Bod Agenda and Papers Feb 02 2016
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chislehurst War Memorial to Swanley Station
Chislehurst war memorial to CARD Swanley station SE.D1 Start Chislehurst war memorial — BR7 5PG Finish Swanley station — BR8 8JD Distance 8.36km Duration 1 hour 50 minutes Ascent 105.2m Access Bus at start of section; train at end of section; bus at Sevenoaks Way en route Facilities Shops and pub at start of section; kiosk at end of section; shops at St Paul’s Cray en route. D1.1 Chislehurst war memorial 0m D1.2 SE on Royal Parade; beyond Bull’s Head, take path to L of road; cross Scadbury Park 3520m Dr; after 350m, L to reach open ground; E to car park; R to St Paul’s Wood Hill; R, then L down fi eld to woods; through woods and out to Leesons Way; round bend to R then L on path into copse; R on path to rec gd; L edge of gd to Chipperfi eld Rd; L to Cotmandene Cres, where R; pass shops, then ahead on Broomwood Rd to Sevenoaks Way. D1.3 Cross Sevenoaks Way; ahead on path across R Cray to Main Rd; path to L of church; 2430m R on Augustine Rd; L on Chalk Pit Ave; L on St Lawrence Close; path to R of end house; L at path jct; R on Chapman’s Lane; ahead to Hockenden Lane. D1.4 L on Hockenden Lane for 80m; R through gate onto track; follow track past scrap 2410m site; L with iron fence on R; under A20; L onto Laburnum Ave; R on Lynden Way; R on Cherry Ave; round bend and R out onto St Mary’s Rd; L, then third R (Everest Pl) to rly; R into stn. -

TRADES. FR'c 1045 Lftred William, Crocken Hill, Swan- Ingarfill John, Knockholt, Sevenoaks Osmer Jn
KENT.) TRADES. FR'C 1045 lftred William, Crocken Hill, Swan- Ingarfill John, Knockholt, Sevenoaks Osmer Jn. jun. Snnnyside, Marden ley Junction Inge Harry, Brook Street farm, Ash, Ounstead Wm. Halstead, Sevenoaks Fielder Harry, Ivy Hatch, Sevenoaks Canterbury Pa.ckham Alfred, Dungate house, Rod- Fielder W. Ivy Hatch, Sevenoaks Jackson Henry & Sons, Hockenden, mersham, Sittingbourne Fill~ess H. Hockenden, St.Mary Cray St. Mary Cray Pain Arnold E. Blackball fm.Svnoaks Foat Thomas, Copp st.Ash,Canterbry Jenner John, Ivy Hatch, Sevenoaks Palmer James Ebenezer, Northumber Foreman Robert, Well hill, Chels- Johnston Alexander, Falcon farm, land house, Colyer's lane, Erit.h field, Orpington Leaveland, Faversham Parsons Benjamin, Vale house, Stock Fowler E. & S. Ulcombe. Maidstone Jordan Percy, !stead rise, Gravesend bury, Si~ingbourne l'rappell Hy.Westerham ID.Westerhm Kearn Arthur, 'l'he Heath, Wilming Parsons Miss Mary, Wilmington, Pry John, Twydale, Gillingham ton, Dartford Dartford k at Stone, Dartford Farner George, Slades green, Erith Keene W. Sole Street, Gravesend Payne William, Pearmaine, Swanley, Gardner H. R. Basted, Platt, Borough Kemp William, Chestnut Street, Swanley Junction Green Borden, Sittingbourne Peckham Mrs.M.Ivy Hatch, Sevenoab Gllbert D. A. Farnborough,Orpington Kemsley Henry, Bredgar, Sittingbrne Pepper Thomas John, Groves, Staple, Gilbert Mrs. Esther, sr Upper Abbey Kitchingham Frank, Bean, Dartford Canterbury road, Belvedere Knell Henry, Broomfield, Maidstone Peto Wm. Bedonwell hill, Belvedere Gillow Fredk. Ivor ho. Worth, Eastry Knight Thomas, Bargain's hill, Rod- Plumbridge Edward & Arthur, Farn Goldin~ Chas. E. William st.Rainhm mersham, Sittingbourne borough, Orpington Goodchild F. Farnborough, Orpington Kno1Vles William, Charlton house, Pollock J rum Stanley Hope, Overs Goodchild John, FarnborQ', Orpington Bapchild, Sittingbourne land, South Street, Faversham Goodchild R. -

The Owl Prowl Continues!
The Owl Prowl Continues! Report of Pilot Survey A tawny owl survey was carried out this autumn in the London Borough of Bromley under the leadership of Bromley Biodiversity Partnership, in particular by Bill Whitaker of the OFC. 59 records were submitted by 33 people from many parts of the borough. Tawny owls were recorded in about 17 areas: High Elms & the Cudham Valley, Darrick Wood area, Marvels & Elmstead Woods, between Elmstead Wood and Chislehurst & Walden Road Recreation Ground, between Chislehurst & Walden Road Recreation Ground & Chislehurst Golf Course, Chislehurst Golf Course itself, Old Hill/Lubbock Road area, Chislehurst, Sundridge Park, Kemnal Road, Chislehurst, the St Pauls Cray Road area, Hawkwood Estate/Petts Wood, Scadbury Park, Hayes, near Bromley South, Kelsey Park, Beckenham, Crofton Woods and south of Biggin Hill. The records clearly show recording effort, with no records for several areas where owls are very likely to be present such as West Wickham and Keston Commons and hardly any records for areas of open countryside to the south and east of the borough where fewer people live. The almost complete lack of records from these areas and the peripheral wards of LBB to the east, south east, south and south west are also likely to be due in part to the fact that we were unable to communicate effectively with residents in these areas before the survey commenced. Within the larger areas where recordings were submitted there are probably several tawny owl territories, for example within High Elms Country Park and along the Cudham Valley. In well populated areas, for example within Chislehurst, there is likely to be some duplication of records, but the large number of tawny owl records for Chislehurst and its surroundings (Chislehurst Common, Chislehurst Golf Course, Petts Wood, Scadbury Park, Elmstead and Marvels Wood, Sundridge Park and Chislehurst & Walden Road Recreation Ground, together with gardens between), may also reflect the importance of good connectivity between areas rich in biodiversity within an urban area. -

Star Lane Appendix , Item 3B PDF 222 KB
The Planes Hockenden Drain 47.0m Drain Hockenden KEYS: Lower Hockenden Farm HIGH SECURITY DROP BOLLARDS FLANKED BY 2 TONNE CONCRETE BOLLARDS WITH 'ROAD CLOSED' SIGNS 4 Drain 1 RETENTION OF CONCRETE BLOCKS WITH 'ROAD CLOSED' SIGNS Little Hockenden Hill Park House Cottages ROAD CLOSED SIGNS Hockenden House Path (um) HOCKENDEN LANE Path (um) HOCKENDEN LANE St Paul's Cray Hill Park Path (um) STAR LANE 1 Hogspringville Hogspringville Stables 2 Highlands Wood STAR LANE LANE Path (um) STAR Track Milewood Caravan Site Track 47.3m Path (um) Mast Brockenhurst Track El Sub Sta SHEEPCOTE LANE STAR LANE Hockenden Wood 10 Appendix A 11 SHEEPCOTE LANE Travellers Site 18 Path STAR LANE 48.6m El Sub Sta 71.9m St Mary Cray Cemetery STAR LANE 58.6m MP 15.75 SL MP 16.25 51 SLs CHESTERFIELD CLOSE SL MP 16.5 SL 63 24 SL SWEEPS LANE Track SWEEPS LANE SHEEPCOTE LANE Track Und 68.2m LANE SWEEPS (um) Path This drawing has been produced by and is the property of the London Borough of Bromley. No responsibility will be accepted by the Council for any unauthorised use of drawings or documents by a third party. Sheepcote Farmhouse NOTE: DO NOT SCALE OFF THIS DRAWING. Path (um) © Crown copyright and database rights 2020 Ordnance Survey 100017661. Job Title: Drawing Title: Environment & Public Protection Scale @ A1: Civic Centre, Stockwell Close, N.T.S. Bromley, BR1 3UH STAR LANE, ORPINGTON PROPOSED PERMANENT CLOSURE OF STAR LANE, ST. MARY CRAY Date: Tel : 020 8464 - 3333 12/06/20 FROM THE JUNCTION OF SWEEPS LANE TO SHEEPCOTE LANE Fax : 020 8313 - 4555 Email : www.bromley.gov.uk Drawn by: By Colin Brand N J.J. -

London Borough of Bromley Progress Report 2008 Air Quality London
London Borough of Bromley Progress Report 2008 Air Quality London Borough of Bromley June 2008 Table of Contents 1 Introduction ..................................................................................................................... 2 1.1 Introduction ........................................................................................................... 2 1.2 Legislative Background......................................................................................... 2 1.3 The Phased Approach to Review and Assessment ............................................. 2 1.4 The Role of the Progress Report .......................................................................... 2 2 The National Air Quality Strategy.................................................................................. 3 2.1 Introduction ........................................................................................................... 3 2.2 Nitrogen Dioxide ................................................................................................... 3 2.3 Particulate Matter.................................................................................................. 7 3 Local Air Quality Monitoring.......................................................................................... 9 3.1 The London Borough of Bromley.......................................................................... 9 3.2 Local Air Quality Management in the London Borough of Bromley...................... 9 3.3 Air Quality Management Areas............................................................................ -

Applications and Decisions: London and the South East of England
OFFICE OF THE TRAFFIC COMMISSIONER (LONDON AND THE SOUTH EAST OF ENGLAND) APPLICATIONS AND DECISIONS PUBLICATION NUMBER: 3949 PUBLICATION DATE: 10 December 2015 OBJECTION DEADLINE DATE: 31 December 2015 Correspondence should be addressed to: Office of the Traffic Commissioner (London and the South East of England) Hillcrest House 386 Harehills Lane Leeds LS9 6NF Telephone: 0300 123 9000 Fax: 0113 248 8521 Website: www.gov.uk/traffic-commissioners The public counter at the above office is open from 9.30am to 4pm Monday to Friday Please note: the Central Licensing Office public counter at Hillcrest House will close at 2pm on Christmas Eve (24 Dec 2015). The office is also closed all day Christmas Day, Boxing Day and New Years Day ’s. The next edition of Applications and Decisions will be published on: 24/12/2015 Publication Price 60 pence (post free) This publication can be viewed by visiting our website at the above address. It is also available, free of charge, via e-mail. To use this service please send an e-mail with your details to: [email protected] APPLICATIONS AND DECISIONS Important Information All correspondence relating to public inquiries should be sent to: Office of the Traffic Commissioner (London and the South East of England) Ivy House 3 Ivy Terrace Eastbourne BN21 4QT The public counter in Eastbourne is open for the receipt of documents between 9.30am and 4pm Monday to Friday. There is no facility to make payments of any sort at the counter. General Notes Layout and presentation – Entries in each section (other than in section 5) are listed in alphabetical order. -
The London Gazette, 24 August, 1923. 5771
THE LONDON GAZETTE, 24 AUGUST, 1923. 5771 Urban District of Orayford. .(13) Crofton Boad, Orpington, from the (8) High Street from Dover Boad to road junction near Crofton Grange via Church Hill. Crofton Court and Clay Farm to its junction at Covert Corner with Chislehurst Boad. Urban District of Sheerness. (14) Poverest Boad from Chislehurst (24) Trinity Boad from the junction with Boad to its junction with Lower Boad, St. Strode Crescent, Cavour Eoad and Albert Mary Cray. Street. (15) (a) Cockmannings Boad and Water- Urban District of Whitstable. pit Lane from the road junction at Grigg's (50) Sea Street and Harbour Street. Cross via Cockmannings Corner and Waterpit Wood to the junction with the Rural District of Blean. St. Mary Cray-Crockenhill road at Keving- (51) Eoad from St. Stephen's Eoad at town. the boundary of the Borough of Canterbury (15) (b) Sheepcote Lane and Hockenden via the Brick Works, Broadoak Crossing, Lane from the St. Mary Cray-Crockenhill and the Smithy, Broadoak, to its junction road to the junction with the Sidcup- near Sweech Farm with the Herne Bay- Farningham road, at Birchwood Corner. Sturry road. (15) (c) Star Lane and Cemetery Boad (52) Eoad from the Henie Bay-Sturry from Hockenden Lane to the junction with road near West Blean House via Hicks .the St. Paul's Cray-St. Mary Cray road near Forstal Wood and East Blean Wood to its St. Mary's Church. junction at Knave's Ash with the Maypole- (16) (a) Boad from the Bromley-Seven- Sturry road, and from that junction via oaks road at Green Street Green via Den- Hoath and Chislet Forstal to the road barn, Hostye Farm, Cudham, Horns Green, junction near the Vicarage, Hollow Street, Scott's Lodge and Cudham Grange to the including the following branches: — road junction at Hawley's Comer. -

Lower North Downs Dip Slope
21. Lower North Downs Dip Slope Key plan Description The Lower North Downs Dip Slope Natural Landscape Area includes parts of the boroughs of Sutton, Croydon, Bromley and Bexley, stretching east–west along the North Downs, north of the Wooded Chalk Slopes (NLA 22) and south of the South London Clays and Gravels (NLA 17) and the South London Pebbly Sands (NLA 19). This is the lower dip slope of the North Downs and the land rises gently to the south. The upper reaches of the Wandle, Ravensbourne and Cray rivers have cut down through the chalk bedrock to form a series of ridges and valleys along the slope. The areas underlain by chalk have ENGLAND 100046223 2009 RESERVED ALL RIGHTS NATURAL CROWN COPYRIGHT. © OS BASE MAP the distinctive concave-convex rolling relief of chalk uplands, with dry 21. Lower North Downs Dip Slope valleys and broad, rounded ridges. The dip slope is formed from the tilted chalk strata (Lewes Nodular, Purley, where the settlement core of Victorian terraces is built around Seaford and Newhaven Chalk formations) of the North Downs ridge the confluence of tributaries of the River Wandle and several railways. 21. Lower North Downs Dip Slope Dip Downs North Lower 21. which runs east west to form the southern rim of the London Basin. There are areas of fragmented and intense modern residential The chalk continues below all of the London area. There are London development in Selsdon/Forestdale, east Orpington and at South Clays and older rocks of the Harwich Formation on the northern Beddington. Open spaces are typically situated on the slopes of the fringes of the chalk dip slope. -
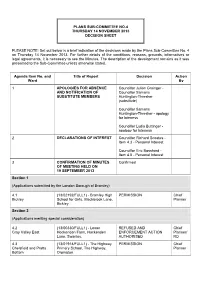
PLEASE NOTE: Set out Below Is a Brief Indication of the Decisions Made by the Plans Sub-Committee No
PLANS SUB-COMMITTEE NO.4 THURSDAY 14 NOVEMBER 2013 DECISION SHEET PLEASE NOTE: Set out below is a brief indication of the decisions made by the Plans Sub-Committee No. 4 on Thursday 14 November 2013. For further details of the conditions, reasons, grounds, informatives or legal agreements, it is necessary to see the Minutes. The description of the development remains as it was presented to the Sub-Committee unless otherwise stated. Agenda Item No. and Title of Report Decision Action Ward By 1 APOLOGIES FOR ABSENCE Councillor Julian Grainger - AND NOTIFICATION OF Councillor Samaris SUBSTITUTE MEMBERS Huntington-Thresher (substitute) Councillor Samaris Huntington-Thresher - apology for lateness Councillor Lydia Buttinger - apology for lateness 2 DECLARATIONS OF INTEREST Councillor Richard Scoates - Item 4.3 - Personal Interest Councillor Eric Bosshard - Item 4.5 - Personal Interest 3 CONFIRMATION OF MINUTES Confirmed OF MEETING HELD ON 19 SEPTEMBER 2013 Section 1 (Applications submitted by the London Borough of Bromley) 4.1 (13/02192/FULL1) - Bromley High PERMISSION Chief Bickley School for Girls, Blackbrook Lane, Planner Bickley. Section 2 (Applications meriting special consideration) 4.2 (13/00330/FULL1) - Lower REFUSED AND Chief Cray Valley East Hockenden Farm, Hockenden ENFORCEMENT ACTION Planner/ Lane, Swanley. AUTHORISED RD 4.3 (13/01914/FULL1) - The Highway PERMISSION Chief Chelsfield and Pratts Primary School, The Highway, Planner Bottom Orpington. London Borough of Bromley – Decisions taken by Plans Sub-Committee No. 4 on Thursday 14 November 2013 Agenda Item No. and Title of Report Decision Action Ward By 4.4 (13/02042/FULL2) - Kennedy PERMISSION Chief Cray Valley West House, Murray Road, Orpington. -

Bournewood Sand and Gravel, Swanley Bypass
Committee Date 28/01/20 Bournewood Sand And Gravel Address Swanley Bypass Swanley BR8 7FL Application 17/01564 Officer Paul Mellor number Cray Valley East Ward Proposal Variation of Condition 1 of planning permission ref. 10/00657/VAR (Summary) (allowed at appeal under PINS ref. APP/G5180/A/11/2145860) to permit continued extraction of Thanet Sand until 31st March 2020 and restoration and recontouring with inert waste until 14th January 2021, with associated access, buildings and structures to remain until 14th January 2021. Applicant Agent Killoughery Waste Management Ltd Miss Maureen Darrie The Stables 43A Willow Lane Long Lane Mitcham East Haddon CR4 4NA Northampton NN6 8DU Reason for Councillor call in referral to committee Call-in Yes RECOMMENDATION PERMISSION KEY DESIGNATIONS Biggin Hill Safeguarding Area Green Belt London City Airport Safeguarding Sites of Interest for Nat. Conservation Smoke Control SCA 20 Land use Details Use Class or Use Floor space (GIA SQM) description Existing Sui generis – mineral Sui generis – mineral extraction extraction Proposed Sui generis – mineral Sui generis – mineral extraction extraction Representation summary Neighbour letters were sent on 23.6.17 and again on 3.10.19. A site notice was displayed on 20.6.17 A press advert was published on 19.7.17 Total number of responses 7 Number in support 0 Number of objections 5 1. SUMMARY OF KEY REASONS FOR RECOMMENDATION The development would not impact detrimentally on the openness and visual amenity of the Green Belt. The proposal would provide an economically viable and satisfactory solution to the completion of mineral extraction at the site and its subsequent restoration. -

Butterflies of London Atlas Project
Butterflies of London Atlas Project 7th April 2018 Welcome to this London Natural History Society project working with other organisations and individuals in London. Thank you for all the records to date. While the project is collating the records from the survey to date, recording is continuing into 2018. Weather during the springs of both 2017 and 2016 had considerable periods of either cold or wet weather which were not conducive to butterfly flight. Records of any butterflies, are welcome – and see also the box below. As before, records from less well visited locations help to build a picture of distribution. Records are particularly sought of: Species Notes Time guide Orange Tip Occurs in low numbers Spring: April and May wandering along hedges, watercourses and other habitats. Seeks Ladies Smock and Hedge Garlic for egg laying; Cow Parsley for roosting; and shrubs for protection. The males are unmistakable; the females are less conspicuous and fly less. Brimstone The fluorescent yellow of the Spring mainly. There can be male is easily recognisable. a second generation in about Females are a whitish-green. August. At rest the intricate wing and vein pattern looks like a leaf. Comma, Peacock, Small Widespread. Easy to Over-wintering adults may Tortoiseshell, Red Admiral identify. emerge in the spring; and subsequent generations may be seen at times during the spring, summer and autumn. Most butterfly records are of adults, while records of eggs and young stages are equally valuable. Species that over-winter as adults may be encountered hibernating in sheds, out-buildings, or deep in vegetation. -

Bromley District
BROMLEY DISTRICT. PARISH OF BECKENHAM. H D A Bl.* Adams, Edward R., 2, Old Square, Lincoln’ s Inn, London 471, did not vote Bl.* Allbrook, J. B., 1, St, James’s-ter., Lower Clapton, N.E. 476, A.L............... 1130 Barry, Ai red, Elmstone House, Beckenham, K ent......................................... 1131 Barry, Francis Tress, The Clock-house, Beckenham............................................. 1132 Bicknell, Percy, Beckenham. S.E...................... .................................................. 1133 Borrowman, John, Elm Cottage, Beckenham, Kent.......................................... 1134 Bowden, Richard Callow, Clapham-common, Surrey............................................ 1135 Brooksbank, Thomas, Penge Lane, Sydenham.... .......................................... Bl.* Butterworih, J. W ., Grove Lodge, Clapham Cora.,Clapham,Surrey, 568 H.D 1136 Caird, Janies, M,P., Cassencary, Cretown, N.B......................... .......................... 1137 Color, Albemarle, Wood Bast wick-hall, near Norwich......................................... 1138 Cgtor, Albemarle, jun , Wood Bastwick Hall, near Norwich.................... ... 1139 Cator, Peter Bertie, Ilolyrood House, Beckenham............................................ 1140 Cator, Peter, Beckenham...................................................................................... 1141 Cator, William, 6, Eaton Place, London .......................................................... 1142 Chalmers, Rev. Frederick Skene Courtnay, Beckenham........................................