disorders and infusion related reactions The adverse effects listed are not exhaustive. Please refer to the relevant Summary of Product Characteristics for full details. Monitoring • FBC, LFTs and U&Es prior to each cycle for 8 cycles then every 12 weeks or as clinically indicated • Thyroid function tests at baseline then every 6 weeks or as clinically indicated • Blood glucose monitoring every 6 weeks or as clinically indicated Dose Modifications The dose modifications listed are for haematological, liver and renal function and some drug specific toxicities only. Dose adjustments may be necessary for other toxicities as well. The dose modifications listed are for haematological, liver and renal function and some drug specific toxicities. Cemiplimub belongs to the immunotherapy class of cancer treatments. Autoimmune toxicities are most frequently noted and can be life threatening. If autoimmune toxicities occur delaying treatment should be considered while investigations or treatments are organised. Some, but not all, toxicities mandate cessation of treatment. Please seek guidance from relevant site specific specialist teams or oncologists / haematologists with experience of prescribing these agents. Clinicians should be aware that the current funding approval precludes further treatment after an interruption of 12 weeks or longer; this situation may change. Refer to the latest version of the European Society of Medical Oncology guidelines; Management of toxicities from immunotherapy: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up (1) . -

Specialty Pharmacy on Strategies and Analysis for Managing High-Cost Specialty Products
Specialty Pharmacy on Strategies and Analysis for Managing High-Cost Specialty Products Opinions Vary on How Useful Requiring WACs on TV Ads Will Be October 2018 While HHS has taken multiple steps toward lowering prescription drug prices, VOLUME 15 | NUMBER 10 the agency’s latest proposal has been its most contentious so far. And while it may succeed in providing consumers more information on drugs’ wholesale acquisition costs (WACs), industry experts wonder how effective it really will be in letting con- Cost of Care, Drug Burden 3 sumers know what they will pay for a drug. Can Be Challenge in Managing CF HHS Secretary Alex Azar unveiled the proposal during a speech at the National Academy of Medicine’s annual meeting Oct. 15. The proposed rule (83 Fed. Reg. 6 MDs May Be Prescribing 22698, Oct. 18, 2018) is scheduled to be published Oct. 18 in the Federal Register. IL-17 Inhibitors as The proposed rule would require direct-to-consumer (DTC) television ads for First-Line Drugs prescription drugs covered by Medicare or Medicaid that have a WAC of more than $35 per month to include that list price in the ad. Specifically, an ad “must contain 7 Coinsurance Continues to a statement or statements indicating the Wholesale Acquisition Cost (referred to Be Top Cost-Share Tactic as the ‘list price’) for a typical 30-day regimen or for a typical course of treatment, Among Specialty Tiers whichever is most appropriate, as determined on the first day of the quarter during which the advertisement is being aired or otherwise broadcast, as follows: ‘The list 8 New FDA Specialty Approvals price for a [30-day supply of ] [typical course of treatment with] [name of prescrip- tion drug or biological product] is [insert list price]. -

PRAC Draft Agenda of Meeting 14-17 April 2020
14 April 2020 EMA/PRAC/132684/2020 Human Division Pharmacovigilance Risk Assessment Committee (PRAC) Draft agenda for the meeting on 14-17 April 2020 Chair: Sabine Straus – Vice-Chair: Martin Huber 14 April 2020, 10:30 – 19:30, via teleconference 15 April 2020, 08:30 – 19:30, via teleconference 16 April 2020, 08:30 – 19:30, via teleconference 17 April 2020, 08:30 – 16:00, via teleconference Organisational, regulatory and methodological matters (ORGAM) 30 April 2020, 09:00-12:00, via teleconference Health and safety information In accordance with the Agency’s health and safety policy, delegates are to be briefed on health, safety and emergency information and procedures prior to the start of the meeting. Disclaimers Some of the information contained in this agenda is considered commercially confidential or sensitive and therefore not disclosed. With regard to intended therapeutic indications or procedure scopes listed against products, it must be noted that these may not reflect the full wording proposed by applicants and may also change during the course of the review. Additional details on some of these procedures will be published in the PRAC meeting highlights once the procedures are finalised. Of note, this agenda is a working document primarily designed for PRAC members and the work the Committee undertakes. Note on access to documents Some documents mentioned in the agenda cannot be released at present following a request for access to documents within the framework of Regulation (EC) No 1049/2001 as they are subject to on- going procedures for which a final decision has not yet been adopted. -

Mrx CLINICAL ALERT
MRx NOVEMBER 2018 CLINICAL ALERT YOUR MONTHLY SOURCE FOR DRUG INFORMATION HIGHLIGHTS HOT TOPIC: While yearly vaccination is the primary NEW FLU MED APPROVED means of preventing and controlling EDITORIAL flu outbreaks, treatment with antiviral Influenza places a considerable burden agents can lessen symptoms, shorten STAFF on the United States (US) healthcare duration of illness, and prevent serious system, with up to 35 million cases complications. reported each year. As the 2018- EDITOR IN CHIEF 2019 flu season gets underway, the UPDATED CONSENSUS ON Maryam Tabatabai Food and Drug Administration (FDA) DIABETES MANAGEMENT PharmD granted Priority Review and approval for Genentech/Shionogi’s baloxavir The American Diabetes Association marboxil (Xofluza™), the first new (ADA) and the European Association for EXECUTIVE EDITOR novel influenza antiviral in nearly 20 the Study of Diabetes (EASD) updated Carole Kerzic years. The new agent is indicated to their 2015 joint position statement on RPh treat acute uncomplicated influenza the management of type 2 diabetes in people ≥ 12 years of age with flu mellitus (T2DM). It includes a new DEPUTY EDITORS symptoms for ≤ 48 hours. Baloxavir decision cycle for patient-centered Stephanie Christofferson marboxil uses a unique mechanism glycemic management with a goal PharmD of action to block the replication of to prevent diabetes complications influenza A and B viruses, including and enhance quality of life (QOL). Jessica Czechowski Avian strains (H7N9, H5N1). In clinical Greater focus is placed on lifestyle PharmD studies, it was well tolerated and management and diabetes self- eased flu symptoms in about the management education and support. Lara Frick same amount of time as the market Weight loss strategies include lifestyle, PharmD, BCPS, BCPP leader, oral oseltamivir (Tamiflu®), and medical nutrition therapy (MNT), significantly less time compared to medication, and surgical interventions.