Establishing Tolerable Upper Intake Levels and a Risk Assessment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
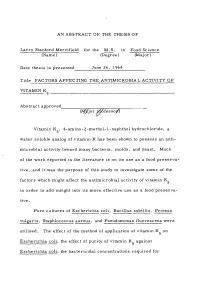
An Abstract of the Thesis Of
AN ABSTRACT OF THE THESIS OF Larry Stanford Merrifield for the M.S. in Food Science (Name) (Degree) (Major) Date thesis is presented June 26, 1964 Titie FACTORS AFFECTING THE ANTIMICROBIAL ACTIVITY OF VITAMIN K 5 Abstract approved (M^jor Tp&Sfesso/) Vitamin K, 4-amino-2-methyl- 1-naphthol hydrochloride, a 5 water soluble analog of vitamin K has been shown to possess an anti- microbial activity toward many bacteria, molds, and yeast. Much of the work reported in the literature is on its use as a food preserva- tive, and it was the purpose of this study to investigate some of the factors which might affect the antimicrobial activity of vitamin K in order to add insight into its more effective use as a food preserva- tive. Pure cultures of Escherichia coli, Bacillus subtilis, Proteus vulgaris, Staphlococcus aureus, and Pseudomonas fluorescens were utilized. The effect of the method of application of vitamin K on Escherichia coli; the effect of purity of vitamin K against Escherichia coli; the bactericidal concentrations required for Escherichia coli, Bacillus subtilis, Proteus vulgaris, Staphlococcus aureus, and Pseudomonas fluorescens; the effect of an absence of oxygen; the effect of contact time with Escherichia coli; the effect of initial count/ml of Escherichia coli; and the synergistic action in combination with propylene glycol were studied. The results demonstrated that air oxidation of vitamin K was 5 necessary to obtain maximum inhibitory activity against Escherichia coli. The use of white, crystalline vitamin K synthesized in the laboratory, as compared to partially oxidized commercial prepara- tions, gave better results against Escherichia coli. -

Molybdenum Studies with Sheep
MOLYBDENUM STUDIES WITH SHEEP By GIUMA M. SHERIH.A Bachelor of Science Cairo University Cairo, Egypt 1957 Submitted to the faculty of the Graduate School of the Oklahoma State Univ~rsity of Agriculture and Applied Science in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE Kay, 1961 MOLYBDENUM STUDIES WITH SHEEP Thesis Approved: I Dean of the Graduate School ii OKLAHOMA STATE UNIVERSITY LIBRARY JAN 2 1962 ACKNOWLEDGEMENT The author wishes to express his deep appreciation to Dr. A. D. Tillman, Professor in the Department of Animal Husbandry, for his valu- able suggestions in planning and carrying out these studies and in writing this thesis. Grateful acknowledgement is also extended to Dr. R. J. Sirny, Associate Professor in the Department of Biochemistry for his invaluable assistance in determining the molybdenum content of the basal rations fed in these studies. 481211 iii- TABLE OF CONTENTS Page INTRODUCTION. • • • REVIEW OF LITERATURE • • • • • • • • • • 2 Molybdenum Toxicity in Ruminants. • • • • 2 Molybdenum, Copper, Sulfur, and Phosphorus Interactions. • 4 Molybdenum and Xanthine Oxidase • • • • 7 Molybdenum as a Dietary Essential for Growth. • • 13 EXPERD"iENT I • • • 1.5 Experimental Procedure. • • 15 Results and Discussion. • 1? Summary • 18 EXPERIMENT II • • • • 19 Experimental Procedure • 19 Results and Discussion. 21 Summary • • • 22 EXPER L'VIENT III • • 23 Experimental Procedure. • • • 2J Results and Discussion. • • • • • • • 24 Summary. • • 2.5 EXPERIMENT IV • • 26 Experimental Procedure. • • • • 26 Results and Discussion. • • • 0 26 Summary • • • • • 29 EXPERIMENT V. • 30 Experimental Procedure. • • • • JO Results and Discussion. • • • • J1 Summary 32 LITERATURE CITED. 33 iv LIST OF TABLES Table Page I. Perc.entage Composition of the Semi-Purified Ration •• • • • • 16 II. -
Zinc Citrate – a Highly Bioavailable Zinc Source
Wellness Foods Europe THE MAGAZINE FOR NUTRITION, FUNCTIONAL FOODS & BEVERAGES AND SUPPLEMENTS Zinc citrate – a highly bioavailable zinc source Reprint from Wellness Foods Europe issue 3/2014 Wellness Foods Europe Special salts Zinc citrate – a highly bioavailable zinc source Markus Gerhart, Jungbunzlauer Ladenburg GmbH Zinc, the versatile mineral, is about to be- Zinc is a component of about 300 enzymes and come the next star in the minerals catego- 2000 transcriptional factors, and 10 % of the ry. Profiting from its various health benefits human proteome contain zinc-binding motives. and its relatively low cost in use, zinc sales Impairment of intestinal zinc absorption results in supplements have shown a double digit in severe clinical manifestations like skin lesions, growth in 2012 and are starting to catch up developmental retardation, stunted growth and with calcium, magnesium and iron, the cate- immune deficiency. gory leaders. Its importance for human health was empha- sised by the European health claim regu lation, Zinc is an essential transition metal that is where zinc received more positive opinions (18 directly or indirectly involved in a wide varie- in total) than any other mineral. The range of ty of physiological processes. After discover- claims (Table 1) includes, amongst others, im- ing the necessity of zinc for Aspergillus niger, it portant health benefits like immunity, bone took another 100 years before its relevance for health, cognitive function and healthy vision. humans was recognised, when the zinc deficien- These health benefits can be clearly defined and cy syndrome was described for the first time by are easy for the consumer to understand. -

DESCRIPTION Nicadan® Tablets Are a Specially Formulated Dietary
DESCRIPTION niacinamide may reduce the hepatic metabolism of primidone Nicadan® tablets are a specially formulated dietary supplement and carbamazepine. Individuals taking these medications containing natural ingredients with anti-inflammatory properties. should consult their physician. Individuals taking anti- Each pink-coated tablet is oval shaped, scored and embossed diabetes medications should have their blood glucose levels with “MM”. Nicadan® is for oral administration only. monitored. Nicadan® should be administered under the supervision of a Allergic sensitization has been reported rarely following oral licensed medical practitioner. administration of folic acid. Folic acid above 1 mg daily may obscure pernicious anemia in that hematologic remission may INGREDIENTS occur while neurological manifestations remain progressive. Each tablet of Nicadan® contains: Vitamin C (as Ascorbic Acid).................100 mg DOSAGE AND ADMINISTRATION Niacinamide (Vitamin B-3) ..................800 mg Take one tablet daily with food or as directed by a physician. Vitamin B-6 (as Pyridoxine HCI) . .10 mg Nicadan® tablets are scored, so they may be broken in half Folic Acid...............................500 mcg if required. Magnesium (as Magnesium Citrate).............5 mg HOW SUPPLIED Zinc (as Zinc Gluconate).....................20 mg Nicadan® is available in a bottle containing 60 tablets. Copper (as Copper Gluconate)..................2 mg 43538-440-60 Alpha Lipoic Acid...........................50 mg Store at 15°C to 30°C (59°F to 86°F). Keep bottle tightly Other Ingredients: Microcrystalline cellulose, Povidone, closed. Store in cool dry place. Hypromellose, Croscarmellose Sodium, Polydextrose, Talc, Magnesium Sterate Vegetable, Vegetable Stearine, Red Beet KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF Powder, Titanium Dioxide, Maltodextrin and Triglycerides. CHILDREN. -

Antioxidants During Your Radiation Therapy
Form: D-5021 What You Need to Know About Taking Antioxidants During Your Radiation Therapy For patients getting radiation therapy Read this brochure to know: • should you take antioxidants during radiation treatment • which vitamins and supplements are safe to take during radiation therapy • what are food sources with antioxidants • where to get more information What are antioxidants? Antioxidants are nutrients found in some foods and also in supplements such as pills. Antioxidants help your body protect your cells from damage and help your body repair damage to your cells. They are good for normal cells because they help repair and prevent damage. Should I take antioxidants during radiation therapy? The goal of radiation therapy is to damage your cancer cells. Antioxidants may prevent your radiation treatment from being as effective because they may protect your cancer cells. Avoid taking large amounts of antioxidants during your radiation therapy treatment. Avoid taking these antioxidant pills in large amounts such as: • vitamin C • vitamin E • beta carotene • selenium Look at the side of your supplement or multivitamin bottle to check the amount of antioxidants. Below is a table of safe amounts of antioxidants you can take while having treatment. Do not take more than the amount listed. Name of antioxidant Do NOT take more than: Vitamin C 90 milligrams per day for men 75 mg per day for women Vitamin E natural Vitamin E (d-alpha- 22 IU per day tocopherol) synthetic Vitamin E (dl- 33 IU per day alpha-tocopherol) Selenium 55 micrograms per day Beta carotene Avoid because there is no safe level IU = International Unit 2 The safe amounts of antioxidants listed in the table come from Health Canada. -

The Role of Nutritional Therapies in the Care Of
© Michael Ash BSc DO ND F.DipION 2010 4/29/2010 'The role of Nutritional Therapy in the care of individuals with cardiovascular related problems' Michael Ash BSc (Hons) DO ND F DipION mBANT NTCC Osteopath Naturopath Nutritional Therapist Researcher Author Nutritional Therapy • A Functional Medicine approach to optimise outcomes, ease of engagement and compliance. • 8 Practical strategies & how to avoid common pitfalls. • Interaction of the immune system with the heart. • GastroCentric Perspective. • How food selection can provide a multi faceted benefit. • Supplements of benefit. 1 © Michael Ash BSc DO ND F.DipION 2010 4/29/2010 Client Overview Goals Determine their aims and outcomes – the purpose of the plan is to support the patients goals with evidence based strategies Identify realistic goals, obtain agreement that these are achievable and describe plan ASSESMENT ANTECEDENTS TRIGGERS Medical history review and systems analysis assess the: MEDIATORS Antecedents: Sex, Age, Genetics, Lifestyle, Experiences, Trauma, Childhood, Stress, etc. Triggers: Events that initiate illness or symptoms – stress, infection, environmental toxins, food. etc. – look to see if they can be removed or controlled Mediators: Cytokines, prostaglandins, free radicals, neurotransmitters, fear, personal value, behavioural conditioning, poverty, etc. Evolutionary Nutritional Therapy • In physiology, foetal nutritional stress appears to flip an evolved switch that sets the body into a state that protects against starvation. • When these individuals encounter modern diets, they respond with the deadly metabolic syndrome of obesity, hypertension, and diabetes. • Barker DJ, Eriksson JG, Forsén T, Osmond C.Fetal origins of adult disease: strength of effects and biological basis. Int J Epidemiol. 2002 Dec;31(6):1235-9. -

(12) United States Patent (10) Patent No.: US 9,149,560 B2 Askari Et Al
USOO9149560B2 (12) United States Patent (10) Patent No.: US 9,149,560 B2 Askari et al. (45) Date of Patent: Oct. 6, 2015 (54) SOLID POLYGLYCOL-BASED 6,149,931 A 11/2000 Schwartz et al. BOCOMPATIBLE PRE-FORMULATION 6,153,211 A 11/2000 Hubbell et al. 6,180,687 B1 1/2001 Hammer et al. 6,207,772 B1 3/2001 Hatsuda et al. (71) Applicant: Medicus Biosciences LLC, San Jose, 6,312,725 B1 1 1/2001 Wallace et al. CA (US) 6,458,889 B1 10/2002 Trollsas et al. 6,475,508 B1 1 1/2002 Schwartz et al. (72) Inventors: Syed H. Askari, San Jose, CA (US); 6,547,714 B1 4/2003 Dailey 6,566,406 B1 5/2003 Pathak et al. Yeon S. Choi, Emeryville, CA (US); 6,605,294 B2 8/2003 Sawhney Paul Yu Jen Wan, Norco, CA (US) 6,624,245 B2 9, 2003 Wallace et al. 6,632.457 B1 10/2003 Sawhney (73) Assignee: Medicus Biosciences LLC, San Jose, 6,703,037 B1 3/2004 Hubbell et al. CA (US) 6,703,378 B1 3/2004 Kunzler et al. 6,818,018 B1 1 1/2004 Sawhney 7,009,343 B2 3/2006 Lim et al. (*) Notice: Subject to any disclaimer, the term of this 7,255,874 B1 8, 2007 Bobo et al. patent is extended or adjusted under 35 7,332,566 B2 2/2008 Pathak et al. U.S.C. 154(b) by 0 days. 7,553,810 B2 6/2009 Gong et al. -

Taste and Smell Disorders in Clinical Neurology
TASTE AND SMELL DISORDERS IN CLINICAL NEUROLOGY OUTLINE A. Anatomy and Physiology of the Taste and Smell System B. Quantifying Chemosensory Disturbances C. Common Neurological and Medical Disorders causing Primary Smell Impairment with Secondary Loss of Food Flavors a. Post Traumatic Anosmia b. Medications (prescribed & over the counter) c. Alcohol Abuse d. Neurodegenerative Disorders e. Multiple Sclerosis f. Migraine g. Chronic Medical Disorders (liver and kidney disease, thyroid deficiency, Diabetes). D. Common Neurological and Medical Disorders Causing a Primary Taste disorder with usually Normal Olfactory Function. a. Medications (prescribed and over the counter), b. Toxins (smoking and Radiation Treatments) c. Chronic medical Disorders ( Liver and Kidney Disease, Hypothyroidism, GERD, Diabetes,) d. Neurological Disorders( Bell’s Palsy, Stroke, MS,) e. Intubation during an emergency or for general anesthesia. E. Abnormal Smells and Tastes (Dysosmia and Dysgeusia): Diagnosis and Treatment F. Morbidity of Smell and Taste Impairment. G. Treatment of Smell and Taste Impairment (Education, Counseling ,Changes in Food Preparation) H. Role of Smell Testing in the Diagnosis of Neurodegenerative Disorders 1 BACKGROUND Disorders of taste and smell play a very important role in many neurological conditions such as; head trauma, facial and trigeminal nerve impairment, and many neurodegenerative disorders such as Alzheimer’s, Parkinson Disorders, Lewy Body Disease and Frontal Temporal Dementia. Impaired smell and taste impairs quality of life such as loss of food enjoyment, weight loss or weight gain, decreased appetite and safety concerns such as inability to smell smoke, gas, spoiled food and one’s body odor. Dysosmia and Dysgeusia are very unpleasant disorders that often accompany smell and taste impairments. -

The Effect of Vitamin Supplementation on Subclinical
molecules Review The Effect of Vitamin Supplementation on Subclinical Atherosclerosis in Patients without Manifest Cardiovascular Diseases: Never-ending Hope or Underestimated Effect? Ovidiu Mitu 1,2,* , Ioana Alexandra Cirneala 1,*, Andrada Ioana Lupsan 3, Mircea Iurciuc 4 , 5 5 2, Ivona Mitu , Daniela Cristina Dimitriu , Alexandru Dan Costache y , Antoniu Octavian Petris 1,2 and Irina Iuliana Costache 1,2 1 Department of Cardiology, Clinical Emergency Hospital “Sf. Spiridon”, 700111 Iasi, Romania 2 1st Medical Department, University of Medicine and Pharmacy “Grigore T. Popa”, 700115 Iasi, Romania 3 Department of Cardiology, University of Medicine, Pharmacy, Science and Technology, 540139 Targu Mures, Romania 4 Department of Cardiology, University of Medicine and Pharmacy “Victor Babes”, 300041 Timisoara, Romania 5 2nd Morpho-Functional Department, University of Medicine and Pharmacy “Grigore T. Popa”, 700115 Iasi, Romania * Correspondence: [email protected] (O.M.); [email protected] (I.A.C.); Tel.: +40-745-279-714 (O.M.) Medical Student, University of Medicine and Pharmacy “Grigore T. Popa”, 700115 Iasi, Romania. y Academic Editors: Raluca Maria Pop, Ada Popolo and Stefan Cristian Vesa Received: 25 March 2020; Accepted: 7 April 2020; Published: 9 April 2020 Abstract: Micronutrients, especially vitamins, play an important role in the evolution of cardiovascular diseases (CVD). It has been speculated that additional intake of vitamins may reduce the CVD burden by acting on the inflammatory and oxidative response starting from early stages of atherosclerosis, when the vascular impairment might still be reversible or, at least, slowed down. The current review assesses the role of major vitamins on subclinical atherosclerosis process and the potential clinical implications in patients without CVD. -

The Efficacy of Pantothenic Acid As a Modifier of Body Composition in a Porcine Model of Obesity Development
Iowa State University Capstones, Theses and Retrospective Theses and Dissertations Dissertations 1-1-2004 The efficacy of pantothenic acid as a modifier of body composition in a porcine model of obesity development Carey Ann Baldwin Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/rtd Recommended Citation Baldwin, Carey Ann, "The efficacy of pantothenic acid as a modifier of body composition in a porcine model of obesity development" (2004). Retrospective Theses and Dissertations. 20349. https://lib.dr.iastate.edu/rtd/20349 This Thesis is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Retrospective Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. The efficacy of pantothenic acid as a modifier of body composition in a porcine model of obesity development by Carey Ann Baldwin A thesis submitted to the graduate faculty in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE Major: Animal Nutrition Program of Study Committee: Tim Stahly, Major Professor Paul Flakoll Chad Stahl Iowa State University Ames, Iowa 2004 Copyright© Carey Ann Baldwin, 2004. All rights reserved. 11 Graduate College Iowa State University This is to certify that the master's thesis of Carey Ann Baldwin has met the thesis requirements of Iowa State University Signatures have been redacted for privacy 111 TABLE OF CONTENTS ACKNOWLEDGEMENTS Vl ABSTRACT Vll CHAPTER 1. GENERAL INTRODUCTION 1 Introduction 1 Thesis Organization 2 Literature Cited 2 CHAPTER 2. -

Molybdenum in Drinking-Water
WHO/SDE/WSH/03.04/11 English only Molybdenum in Drinking-water Background document for development of WHO Guidelines for Drinking-water Quality __________________ Originally published in Guidelines for drinking-water quality, 2nd ed. Vol. 2. Health criteria and other supporting information. World Health Organization, Geneva, 1996. © World Health Organization 2003 All rights reserved. Publications of the World Health Organization can be obtained from Marketing and Dissemination, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel: +41 22 791 2476; fax: +41 22 791 4857; email: [email protected]). Requests for permission to reproduce or translate WHO publications - whether for sale or for noncommercial distribution - should be addressed to Publications, at the above address (fax: +41 22 791 4806; email: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. The World Health Organization -

Directory of Us Bean Suppliers · Quality Grown in the Usa
US DRY DIRECTORY OF US BEAN SUPPLIERS · QUALITY GROWN IN THE USA BEANENGLISH SUPPLIERS DIRECTORY DRY BEANS FROM THE USA edn ll R ryn ma ber avyn eyn S an N idn inkn Cr K P ed R rk a D hernn yen ort cke dneyn zon N Bla Ki ban man at d ar Li e Re G ge r t ar G L h ig L ton Pin Liman ckn y Bla iman n ab y L dzuki B ab A B n e re G U.S. DRY BEANS www.usdrybeans.com International Year of the Pulse 2016 · www.iyop.net 01 n Pink Adzuki Large Lima Pink Garbanzo Dark Red Kidney Great Northern an Lim ge ar L Small Red Navy Black Baby Lima Blackeye Light Red Kidney in dzuk A Green Baby Lima Pinto Cranberry TABLE OF CONTENTS About the US Dry Bean Council 2 US Dry Bean Council Overseas Representatives 3 USDBC Members and Producers Organisations4 Major US Dry Bean Classes 6 Dry Bean Production Across the US 8 Companies by Bean Class 10 Alphabetical Listing Of US Dry Bean Suppliers 14 Nutritional Value 34 About the US Dry Bean Industry 36 USDBC Staff 37 02 ABOUT THE US DRY BEAN COUNCIL (USDBC) The USDBC is a trade association comprised of leaders in the bean industry with the common goal of educating US consumers about the benefits of beans. The USDBC gives a voice to the bean industry and provides information to consumers, health professionals, educators USDBC USA and the media about the good taste, nutritional value and Rebecca Bratter, Executive Director versatility of beans.