Basic Concepts in Drug Addiction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nightshade”—A Hierarchical Classification Approach to T Identification of Hallucinogenic Solanaceae Spp
Talanta 204 (2019) 739–746 Contents lists available at ScienceDirect Talanta journal homepage: www.elsevier.com/locate/talanta Call it a “nightshade”—A hierarchical classification approach to T identification of hallucinogenic Solanaceae spp. using DART-HRMS-derived chemical signatures ∗ Samira Beyramysoltan, Nana-Hawwa Abdul-Rahman, Rabi A. Musah Department of Chemistry, State University of New York at Albany, 1400 Washington Ave, Albany, NY, 12222, USA ARTICLE INFO ABSTRACT Keywords: Plants that produce atropine and scopolamine fall under several genera within the nightshade family. Both Hierarchical classification atropine and scopolamine are used clinically, but they are also important in a forensics context because they are Psychoactive plants abused recreationally for their psychoactive properties. The accurate species attribution of these plants, which Seed species identifiction are related taxonomically, and which all contain the same characteristic biomarkers, is a challenging problem in Metabolome profiling both forensics and horticulture, as the plants are not only mind-altering, but are also important in landscaping as Direct analysis in real time-mass spectrometry ornamentals. Ambient ionization mass spectrometry in combination with a hierarchical classification workflow Chemometrics is shown to enable species identification of these plants. The hierarchical classification simplifies the classifi- cation problem to primarily consider the subset of models that account for the hierarchy taxonomy, instead of having it be based on discrimination between species using a single flat classification model. Accordingly, the seeds of 24 nightshade plant species spanning 5 genera (i.e. Atropa, Brugmansia, Datura, Hyocyamus and Mandragora), were analyzed by direct analysis in real time-high resolution mass spectrometry (DART-HRMS) with minimal sample preparation required. -

The Mandrake and the Ancient World,” the Evangelical Quarterly 28.2 (1956): 87-92
R.K. Harrison, “The Mandrake And The Ancient World,” The Evangelical Quarterly 28.2 (1956): 87-92. The Mandrake and the Ancient World R.K. Harrison [p.87] Professor Harrison, of the Department of Old Testament in Huron College, University of Western Ontario, has already shown by articles in THE EVANGELICAL QUARTERLY his interest and competence in the natural history of the Bible. Here he examines one of the more curious Biblical plants. The mandrake is one of the plants which still grows widely in the Middle East, and which has claimed magical associations from a very remote period. It is generally assigned the botanical name of Mandragora officinarum L..1 and is a perennial of the order Solanaceae. It claims affinity with the potato and eggplant, and is closely allied to the Atropa belladonna L.,2 with which it is not infrequently confused by some writers. The modern Arab knows it by a number of names, including Tuffah£ el Majanin (‘Madmen’s Apple) and Beid el Jinn (Eggs of the Jinn), apparently a reference to the ability of the plant to invigorate and stimulate the senses even to the point of mental imbalance. The former name may perhaps be a survival of the belief found in Oriental folk-lore regarding the magical herb Baaras, with which the mandrake is identified by some authorities.3 According to the legends associated with this plant, it was highly esteemed amongst the ancients on account of its pronounced magical properties. But because of the potency of these attributes it was an extremely hazardous undertaking for anyone to gather the plant, and many who attempted it were supposed to have paid for their daring with [p.88] sickness and death.4 Once the herb had been gathered, however, it availed for a number of diseases, and in antiquity it was most reputed for its ability to cure depression and general disorders of the mind. -

Inventory of Toxic Plants in Morocco: an Overview of the Botanical, Biogeography, and Phytochemistry Studies
Hindawi Journal of Toxicology Volume 2018, Article ID 4563735, 13 pages https://doi.org/10.1155/2018/4563735 Review Article Inventory of Toxic Plants in Morocco: An Overview of the Botanical, Biogeography, and Phytochemistry Studies Hanane Benzeid , Fadma Gouaz, Abba Hamadoun Touré, Mustapha Bouatia , Mohamed Oulad Bouyahya Idrissi, and Mustapha Draoui LaboratoiredeChimieAnalytiqueetdeBromatologie,FacultedeM´ edecine´ et de Pharmacie, Universite´ Mohamed V, Rabat, Morocco Correspondence should be addressed to Hanane Benzeid; [email protected] Received 10 December 2017; Revised 22 February 2018; Accepted 25 March 2018; Published 3 May 2018 Academic Editor: Orish Ebere Orisakwe Copyright © 2018 Hanane Benzeid et al. Tis is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Since they are natural, plants are wrongly considered nondangerous; therefore people used them in various contexts. Each plant is used alone or in mixture with others, where knowledge and the requirements of preparation and consumption are not mastered. Tus, intoxications due to the use of plants have become more and more frequent. Te reports of intoxications made at the Antipoison Center and Pharmacovigilance of Morocco (ACPM) support this fnding, since the interrogations sufered by the victimsshowthattheuseofplantsispracticedirrationally,anarchically, and uncontrollably. Faced by the increase of these cases of poisoning in Morocco, it seemed necessary to investigate the nature of poisonous plants, their monographs, and the chemicals responsible for this toxicity. 1. Introduction Tus, we thought it is necessary to study the nature of these poisonous plants and their monographs. Sinceimmemorialtime,thehumanhasusedplants,frstto feed himself and then to heal himself. -

Feasibility Study of Kailash Sacred Landscape
Kailash Sacred Landscape Conservation Initiative Feasability Assessment Report - Nepal Central Department of Botany Tribhuvan University, Kirtipur, Nepal June 2010 Contributors, Advisors, Consultants Core group contributors • Chaudhary, Ram P., Professor, Central Department of Botany, Tribhuvan University; National Coordinator, KSLCI-Nepal • Shrestha, Krishna K., Head, Central Department of Botany • Jha, Pramod K., Professor, Central Department of Botany • Bhatta, Kuber P., Consultant, Kailash Sacred Landscape Project, Nepal Contributors • Acharya, M., Department of Forest, Ministry of Forests and Soil Conservation (MFSC) • Bajracharya, B., International Centre for Integrated Mountain Development (ICIMOD) • Basnet, G., Independent Consultant, Environmental Anthropologist • Basnet, T., Tribhuvan University • Belbase, N., Legal expert • Bhatta, S., Department of National Park and Wildlife Conservation • Bhusal, Y. R. Secretary, Ministry of Forest and Soil Conservation • Das, A. N., Ministry of Forest and Soil Conservation • Ghimire, S. K., Tribhuvan University • Joshi, S. P., Ministry of Forest and Soil Conservation • Khanal, S., Independent Contributor • Maharjan, R., Department of Forest • Paudel, K. C., Department of Plant Resources • Rajbhandari, K.R., Expert, Plant Biodiversity • Rimal, S., Ministry of Forest and Soil Conservation • Sah, R.N., Department of Forest • Sharma, K., Department of Hydrology • Shrestha, S. M., Department of Forest • Siwakoti, M., Tribhuvan University • Upadhyaya, M.P., National Agricultural Research Council -

Katharine House Hospice Drug Policy
KATHARINE HOUSE HOSPICE DRUG POLICY 5th EDITION Approved by: Date of Approval: Originator: Medical Director Ref: BR/Policies/Drug Revision: 4 Approved: Page 1 of 108. Revision due by: KATHARINE HOUSE HOSPICE Preface The use of drugs is an essential part of Palliative Care, but drugs are potentially dangerous if used without due care and attention. This Drug Policy collates a range of policy and multiple drug- related procedures into one document in a way that is intended to minimise the risk of drug- related harm at Katharine House Hospice. Because of the interrelatedness of much of this information, the document is extensively cross-referenced. However, every effort has been taken to make each separate section complete in itself and, in order to achieve this, certain key points may have been repeated in different parts of the document. This Policy has taken account of all appropriate pieces of national legislation. Every relevant standard in the Department of Health National Minimum Standards for Independent Health Care 2002 has also been considered in drawing up this policy, as well as all pertinent advice contained in any correspondence we have had with the HealthCare Commission. Guidance from a range of advisory bodies has also been considered. The hospice is now regulated by the Care Quality Commission. However, reference is still deliberately made to the now defunct Health Care Commission when this specifically relates to correspondence with that organisation that helped to clarify aspects of hospice policy and procedure. A number of in-house procedures and clinical guidelines supplement the Drugs Policy. These include: • Procedure for the Procurement, Handling and Storage of Oxygen Cylinders (Clinical Policies Folder). -

Finland Country Drug Report 2017
Finland Country Drug Report 2017 Contents: At a glance | National drug strategy and coordination (p. 2) | Public expenditure (p. 3) | Drug laws and drug law offences (p. 4) | Drug use (p. 5) | Drug harms (p. 8) | Prevention (p. 10) | Harm reduction (p. 11) | Treatment (p. 12) | Drug use and responses in prison (p. 14) | Quality assurance (p. 15) | Drug-related research (p. 15) | Drug markets (p. 16) | Key drug statistics for Finland (p. 18) | EU Dashboard (p. 20) THE DRUG PROBLEM IN FINLAND AT A GLANCE Drug use Treatment entrants Overdose deaths Drug law offences in young adults (15-34 years) by primary drug in the last year 250 Cannabis 200 23 478 166 150 13.5 % Top 5 drugs seized 100 ranked according to quantities Cannabis, 21% 50 measured in kilograms Amphetamines, 15 % Cocaine, 0 % 0 1. Amphetamine 2011 2012 2013 2015 2014 Opioids, 52 % 2010 2007 2008 2006 9 % 17.9 % 2009 Other, 12 % 2. Herbal cannabis Other drugs Opioid substitution HIV diagnoses 3. Cannabis resin MDMA 2.5 % treatment clients attributed to injecting 4. Cocaine Amphetamines 2.4 % 14 5. Heroin Cocaine 1 % 12 3 000 10 Population 8 (15-64 years) 6 7 High-risk opioid users Syringes distributeddistributed 4 through specialised 2 3 483 757 programmes 0 13 836 2011 2012 2013 2015 2014 2010 2007 2008 2006 2009 Source: EUROSTAT (12 700 - 15 090) 5 301 000 Source: ECDC Extracted on: 26/03/2017 NB: Data presented here are either national estimates (prevalence of use, opioid drug users) or reported numbers through the EMCDDA indicators (treatment clients, syringes, deaths and HIV diagnosis, drug law offences and seizures). -

PSYCHEDELIC DRUGS (P.L) 1. Terminology “Hallucinogens
PSYCHEDELIC DRUGS (p.l) 1. Terminology “hallucinogens” – induce hallucinations, although sensory distortions are more common “psychotomimetics” – to minic psychotic states, although truly most drugs in this class do not do so “phantasticums”or “psychedelics” – alter sensory perception (Julien uses “psychedelics”) alterations in perception, cognition, and mood, in presence of otherwise clear ability to sense” may increase sensory awareness, increase clarity, decrease control over what is sensed/experienced “self-A” may feel a passive observer of what “self-B” is experiencing often accompanied by a sense of profound meaningfulness, of divine or cosmic importance (limbic system?) these drugs can be classified by what NT they mimic: anti-ACh, agonists for NE, 5HT, or glutamate (See p. 332, Table 12.l in Julien, 9th Ed.) 2. The Anti-ACh Psychedelics e.g. scopolamine (classified as an ACh blocker) high affinity, no efficacy plant product: Belladonna or “deadly nightshade” (Atropa belladonna) Datura stramonium (jimson weed, stinkweed) Mandragora officinarum (mandrake plant) pupillary dilation (2nd to atropine) PSYCHEDELIC DRUGS (p.2) 2. Anti-ACh Psychedelics (cont.) pharmacological effects: e.g. scopolamine (Donnatal) clinically used to tx motion sickness, relax smooth muscles (gastric cramping), mild sedation/anesthetic effect PNS effects --- dry mouth relaxation of smooth muscles decreased sweating increased body temperature blurred vision dry skin pupillary dilation tachycardia, increased BP CNS effects --- drowsiness, mild euphoria profound amnesia fatigue decreased attention, focus delirium, mental confusion decreased REM sleep no increase in sensory awareness as dose increases --- restlessness, excitement, hallucinations, euphoria, disorientation at toxic dose levels --- “psychotic delirium”, confusion, stupor, coma, respiratory depression so drug is really an intoxicant, amnestic, and deliriant 3. -

The Phytochemistry of Cherokee Aromatic Medicinal Plants
medicines Review The Phytochemistry of Cherokee Aromatic Medicinal Plants William N. Setzer 1,2 1 Department of Chemistry, University of Alabama in Huntsville, Huntsville, AL 35899, USA; [email protected]; Tel.: +1-256-824-6519 2 Aromatic Plant Research Center, 230 N 1200 E, Suite 102, Lehi, UT 84043, USA Received: 25 October 2018; Accepted: 8 November 2018; Published: 12 November 2018 Abstract: Background: Native Americans have had a rich ethnobotanical heritage for treating diseases, ailments, and injuries. Cherokee traditional medicine has provided numerous aromatic and medicinal plants that not only were used by the Cherokee people, but were also adopted for use by European settlers in North America. Methods: The aim of this review was to examine the Cherokee ethnobotanical literature and the published phytochemical investigations on Cherokee medicinal plants and to correlate phytochemical constituents with traditional uses and biological activities. Results: Several Cherokee medicinal plants are still in use today as herbal medicines, including, for example, yarrow (Achillea millefolium), black cohosh (Cimicifuga racemosa), American ginseng (Panax quinquefolius), and blue skullcap (Scutellaria lateriflora). This review presents a summary of the traditional uses, phytochemical constituents, and biological activities of Cherokee aromatic and medicinal plants. Conclusions: The list is not complete, however, as there is still much work needed in phytochemical investigation and pharmacological evaluation of many traditional herbal medicines. Keywords: Cherokee; Native American; traditional herbal medicine; chemical constituents; pharmacology 1. Introduction Natural products have been an important source of medicinal agents throughout history and modern medicine continues to rely on traditional knowledge for treatment of human maladies [1]. Traditional medicines such as Traditional Chinese Medicine [2], Ayurvedic [3], and medicinal plants from Latin America [4] have proven to be rich resources of biologically active compounds and potential new drugs. -

Cordyceps Medicinal Fungus: Harvest and Use in Tibet
HerbalGram 83 • August – October 2009 83 • August HerbalGram Kew’s 250th Anniversary • Reviving Graeco-Arabic Medicine • St. John’s Wort and Birth Control The Journal of the American Botanical Council Number 83 | August – October 2009 Kew’s 250th Anniversary • Reviving Graeco-Arabic Medicine • Lemongrass for Oral Thrush • Hibiscus for Blood Pressure • St. John’s Wort and BirthWort Control • St. John’s Blood Pressure • HibiscusThrush for Oral for 250th Anniversary Medicine • Reviving Graeco-Arabic • Lemongrass Kew’s US/CAN $6.95 Cordyceps Medicinal Fungus: www.herbalgram.org Harvest and Use in Tibet www.herbalgram.org www.herbalgram.org 2009 HerbalGram 83 | 1 STILL HERBAL AFTER ALL THESE YEARS Celebrating 30 Years of Supporting America’s Health The year 2009 marks Herb Pharm’s 30th anniversary as a leading producer and distributor of therapeutic herbal extracts. During this time we have continually emphasized the importance of using the best quality certified organically cultivated and sustainably-wildcrafted herbs to produce our herbal healthcare products. This is why we created the “Pharm Farm” – our certified organic herb farm, and the “Plant Plant” – our modern, FDA-audited production facility. It is here that we integrate the centuries-old, time-proven knowledge and wisdom of traditional herbal medicine with the herbal sciences and technology of the 21st Century. Equally important, Herb Pharm has taken a leadership role in social and environmental responsibility through projects like our use of the Blue Sky renewable energy program, our farm’s streams and Supporting America’s Health creeks conservation program, and the Botanical Sanctuary program Since 1979 whereby we research and develop practical methods for the conser- vation and organic cultivation of endangered wild medicinal herbs. -

Common Poisonous Plants in Sri Lanka
COMMON POISONOUS PLANTS IN SRI LANKA ATHTHNA (THORN APPLE) Most poisonous flowers/ stem/ fruit/ leaves/roots Fatal dose: 50-75 seeds Botanical Name: Datura stramonium Toxin: Belladonna alkaloids (atropine, hyoscine and hyoscyamine) CIRCUMSTANCES OF DATURA POISONING Stupefying purpose Mixed with cigarettes produce state of unconsciousness to facilitate robbery & rape mixed with sweets (gingerly) robbery & rape Accidental poisoning: Children Suicidal Homicidal : very rare DATURA POISONING SIGNS & SYMPTOMS Produce characteristic manifestations of anticholinergic poisoning Dryness of mouth Autopsy findings Dysphagia Seeds in stomach & non specific Dysarthria features Diplopia Dry hot and red skin Drowsiness leading to coma Urinary retention Death : respiratory failure or cardiac arrhythmia DIVI KADURU (EVE’S APPLE) Most poisonous / latex/ fruit/ seeds Botanical Name: Pagiy antha dicotoma Botanical Name: Tabernaemanta dicotoma Toxin: alkaloids/ strychnine SIGNS & SYMPTOMS OF DIVI KADURU POISONING White latex : inflammation of eye Ingestion : dryness of mucus membranes, thirst, dilataiton of pupils, rapid pulse, psychomotor disturbances, hallucinogenic effects. Autopsy findings Accidental poisonin g: Children Seeds in stomach & non specific Suicidal poisoning features GODA KADURU (BITTER NUT) Most poisonous: Seed (although all parts toxics) Fatal dose: 1-2 seeds Botanical Name: Strychnos nux vomica Toxin: alkaloids ( strychnine/ brucine) CIRCUMSTANCES OF GODA KADURU POISONING Strychnine injections are used to kill stray dogs/ -

Downloaded from by Pediatricsguest on October Vol.3, 2021 109 No
Just a Click Away: Recreational Drug Web Sites on the Internet Paul M. Wax, MD ABSTRACT. The explosive growth of the Internet in sharp rise in MDMA use among college students as recent years has provided a revolutionary new means of well.3 The report of the Drug Abuse Warning Net- interpersonal communication and connectivity. Informa- work released in December 2000 reveals that emer- tion on recreational drugs—once limited to bookstores, gency department (ED) episodes related to MDMA, libraries, mass media, and personal contacts—is now GHB, and ketamine increased significantly during readily available to just about anyone with Internet ac- 4 cess. Not surprising, Internet access greatly facilitates the the period 1994 to 1999. In addition, abuse of some free and easy exchange of ideas, opinions, and unedited older drugs, such as dextromethorphan, seems to be 5 and nonrefereed information about recreational drugs. on the upsurge. This article presents a patient who came to medical at- Simultaneous with this “club” drug revolution has tention as the result of recreational drug-taking behavior been the explosive growth of the Internet. A dra- directly influenced by her Internet browsing. A second matic change in the everyday means of communica- case is presented in which the only information available tions has taken place. E-mail is now ubiquitous, and about the medical effects of a new “designer” drug was the World Wide Web, known as the Internet, brings found on a recreational drug Internet Web site. Several people together from all over the world attracted by such Web sites are described in detail. -
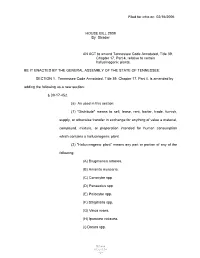
Filed for Intro on 02/16/2006 HOUSE BILL 2909 by Strader an ACT To
Filed for intro on 02/16/2006 HOUSE BILL 2909 By Strader AN ACT to amend Tennessee Code Annotated, Title 39, Chapter 17, Part 4, relative to certain hallucinogenic plants. BE IT ENACTED BY THE GENERAL ASSEMBLY OF THE STATE OF TENNESSEE: SECTION 1. Tennessee Code Annotated, Title 39, Chapter 17, Part 4, is amended by adding the following as a new section: § 39-17-452. (a) As used in this section: (1) "Distribute" means to sell, lease, rent, barter, trade, furnish, supply, or otherwise transfer in exchange for anything of value a material, compound, mixture, or preparation intended for human consumption which contains a hallucinogenic plant. (2) "Hallucinogenic plant" means any part or portion of any of the following: (A) Brugmansia arborea. (B) Amanita muscaria. (C) Conocybe spp. (D) Panaeolus spp. (E) Psilocybe spp. (F) Stropharia spp. (G) Vinca rosea. (H) Ipomoea violacea. (I) Datura spp. HB2909 01337129 -1- (J) Pancreatium trianthum. (K) Kaempferia galanga. (L) Olmedioperebea sclerophylla. (M) Mesembryanthemum spp. (N) Virola spp. (O) Anadenanthera peregrina. (P) Anadenanthera colubrina. (Q) Erythina spp. (R) Genista canariensis. (S) Mimosa hostilis. (T) Rhynchosia spp. (U) Sophora secundiflora. (V) Peganum harmala. (W) Banisteriopsis spp. (X) Tetrapteris methystica. (Y) Heimia salicfolia. (Z) Tabernanthe iboga. (AA) Prestonia amazonica. (BB) Lagoehilus inebrians. (CC) Rivea corymbosa. (DD) Salvia divinorum. (EE) Atropa belladonna. (FF) Hyoscyamus niger. (GG) Mandragora officinarum. (HH) Brunfelsia spp. - 2 - 01337129 (II) Methysticodendron amesianum. (JJ) Latua pubiflora. (KK) Calea Zacatechichi. (LL) Physalis subglabrata. (MM) Solanum carolinense. (3) "Homeopathic drug" means any drug labeled as being homeopathic which is listed in the Homeopathic Pharmacopeia of the United States, an addendum to it, or its supplements.