Texas Medication Algorithm Project Procedural Manual: Schizophrenia Algorithm
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Negative Symptoms in Schizophrenia
Reward Processing Mechanisms of Negative Symptoms in Schizophrenia Gregory P. Strauss, Ph.D. Assistant Professor Department of Psychology University of Georgia Disclosures ACKNOWLEDGMENTS & DISCLOSURES ▪ Receive royalties and consultation fees from ProPhase LLC in connection with commercial use of the BNSS and other professional activities; these fees are donated to the Brain and Behavior Research Foundation. ▪ Last 12 Months: Speaking/consultation with Minerva, Lundbeck, Acadia What are negative symptoms and why are they important? Domains of psychopathology in schizophrenia Negative Symptoms ▪ Negative symptoms - reductions in goal-directed activity, social behavior, pleasure, and the outward expression of emotion or speech Cognitive Positive ▪ Long considered a core feature of psychotic disorders1,2 Deficits Symptoms ▪ Distinct from other domains of psychopathology (e.g., psychosis, disorganization) 3 ▪ Associated with a range of poor clinical outcomes (e.g., Disorganized Affective disease liability, quality of life, subjective well-being, Symptoms Symptoms recovery) 4-7 1. Bleuler E. [Dementia praecox or the group of schizophrenias]. Vertex Sep-Oct 2010;21(93):394-400. 2. Kraepelin E. Dementia praecox and paraphrenia (R. M. Barclay, Trans.). New York, NY: Krieger. 1919. 3. Peralta V, Cuesta MJ. How many and which are the psychopathological dimensions in schizophrenia? Issues influencing their ascertainment. Schizophrenia research Apr 30 2001;49(3):269-285. 4. Fervaha G, Remington G. Validation of an abbreviated quality of life scale for schizophrenia. Eur Neuropsychopharmacol Sep 2013;23(9):1072-1077. 5. Piskulic D, Addington J, Cadenhead KS, et al. Negative symptoms in individuals at clinical high risk of psychosis. Psychiatry research Apr 30 2012;196(2-3):220-224. -

Guidance on the Use of Mood Stabilizers for the Treatment of Bipolar Affective Disorder Version 2
Guidance on the use of mood stabilizers for the treatment of bipolar affective disorder Version 2 RATIFYING COMMITTEE DRUGS AND THERAPEUTICS GROUP DATE RATIFIED July 2015 REPLACES Version 1 dated July 2013 NEXT REVIEW DATE July 2017 POLICY AUTHORS Jules Haste, Lead Pharmacist, Brighton and Hove Members of the Pharmacy Team (contributors are listed overleaf) If you require this document in an alternative format, i.e. easy read, large text, audio or Braille please contact the pharmacy team on 01243 623349 Page 1 of 49 Contributors Jed Hewitt, Chief Pharmacist - Governance & Professional Practice James Atkinson, Pharmacist Team Leader Mental Health and Community Services Miguel Gomez, Lead Pharmacist, Worthing. Hilary Garforth, Lead Pharmacist, Chichester. Pauline Daw, Lead Pharmacist (CRHTs & AOT), East Sussex. Iftekhar Khan, Lead Pharmacist (S&F Service), East Sussex. Graham Brown, Lead Pharmacist CAMHS & EIS. Gus Fernandez, Specialist Pharmacist MI and MH Lisa Stanton, Specialist Pharmacist Early Intervention Services & Learning Disabilities. Nana Tomova, Specialist Pharmacist, Crawley. Page 2 of 49 Section Title Page Number Introduction and Key Points 4 1. General principles in the treatment of acute mania 6 2. General principles in the treatment of bipolar depression 8 3. General principles in long term treatment 10 4. Rapid cycling 13 5. Physical health 13 6. Treatment in special situations 6.1 Pregnancy 15 6.2 Breast-feeding 17 6.3 Older adults 19 6.4 Children and adolescents 22 6.5 Learning disabilities 29 6.6 Cardiac dysfunction 30 6.7 Renal dysfunction 34 6.8 Hepatic dysfunction 37 6.9 Epilepsy 41 7. The risk of switching to mania with antidepressants 43 8. -

Homicide and Associated Steroid Acute Psychosis: a Case Report
Hindawi Publishing Corporation Case Reports in Medicine Volume 2011, Article ID 564521, 4 pages doi:10.1155/2011/564521 Case Report Homicide and Associated Steroid Acute Psychosis: A Case Report G. Airagnes,1, 2 C. Rouge-Maillart,1, 3 J.-B. Garre,2, 3 and B. Gohier2 1 Service de M´edecine L´egale, CHU d’Angers, 49933 Angers Cedex 09, France 2 D´epartement de Psychiatrie et de Psychologie m´edicale, CHU d’Angers, 49933 Angers Cedex 09, France 3 IFR 132, Universit´e d’Angers, 49035 Angers, France Correspondence should be addressed to G. Airagnes, [email protected] Received 22 June 2011; Revised 26 August 2011; Accepted 26 September 2011 Academic Editor: Massimo Gallerani Copyright © 2011 G. Airagnes et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. We report the case of an old man treated with methylprednisolone for chronic lymphoid leukemia. After two months of treatment, he declared an acute steroid psychosis and beat his wife to death. Steroids were stopped and the psychotic symptoms subsided, but his condition declined very quickly. The clinical course was complicated by a major depressive disorder with suicidal ideas, due to the steroid stoppage, the leukemia progressed, and by a sudden onset of a fatal pulmonary embolism. This clinical case highlights the importance of early detection of steroid psychosis and proposes, should treatment not be stopped, a strategy of dose reduction combined with a mood stabilizer or antipsychotic treatment. -

The Clinical Presentation of Psychotic Disorders Bob Boland MD Slide 1
The Clinical Presentation of Psychotic Disorders Bob Boland MD Slide 1 Psychotic Disorders Slide 2 As with all the disorders, it is preferable to pick Archetype one “archetypal” disorder for the category of • Schizophrenia disorder, understand it well, and then know the others as they compare. For the psychotic disorders, the diagnosis we will concentrate on will be Schizophrenia. Slide 3 A good way to organize discussions of Phenomenology phenomenology is by using the same structure • The mental status exam as the mental status examination. – Appearance –Mood – Thought – Cognition – Judgment and Insight Clinical Presentation of Psychotic Disorders. Slide 4 Motor disturbances include disorders of Appearance mobility, activity and volition. Catatonic – Motor disturbances • Catatonia stupor is a state in which patients are •Stereotypy • Mannerisms immobile, mute, yet conscious. They exhibit – Behavioral problems •Hygiene waxy flexibility, or assumption of bizarre • Social functioning – “Soft signs” postures as most dramatic example. Catatonic excitement is uncontrolled and aimless motor activity. It is important to differentiate from substance-induced movement disorders, such as extrapyramidal symptoms and tardive dyskinesia. Slide 5 Disorders of behavior may involve Appearance deterioration of social functioning-- social • Behavioral Problems • Social functioning withdrawal, self neglect, neglect of • Other – Ex. Neuro soft signs environment (deterioration of housing, etc.), or socially inappropriate behaviors (talking to themselves in -
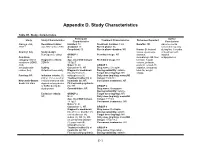
Appendix D. Study Characteristics
Appendix D. Study Characteristics Table D1. Study characteristics Participant Author Study Study Characteristics Treatment Characteristics Outcomes Reported Characteristics Conclusions Alacqua et al., Recruitment dates: Enrolled: 73 Treatment duration: 3 mo Benefits: NR Adverse events 2008 96 Jan 2002 to Dec 2003 Analyzed: 73 Run-in phase: No occurred frequently Completed: 50 Run-in phase duration: NR Harms: Behavioral during first 3 months Country: Italy Study design: issues, dyskinesia, of treatment with Retrospective cohort GROUP 1 Permitted drugs: NR dystonia, atypical Condition N: 2 dermatologic AE, liver antipsychotics. category: Mixed Diagnostic criteria: Age, mean±SD (range): Prohibited drugs: NR function, hepatic conditions (ADHD, DSM-IV 15.5±0.7 volume, prolactin, ASD, Males %: 50 GROUP 1 prolactin-related AE, schizophrenia- Setting: Caucasian %: NR Drug name: Clozapine sedation, sleepness, related, tics) Outpatient/community Diagnostic breakdown Dosing variability: variable total AE, weight (n): psychosis (1), Target dose (mg/day): NR change Funding: NR Inclusion criteria: (1) schizophrenia (1) Daily dose (mg/day), mean±SD ≤18 yr, (2) received an Treatment naïve (n): all (range): 150±70.1 Newcastle-Ottawa incident treatment with Inpatients (n): NR Concurrent treatments: NR Scale: 6/8 stars atypical antipsychotics First episode psychosis or SSRIs during the (n): NR GROUP 2 study period Comorbidities: NR Drug name: Olanzapine Dosing variability: variable Exclusion criteria: GROUP 2 Target dose (mg/day): NR NR N: 24 Daily dose -

Mechanism of Action of Antidepressants and Mood Stabilizers
79 MECHANISM OF ACTION OF ANTIDEPRESSANTS AND MOOD STABILIZERS ROBERT H. LENOX ALAN FRAZER Bipolar disorder (BPD), the province of mood stabilizers, the more recent understanding that antidepressants share has long been considered a recurrent disorder. For more this property in UPD have focused research on long-term than 50 years, lithium, the prototypal mood stabilizer, has events, such as alterations in gene expression and neuroplas- been known to be effective not only in acute mania but ticity, that may play a significant role in stabilizing the clini- also in the prophylaxis of recurrent episodes of mania and cal course of an illness. In our view, behavioral improvement depression. By contrast, the preponderance of past research and stabilization stem from the acute pharmacologic effects in depression has focused on the major depressive episode of antidepressants and mood stabilizers; thus, both the acute and its acute treatment. It is only relatively recently that and longer-term pharmacologic effects of both classes of investigators have begun to address the recurrent nature of drugs are emphasized in this chapter. unipolar disorder (UPD) and the prophylactic use of long- term antidepressant treatment. Thus, it is timely that we address in a single chapter the most promising research rele- vant to the pharmacodynamics of both mood stabilizers and MOOD STABILIZERS antidepressants. As we have outlined in Fig. 79.1, it is possible to charac- The term mood stabilizer within the clinical setting is com- terize both the course and treatment of bipolar and unipolar monly used to refer to a class of drugs that treat BPD. -
Introduction to Agitation, Delirium, and Psychosis Curriculum for Psychologists/Social Workers
FACILITATOR MANUAL ENGLISH-HAITI Introduction to Agitation, Delirium, and Psychosis Curriculum for Psychologists/Social Workers Introduction to Agitation, Delirium, and Psychosis Curriculum for Psychologists/Social Workers Partners In Health (PIH) is an independent, non-profit organization founded over twenty years ago in Haiti with a mission to provide the very best medical care in places that had none, to accompany patients through their care and treatment, and to address the root causes of their illness. Today, PIH works in fourteen countries with a comprehensive approach to breaking the cycle of poverty and disease — through direct health-care delivery as well as community-based interventions in agriculture and nutrition, housing, clean water, and income generation. PIH’s work begins with caring for and treating patients, but it extends far beyond to the transformation of communities, health systems, and global health policy. PIH has built and sustained this integrated approach in the midst of tragedies like the devastating earthquake in Haiti. Through collaboration with leading medical and academic institutions like Harvard Medical School and the Brigham & Women’s Hospital, PIH works to disseminate this model to others. Through advocacy efforts aimed at global health funders and policymakers, PIH seeks to raise the standard for what is possible in the delivery of health care in the poorest corners of the world. PIH works in Haiti, Russia, Peru, Rwanda, Sierra Leone, Liberia Lesotho, Malawi, Kazakhstan, Mexico and the United States. For more information about PIH, please visit www.pih.org. Many PIH and Zanmi Lasante staff members and external partners contributed to the development of this training. -

Page 1 of 85 Reference ID: 3091122
HIGHLIGHTS OF PRESCRIBING INFORMATION As an adjunct to 2-5 mg 5-10 mg 15 mg These highlights do not include all the information needed to use ABILIFY antidepressants for the /day /day /day safely and effectively. See full prescribing information for ABILIFY. treatment of major ® ABILIFY (aripiprazole) Tablets depressive disorder – adults ® ABILIFY DISCMELT (aripiprazole) Orally Disintegrating Tablets (2.3) ® Irritability associated with 2 mg/day 5-10 mg/day 15 mg/day ABILIFY (aripiprazole) Oral Solution ® autistic disorder – pediatric ABILIFY (aripiprazole) Injection FOR INTRAMUSCULAR USE ONLY patients (2.4) Initial U.S. Approval: 2002 Agitation associated with 9.75 mg /1.3 30 mg/day schizophrenia or bipolar mL injected injected WARNINGS: INCREASED MORTALITY IN ELDERLY mania – adults (2.5) IM IM PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS and • Oral formulations: Administer once daily without regard to meals (2) SUICIDALITY AND ANTIDEPRESSANT DRUGS • IM injection: Wait at least 2 hours between doses. Maximum daily dose See full prescribing information for complete boxed warning. 30 mg (2.5) • Elderly patients with dementia-related psychosis treated with ----------------------DOSAGE FORMS AND STRENGTHS--------------------- antipsychotic drugs are at an increased risk of death. ABILIFY is not approved for the treatment of patients with dementia-related • Tablets: 2 mg, 5 mg, 10 mg, 15 mg, 20 mg, and 30 mg (3) psychosis. (5.1) • Orally Disintegrating Tablets: 10 mg and 15 mg (3) • Oral Solution: 1 mg/mL (3) • Children, adolescents, and young adults taking antidepressants for • Injection: 9.75 mg/1.3 mL single-dose vial (3) major depressive disorder (MDD) and other psychiatric disorders are at increased risk of suicidal thinking and behavior. -

Active Moiety Name FDA Established Pharmacologic Class (EPC) Text
FDA Established Pharmacologic Class (EPC) Text Phrase PLR regulations require that the following statement is included in the Highlights Indications and Usage heading if a drug is a member of an EPC [see 21 CFR 201.57(a)(6)]: “(Drug) is a (FDA EPC Text Phrase) indicated for [indication(s)].” For Active Moiety Name each listed active moiety, the associated FDA EPC text phrase is included in this document. For more information about how FDA determines the EPC Text Phrase, see the 2009 "Determining EPC for Use in the Highlights" guidance and 2013 "Determining EPC for Use in the Highlights" MAPP 7400.13. .alpha. -
Schizophrenia- What You Need to Know
SCHIZOPHRENIA- WHAT YOU NEED TO KNOW BY CATHY CYWINSKI, MSW LCSW SIGNS AND SYMPTOMS OF SCHIZOPHRENIA • Hallucinations- false perception • Delusions –fixed false belief • Grossly Disorganized Speech and Behavior • Tend to dress and act in odd ways • Flat Affect SYMPTOMS • Hallucinations-can occur with any of the five senses: • Auditory hallucinations • Visual hallucinations • Tactile hallucinations • Olfactory hallucinations • Gustatory hallucinations SYMPTOMS • Bizarre delusion – this simply translated means a delusion regarding something that CANNOT possibly happen. • Nonbizarre delusion – this is a delusion regarding something that CAN possibly happen. COMMON TYPES OF DELUSIONS • Grandiose • Erotomanic • Religious • Delusions of Control • Persecutory • Referential SYMPTOMS • Disorganized Speech • Loose associations- may go from one topic to another with no clear logic • Tangentiality- answers to questions may be obliquely related or completely unrelated • Incoherence or word salad- speech may be so severely disorganized that it is nearly incomprehensible SYMPTOMS • Grossly disorganized behavior • A person may appear disheveled, may dress in an unusual manner (many layers of clothes on a hot day), or may display inappropriate sexual behavior. • Alogia-poverty of speech- brief, empty replies • Avolition- inability to initiate and persist in goal directed activates. The person may sit for long periods of time and show little interest in participating in work or social activities. • Catatonic motor behaviors- a marked decrease in reactivity to the environments. SYMPTOMS • Negative Symptoms • Affect flattening- a person’s face appearing immobile and unresponsive, with poor eye contact and reduced body language IS THERE SOMETHING TO FEAR • Myth: People with a severe mental illness are violent and unpredictable. • Fact: The vast majority of people with mental health problems are no more likely to be violent than anyone else. -

Mood Stabilizers
Mood Stabilizers Anticonvulsants Depakene/Stavzor (valproic acid) and Depakote/Depakote ER (divalproex sodium) Equetro, Tegretol, and Tegretol-XR (carbamazepine) Lamictal (lamotrigine) Lyrica (pregabalin) Neurontin (gabapentin) Topamax (topiramate) Trileptal (oxcarbazepine) Lithium Carbonate and Lithium Citrate Lithium carbonate Lithium Citrate Lithobid Second-Generation Antipsychotics Abilify (aripiprazole) Clozaril (clozapine) Geodon (ziprasidone) Invega (paliperidone) Risperdal, Risperdal M-Tab, and Risperdal Consta (risperidone) Seroquel (quetiapine) Zyprexa and Zyprexa Zydis (olanzapine) Simply defined, mood stabilizers are medicines used in treating mood disorders such as bipolar disorder and depression. Bipolar disorder is characterized by mood swings in which the individual cycles between mania and depression. The symptoms fluctuate from euphoria and limitless energy in the manic phase to the depths of depression with little energy, guilt, sadness, decreased concentration, lack of appetite, and sleep distur- bance. Because of the wide range of symptoms, from mania to depression, bipolar disorder is often called manic depression. Mood stabilizers are used to treat acute mania, hypomania (a mild form of mania), mixed episodes (when mania and depression coexist in an episode), and depression. Following the acute episode, mood stabilizers Page 2 of 3 MOOD STABILIZERS are used in maintenance therapy to prevent the cyclical relapse of abnormal mood elevations and depressions. The goals of maintenance treatment with a mood stabilizer are to 1) reduce residual symptoms, 2) prevent manic or depressive relapse, 3) reduce the frequency of cycling into the next manic or depressive episode, 4) improve functioning, and 5) reduce the risk of suicide. Lithium Lithium was one of the first mood stabilizers used in the treatment of bipolar disorder. -

A History of the Pharmacological Treatment of Bipolar Disorder
International Journal of Molecular Sciences Review A History of the Pharmacological Treatment of Bipolar Disorder Francisco López-Muñoz 1,2,3,4,* ID , Winston W. Shen 5, Pilar D’Ocon 6, Alejandro Romero 7 ID and Cecilio Álamo 8 1 Faculty of Health Sciences, University Camilo José Cela, C/Castillo de Alarcón 49, 28692 Villanueva de la Cañada, Madrid, Spain 2 Neuropsychopharmacology Unit, Hospital 12 de Octubre Research Institute (i+12), Avda. Córdoba, s/n, 28041 Madrid, Spain 3 Portucalense Institute of Neuropsychology and Cognitive and Behavioural Neurosciences (INPP), Portucalense University, R. Dr. António Bernardino de Almeida 541, 4200-072 Porto, Portugal 4 Thematic Network for Cooperative Health Research (RETICS), Addictive Disorders Network, Health Institute Carlos III, MICINN and FEDER, 28029 Madrid, Spain 5 Departments of Psychiatry, Wan Fang Medical Center and School of Medicine, Taipei Medical University, 111 Hsin Long Road Section 3, Taipei 116, Taiwan; [email protected] 6 Department of Pharmacology, Faculty of Pharmacy, University of Valencia, Avda. Vicente Andrés, s/n, 46100 Burjassot, Valencia, Spain; [email protected] 7 Department of Pharmacology and Toxicology, Faculty of Veterinary Medicine, Complutense University, Avda. Puerta de Hierro, s/n, 28040 Madrid, Spain; [email protected] 8 Department of Biomedical Sciences (Pharmacology Area), Faculty of Medicine and Health Sciences, University of Alcalá, Crta. de Madrid-Barcelona, Km. 33,600, 28871 Alcalá de Henares, Madrid, Spain; [email protected] * Correspondence: fl[email protected] or [email protected] Received: 4 June 2018; Accepted: 13 July 2018; Published: 23 July 2018 Abstract: In this paper, the authors review the history of the pharmacological treatment of bipolar disorder, from the first nonspecific sedative agents introduced in the 19th and early 20th century, such as solanaceae alkaloids, bromides and barbiturates, to John Cade’s experiments with lithium and the beginning of the so-called “Psychopharmacological Revolution” in the 1950s.