ORIGINAL ARTICLES Problems Faced by Rural People In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
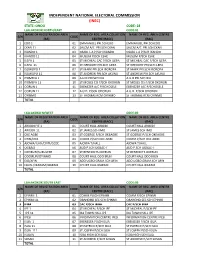
Ondo Code: 28 Lga:Akokok North/East Code:01 Name of Registration Area Name of Reg
INDEPENDENT NATIONAL ELECTORAL COMMISSION (INEC) STATE: ONDO CODE: 28 LGA:AKOKOK NORTH/EAST CODE:01 NAME OF REGISTRATION AREA NAME OF REG. AREA COLLATION NAME OF REG. AREA CENTRE S/N CODE (RA) CENTRE (RACC) (RAC) 1 EDO 1 01 EMMANUEL PRI.SCHEDO EMMANUEL PRI.SCHEDO 2 EKAN 11 02 SALEM A/C PRI.SCH EKAN SALEM A/C PRI.SCH EKAN 3 IKANDO 1 03 OSABL L.A P/SCH IKANDO OSABL L.A P/SCH IKANDO 4 IKANDO 11 04 MUSLIM P/SCH ESHE MUSLIM P/SCH ESHE 5 ILEPA 1 05 ST MICHEAL CAC P/SCH ILEPA ST MICHEAL CAC P/SCH ILEPA 6 ILEPA 11 06 ST GREGORY PRI.SCH ILEPA ST GREGORY PRI.SCH ILEPA 7 ISOWOPO 1 07 ST MARK PRI.SCH IBOROPA ST MARK PRI.SCH IBOROPA 8 ISOWOPO 11 08 ST ANDREW PRI.SCH AKUNU ST ANDREW PRI.SCH AKUNU 9 IYOMEFA 1 09 A.U.D PRI.SCH IKU A.U.D PRI.SCH IKU 10 IYOMEFA 11 10 ST MOSES CIS P/SCH OKORUN ST MOSES CIS P/SCH OKORUN 11 OORUN 1 11 EBENEZER A/C P/SCHOSELE EBENEZER A/C P/SCHOSELE 12 OORUN 11 12 A.U.D. P/SCH ODORUN A.U.D. P/SCH ODORUN 13 OYINMO 13 ST THOMAS RCM OYINMO ST THOMAS RCM OYINMO TOTAL LGA:AKOKO N/WEST CODE:02 NAME OF REGISTRATION AREA NAME OF REG. AREA COLLATION NAME OF REG. AREA CENTRE S/N CODE (RA) CENTRE (RACC) (RAC) 1 ARIGIDI IYE 1 01 COURT HALL ARIGIDI COURT HALL ARIGIDI 2 ARIGIDI 11 02 ST JAMES SCH IMO ST JAMES SCH IMO 3 OKE AGBE 03 ST GOERGE P/SCH OKEAGBE ST GOERGE P/SCH OKEAGBE 4 OYIN/OGE 04 COMM.P/SCH OKE AGBE COMM.P/SCH OKE AGBE 5 AJOWA/ILASI/ERITI/GEDE 05 AJOWA T/HALL AJOWA T/HALL 6 OGBAGI 06 AUD P.SCH OGBAC-I AUD P.SCH OGBAC-I 7 OKEIRUN/SURULERE 07 ST BENEDICTS OKERUN ST BENEDICTS OKERUN 8 ODOIRUN/OYINMO 08 COURT HALL ODO IRUN COURT HALL ODO IRUN 9 ESE/AFIN 09 ADO UGBO GRAM.SCH AFIN ADO UGBO GRAM.SCH AFIN 10 EBUSU/IKARAM/IBARAM 10 COURT HALL IKARAM COURT HALL IKARAM TOTAL LGA:AKOKOK SOUTH EAST CODE:03 NAME OF REGISTRATION AREA NAME OF REG. -

A Historical Survey of Socio-Political Administration in Akure Region up to the Contemporary Period
European Scientific Journal August edition vol. 8, No.18 ISSN: 1857 – 7881 (Print) e - ISSN 1857- 7431 A HISTORICAL SURVEY OF SOCIO-POLITICAL ADMINISTRATION IN AKURE REGION UP TO THE CONTEMPORARY PERIOD Afe, Adedayo Emmanuel, PhD Department of Historyand International Studies,AdekunleAjasin University,Akungba-Akoko, Ondo State, Nigeria Abstract Thepaper examines the political transformation of Akureregion from the earliest times to the present. The paper traces these stages of political development in order to demonstrate features associated with each stage. It argues further that pre-colonial Akure region, like other Yoruba regions, had a workable political system headed by a monarch. However, the Native Authority Ordinance of 1916, which brought about the establishment of the Native Courts and British judicial administration in the region led to the decline in the political power of the traditional institution.Even after independence, the traditional political institution has continually been subjugated. The work relies on both oral and written sources, which were critically examined. The paper, therefore,argues that even with its present political status in the contemporary Nigerian politics, the traditional political institution is still relevant to the development of thesociety. Keywords: Akure, Political, Social, Traditional and Authority Introduction The paper reviews the political administration ofAkure region from the earliest time to the present and examines the implication of the dynamics between the two periods may have for the future. Thus,assessment of the indigenous political administration, which was prevalent before the incursion of the colonial administration, the political administration during the colonial rule and the present political administration in the region are examined herein.However, Akure, in this context, comprises the present Akure North, Akure South, and Ifedore Local Government Areas of Ondo State, Nigeria. -

Petroleum Extraction, Agriculture and Local Communities in the Niger Delta
Petroleum Extraction, Agriculture and Local Communities in the Niger Delta. A Case of Ilaje Community. Adedayo Ladelokun Howard University Chapter I: Introduction Petroleum resource exploration and extraction-- ● A crucial economic activity ● Petroleum resources contributed substantially to economic development ● Conversely, petroleum exploration and extraction often induce negative impacts on other economic activities such as agriculture. ● Threatens environmental Safety. ● Ilaje Community,Ondo State,Nigeria, was chosen as a case study. Introduction Cont. ● Location and member states of the Niger Delta. Located in Coastal Southern Region of Nigeria. Map of the Niger Delta region Niger Delta Image of the Niger Delta Source: Ken Saro-Wiwa 20 years on Niger Delta ... Cnn.com Map of Ondo State Showing the 18 Local Government Areas Ilaje Local Government Introduction Cont. ● Population --- Estimated at 46 Million(UNDP) ● Geographical Landmark --- ND Covers area over 70,000 Sq Kilometers (ie 27,000 Miles) ● Occupation --- Farming, Fishing, Canoe Making, Trading, Net Making, and Mat Making. ● Ilaje Community --- Occupies Atlantic Coastline of Ondo State,Nigeria. ● Ilaje Local Government (Polluted Area) was one of the 18 Local Governments in Ondo State, Nigeria. ● Five Local Governments were randomly selected to served as control. Scope of the study This research work will cover Ilaje Community in Ondo State. Ondo State is located in the petroleum producing area of the Niger Delta Ilaje community was mainly into agricultural production Chapter II: Literature Review ● Agriculture in Economic Development of Nigeria: ○ Machinery for life sustenance ○ Supportive role raw material provision for industrial development ○ Todaro MP (2000) viewed role of AG as passive and supportive ○ Precondition for eco developed ○ Rapid structural transformation of the AG sector Literature Review Continues Jhingan M.L (1985) opined that: (a) AG provides food surplus for the rapidly expanding population. -

Gender Sensitivity to Public School Enrolment in Ondo State, Nigeria Using Systematic Sampling
DOI: http://dx.doi.org/10.4314/gjpas.v22i1.8 GLOBAL JOURNAL OF PURE AND APPLIED SCIENCES VOL. 22, 2016: 61-71 COPYRIGHT© BACHUDO SCIENCE CO. LTD PRINTED IN NIGERIA ISSN 1118-0579 61 www.globaljournalseries.com, Email: [email protected] GENDER SENSITIVITY TO PUBLIC SCHOOL ENROLMENT IN ONDO STATE, NIGERIA USING SYSTEMATIC SAMPLING ADEDAYO AMOS ADEWARA AND ADEBOLA ANTHONIA ADENIYI (Received 15 December 2015; Revision Accepted 3 March 2016) ABSTRACT This study employed the total number of public schools in Ondo, Nigeria which gives information on the name of the school, males and females in each school from JSS1 to SS3 in the eighteen local government areas. Systematic sampling was used to select forty eight schools from the two hundred and eighty eight public schools in the state during the 2012/2013 and 2013/2014 academic sections. Applying the instrument of Pearson product moment correlation coefficient, the study revealed that (i).females are more sensitive to public school enrolment during 2012/2013 and 2013/2014 academic sessions than their males counterparts, (ii).there is significant difference between the female enrolments during the two academic sessions, (iii).there is significant difference between the male enrolments during the two academic sessions and (iv). the trend of male female enrolments in the selected public schools shows improvement during 2013/2014 over that of 2012/2013 academic session. KEYWORD: Gender, Sensitivity, Systematic Sampling, School, Enrolment INTRODUCTION University of Technology, Akure, Adekunle Ajasin University, Akungba/Akoko, Ondo State polytechnic, The foundation of any state is in the number of Owo, Federal College of Agriculture, Akure and people who are literate in that particular state. -

Ondo State Conflictbulletin: Nigeria
THE FUND FOR PEACE Nigeria Conflict Bulletin: Ondo State Patterns and Trends, January 2012 - J u n e 2 0 1 5 While violence in Ondo has historically Democratic Party (PDP). The next page shows the relative distribution of been relatively low, in the first half of 2015 gubernatorial elections are scheduled for incidents from one LGA to the next from reported fatalities increased significantly as 2016. January 2012 to June 2015. The trendline on compared to previous years. This was the next page shows the number of mainly in connection to a few incidents of This Conflict Bulletin provides a brief incidents and fatalities over time. The bar criminality (bank robberies in Owo and snapshot of the trends and patterns of chart shows the relative trend of incidents Akoko North West LGAs) and piracy (Ilaje conflict risk factors at the State and LGA of insecurity by LGA per capita. LGA) that killed dozens. Other issues, levels, drawing on the data available on the reported in Ondo included political tensions P4P Digital Platform for Multi-Stakeholder The summaries draw on data collected by and cult violence. Engagement (www.p4p-nigerdelta.org). It ACLED, FFP’s UNLocK, the Council on represents a compilation of the data from Foreign Relations’ NST, WANEP Nigeria, CSS/ After the 2012 gubernatorial election, in the sources listed below, not necessarily the ETH Zurich, NEEWS2015, and Nigeria Watch which Olusegun Mimiko of the Labour Party opinions of FFP or any other organization integrated on the P4P platform. They also (LP) was re-elected, the losing parties raised that collaborated on the production of this draw on data and information from concerns about alleged election bulletin. -

Conflict Incident Monthly Tracker
Conflict Incident Monthly Tracker Ondo State: July - August 2018 B a ck gro und was reportedly kidnapped by masked that had raped them earlier. In July, a 45- gunmen at his farm in Akure North LGA. year old man was reportedly arrested for This monthly tracker is designed to update raping his daughter in Ondo town, Akure Peace Agents on patterns and trends in Cult Violence: In June, three people were South LGA. conflict risk and violence, as identified by the reportedly killed by cultists in Akure South Integrated Peace and Development Unit LGA. The victims were killed with machetes Others: In June, a 13-year old pupil was (IPDU) early warning system, and to seek at three different locations in the area. reportedly killed by a stray bullet fired by a feedback and input for response to mitigate Violence Affecting Women and Girls soldier in Akoko North West LGA. Separately, areas of conflict. (VAWG): In addition to the impact of two siblings, aged 2 and 4, were reportedly burned to death by fire at their home in Patterns and Trends criminality and communal tensions on women and girls listed above, sexual Akure South LGA. M ay-J ul y 20 1 8 violence was also reported during this Recent Incidents or According to Peace Map data (see Figure 1), period. In May, for instance, a 42-year old incidents reported in Ondo state during this man reportedly raped his neighbor’s 10-year Issues, August 2018 period included communal tensions, old daughter in Akure South LGA. Separately, Incidents during the month related mainly to criminality, cult violence, domestic violence, five young men reportedly tortured and criminality, communal tension, and domestic and Violence Affecting Women and Girls raped two under-aged girls in Ondo West violence. -

Conflict Bulletin: Ondo State
The Fund for Peace Conflict Bulletin: Ondo State Patterns and Trends, 2012-2014 election irregularities and intimidation. The ACLED integrated on the P4P platform. They next gubernatorial elections are slated for also draw on data and information from 2016. “Violence in Nigeria: Patterns and Trends,” by Patricia Taft and Nate Haken (Springer In early 2014, most incidents in Ondo State Press, April 2015). involved domestic and interpersonal violence. In May, a clash between rival cult groups reportedly left one person dead. LGA Level Summary Overall, much of the violence in Ondo state was related to instances of petty crime and Akure North/South kidnappings. (Ondo Central Senatorial District) This Conflict Bulletin provides a brief snapshot of the trends and patterns of During the second half of 2012, violence conflict risk factors at the State and LGA sometimes had a political dimension in the levels, drawing on relevant data made context of a hotly contested gubernatorial ndo state has a population of available from the P4P Digital Platform for election in October. Both the Action approximately 3.44 million according Multi-Stakeholder Engagement (www.p4p- Congress of Nigeria and the People’s to the most recent census (2006). The nigerdelta.org). It represents a compilation majority are of Yoruba descent, with of the data from sources listed below, not Reported Violence a sizable minority of those from Ijaw necessarily opinions of FFP or any other subgroups, particularly along the coast. organization that collaborated on the Incidents per million people, 2014 (Jul-Dec) Ondo derives most of its revenue from the production of this bulletin. -

A Focus on Iju Town, Ondo State, Nigeria)
Civil and Environmental Research www.iiste.org ISSN 2224-5790 (Paper) ISSN 2225-0514 (Online) Vol.9, No.9, 2017 Willingness to Improving Infrastructure (A Focus on Iju Town, Ondo State, Nigeria) Okosun, Senator Endurance 1 Ajisola, Kolawole Thomas 2 Oluwajana, Somope Modupe 3 1.Department of Urban and Regional Planning, School of Environmental Technology. Federal University of Technology Akure, Nigeria 2.Department of Computer Science, College of Education Ikere, Ikere Ekiti, Nigeria 3.Department of Quantity Surveying, School of Environmental Technology. Federal University of Technology Akure, Nigeria Abstract In the 21 st century of human habitat and global transformation of towns and cities, a nation develops through willingness of stakeholders (i.e. Government, Community Based Organizations, Non-Governmental Organizations, and Individuals) in improving infrastructural facilities that allow a society to function effectively. This study examined the effects of infrastructure on the socio-economic livelihood of the people in Iju community, with a view to enhancing development and alleviating poverty. Data was collected with the aid of structured questionnaire from 180 respondents using stratified sampling. The sample size was the ratio of buildings. The processing of data in the study was carried out using the Statistical Package for Social Sciences (SPSS) version 19. Data collected were analyzed at two levels using univariate and bivariate statistics. The Univariate Analysis was used to present the data on frequency distribution through the use of tables, charts, maps, and percentages. The Bivariate Analysis was used in carrying out the tests of the formulated hypotheses Findings revealed that provisions of infrastructures such as road, water supply, electricity, school and town halls were instrumental in improving the socio-economic activities of the people, however the condition of some facilities in the town was dilapidated and as such had not been adequately maintained. -

BRIEF HISTORY Ondo State Was Created in 1976 out of the Former
9 Ijebu North 82 10 Ijebu North East 94 11 Ijebu Ode 70 12 Ikenne 50 13 Imeko / Afon 80 14 Ipokia 120 15 Obafemi / Owode 20 16 Odeda 30 17 Odogbolu 58 18 0gun Waterside 201 19 Remo North 58 20 Sagamu 45 ONDO BRIEF HISTORY Ondo State was created in 1976 out of the former Western State. The state lies between latitudes 5 45’ and 7 52’N and longitudes 4 20’ and 6 03’E. It is bounded on the east by Edo and Delta states, on the west by Ogun and Osun states, on the north by Ekiti and Kogi states, and to the south by the Bight of Benin of the Atlantic Ocean. The state occupies a land area of about 15,000 Square kilometers with a population of 3,441,924 people according to 2006 census. The state has eighteen (18) Local Government Areas, with Akure as the capital city as well as the largest settlement. Some of the other prominent towns in the state are Ondo, Owo, Ore, Okitipupa, Ikare, Idanre, and Ile-Oluji. The people of the state are mostly Yoruba, although other Nigerians and foreign nationals equally live in the state. Agriculture is the mainstay of the people of Ondo State. The state has notable tourist attractions including Owo Museum, Ipale Iloro Water Falls, Igbokoda Water Front, Oke Maria Hills and Olumirin Water Falls. SENATORIAL DISTRICTS S/N DISTRICT LGA COMPOSITION RA PU COLLATION CENTRE 82 Ondo North Akoko North East/ Akoko North 72 889 Mapo Hall Owo SD/082/0D West/Akoko South East/Akoko South West/Owo Ose 83 Ondo Akure North/Akure South/Idanre 65 978 St. -

Conflict Incident Monthly Tracker
Conflict Incident Monthly Tracker Ondo State: June - Ju ly 201 8 B a ck gro und installation of a new monarch. Separately, a girls were reportedly kidnapped by the wife woman reportedly died during a clash of one of the five men that had earlier raped, This monthly tracker is designed to update between Yorubas and Hausas in Sabo, Akure and tortured them in Ondo West LGA. Peace Agents on patterns and trends in South LGA. The woman slumped and died of conflict risk and violence, as identified by the Political Tension: In May, the Deputy shock while she was searching for her son at Integrated Peace and Development Unit Speaker of the Ondo State House of the scene of the clash. (IPDU) early warning system, and to seek Assembly was impeached by his colleagues. feedback and input for response to mitigate Violence Affecting Women and Girls Others: In June, a 13-year old pupil was areas of conflict. (VAWG): In addition to the impact of reportedly killed by a stray bullet fired by a criminality and communal tensions on Patterns and Trends soldier who was maintaining order during a women and girls listed above, sexual cultural display by some Fulani men in Akoko A pr il - J un e 20 1 8 violence was also reported during this North West LGA. Separately, two siblings, According to Peace Map data (see Figure 1), period. In May, for instance, a 42-year old aged 2 and 4, were reportedly burned to there was an increase in conflict risk and man was reportedly arrested and sentenced death by fire at their home in Akure South lethal violence in Ondo state in June 2018. -

ISSN: 2320-5407 Int
ISSN: 2320-5407 Int. J. Adv. Res. 6(2), 397-407 Journal Homepage: -www.journalijar.com Article DOI:10.21474/IJAR01/6451 DOI URL: http://dx.doi.org/10.21474/IJAR01/6451 RESEARCH ARTICLE GEOGRAPHICAL ANALYSIS OF ONDO STATE GUBERNATORIAL ELECTION RESULTS OF 2012 AND 2016. Richard Babajide Adeleke. Department of Geography, University of Ibadan. …………………………………………………………………………………………………….... Manuscript Info Abstract ……………………. ……………………………………………………………… Manuscript History Space is one of the key drivers of election results and the few studies on the influence of space on election results in Nigeria reported a mere Received: 05 December 2017 spatial distribution without giving an insight into their spatial Final Accepted: 07 January 2018 clustering. Using Global and Local Moran’s I geospatial techniques, the Published: February 2018 study found a significant positive spatial autocorrelation and clustering Keywords:- of votes in 2012 election for the candidates of Peoples Democratic Election, GIS, Spatial Autocorrelation, Party in Ilaje, Irele and Ese-Odo local government areas while that of Ondo State, Nigeria Action Congress of Nigeria was in Owo and Akoko Southwest. In 2016 election, that of All Progressives Congress was in Owo and Ondo East. However, there was a significant negative spatial autocorrelation and clustering of votes for the candidates of Labour Party in Akure North and Alliance for Democracy in Ese-Odo and Ilaje in 2012 election. On the whole, the pattern of votes cast for the victorious party in 2016 election was found to be more regionally concentrated when compared to 2012. The study concluded that a lot still has to be done with regard to voters’ education. Copy Right, IJAR, 2018,. -

Geostatistical Investigation and Ambient Radiation Mapping of Akure North and South Local Government
ISSN: 2455-2631 © December 2016 IJSDR | Volume 1, Issue 12 Geostatistical investigation and ambient radiation mapping of Akure north and south local government areas of Ondo state, Nigeria Dinyo Enoch Omosehinmi1, Adeseye Muyiwa Arogunjo2 Department of Physics Federal University of Technology, Akure, Nigeria Abstract: The need for geostatistical estimation and mapping of ambient radiation prevalence in Akure North and South Local Government Areas of Ondo State, Nigeria prompted dose rate assessment at 166 selected sample locations in these areas. Global Positioning System (GPS) and Geiger-Muller Counter (GMC) were respectively used for location identification and dose rates measurement within an interval of ퟏ − ퟏ. ퟓ퐤퐦. The dose rates were measured at ퟏ퐦 above the ground level. The values of Dose Rate (DR) in air, and Annual Dose Rate (ADR) in air ranged from ퟎ. ퟏퟔ ± ퟎ. ퟎퟏ to ퟎ. ퟑퟕ ± ퟎ. ퟎퟒ 훍퐒훎 퐡 and ퟏ. ퟒퟎ ± ퟎ. ퟎퟗ to ퟑ. ퟐퟒ ± ퟎ. ퟑퟓ 퐦퐒훎 퐲 respectively. The mean dose rate and mean annual dose rate in air are ퟎ. ퟐퟔ ± ퟎ. ퟎퟑ 훍퐒훎 퐡 and ퟐ. ퟐퟖ ± ퟎ. ퟐퟔ 퐦퐒훎 퐲. The measured DR and calculated ADR was processed in ArcGIS and Surfer, using Inverse Distance Weighting (IDW) and Kriging interpolation to produce delineation maps of ambient radiation, in 2D and 3D. Only about ퟏ% of the variation in dose rate is explained by spatial data- elevation, latitude and longitude, which suggest very weak correlation between DR and spatial data(s). All dose rates are within the limit of internationally accepted Ambient Radiation levels; it poses no health effect on the general public.