Planning Ahead, Working Together
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Mileage and Admissions
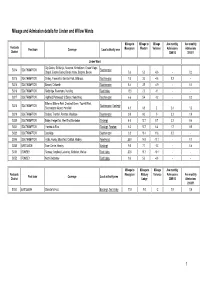
Mileage and Admission details for Linden and Willow Wards Mileage to Mileage to Mileage Ave monthly Ave monthly Postcode Post town Coverage Local authority area Moorgreen Western Variance Admissions Admissions District 2009/10 2010/11 Linden Ward City Centre, St. Mary's, Newtown, Nicholstown, Ocean Village, SO14 SOUTHAMPTON Southampton Chapel, Eastern Docks, Bevois Valley, Bargate, Bevois 5.6 5.0 -0.6 - 0.2 SO15 SOUTHAMPTON Shirley, Freemantle, Banister Park, Millbrook, Southampton 7.6 3.0 -4.6 0.2 - SO16 SOUTHAMPTON Bassett, Chilworth Southampton 8.4 3.5 -4.9 - 0.1 SO16 SOUTHAMPTON Redbridge, Rownhams, Nursling Test Valley 13.0 2.0 -11 - - SO17 SOUTHAMPTON Highfield, Portswood, St Denys, Swaythling Southampton 6.6 5.4 -1.2 - 0.2 Bitterne, Bitterne Park, Chartwell Green, Townhill Park, SO18 SOUTHAMPTON Southampton , Eastleigh Southampton Airport, Harefield 4.5 6.5 2 2.4 1.2 SO19 SOUTHAMPTON Sholing, Thornhill, Peartree, Woolston Southampton 9.0 9.0 0 3.2 1.9 SO30 SOUTHAMPTON Botley, Hedge End, West End, Bursledon Eastleigh 4.0 12.7 8.7 2.2 0.4 SO31 SOUTHAMPTON Hamble-le-Rice Eastleigh , Fareham 6.3 12.7 6.4 1.7 0.5 SO32 SOUTHAMPTON Curdridge Southampton 3.8 15.4 11.6 0.2 - SO45 SOUTHAMPTON Hythe, Fawley, Blackfield, Calshot, Hardley New Forest 25.9 14.8 -11.1 - 0.1 SO50 EASTLEIGH Town Centre, Hamley Eastleigh 9.0 7.7 -1.3 - 0.6 SO51 ROMSEY Romsey, Ampfield, Lockerley, Mottisfont, Wellow Test Valley 20.8 10.7 -10.1 - - SO52 ROMSEY North Baddesley Test Valley 9.6 5.0 -4.6 - - Mileage to Mileage to Mileage Ave monthly Postcode Moorgreen Melbury Variance Admissions Ave monthly Post town Coverage Local authority area District Lodge 2009/10 Admissions 2010/11 SO53 EASTLEIGH Chandler's Ford Eastleigh , Test Valley 11.0 9.0 -2 1.8 0.6 1 Mileage to Mileage to Mileage Ave monthly Ave monthly Postcode Post town Coverage Local authority area Moorgreen Western Variance Admissions Admissions District 2009/10 2010/11 Willow Ward City Centre, St. -

38 Torridge Gardens, West End, SO18 3NF
38 Torridge Gardens, West End, SO18 3NF 38 Torridge Gardens West End Southampton SO18 3NF oieo £220,000 INTRODUCTION Set within a quiet cul-de-sac and within walking distance of the local recreation ground, parade of shops and pub, this lovely and well-proportioned two bedroom home is certainly expected to generate a healthy amount of interest and comes with the additional benefits of no forward chain. Accommodation on the ground floor briefly comprises an entrance porch, good-sized lounge/diner from which stairs lead to the first floor, and then a modern kitchen. On the first floor there are two double bedrooms and a m odern bathroom suite, with the property also benefitting from being fully double glazed and gas centrally heated. Externally, the house comes with attractive front and rear gardens and has the additional benefit of two off road parking spaces to the rear. LOCATION Chartwell Green is a popular suburb of Southampton and is approximately 5 miles away from Southampton's thriving city centre which also has a mainline railway station. Chartwell Green also has a selection of shops and local amenities, which are within walking distance, as is the Cutbush Recreation Ground that provides an attractive short, wooded walk to Riverside Park. The property is also within the catchment area for Townhill Infant School (rated Ofsted Outstanding) and the property also benefits from being close to Townhill Junior School and the highly rated Bitterne Park school. Southampton Airport is also just under half an hour away and all main motorway access routes also benefit from being within easy reach. -

Neighbourhoods in England Rated E for Green Space, Friends of The
Neighbourhoods in England rated E for Green Space, Friends of the Earth, September 2020 Neighbourhood_Name Local_authority Marsh Barn & Widewater Adur Wick & Toddington Arun Littlehampton West and River Arun Bognor Regis Central Arun Kirkby Central Ashfield Washford & Stanhope Ashford Becontree Heath Barking and Dagenham Becontree West Barking and Dagenham Barking Central Barking and Dagenham Goresbrook & Scrattons Farm Barking and Dagenham Creekmouth & Barking Riverside Barking and Dagenham Gascoigne Estate & Roding Riverside Barking and Dagenham Becontree North Barking and Dagenham New Barnet West Barnet Woodside Park Barnet Edgware Central Barnet North Finchley Barnet Colney Hatch Barnet Grahame Park Barnet East Finchley Barnet Colindale Barnet Hendon Central Barnet Golders Green North Barnet Brent Cross & Staples Corner Barnet Cudworth Village Barnsley Abbotsmead & Salthouse Barrow-in-Furness Barrow Central Barrow-in-Furness Basildon Central & Pipps Hill Basildon Laindon Central Basildon Eversley Basildon Barstable Basildon Popley Basingstoke and Deane Winklebury & Rooksdown Basingstoke and Deane Oldfield Park West Bath and North East Somerset Odd Down Bath and North East Somerset Harpur Bedford Castle & Kingsway Bedford Queens Park Bedford Kempston West & South Bedford South Thamesmead Bexley Belvedere & Lessness Heath Bexley Erith East Bexley Lesnes Abbey Bexley Slade Green & Crayford Marshes Bexley Lesney Farm & Colyers East Bexley Old Oscott Birmingham Perry Beeches East Birmingham Castle Vale Birmingham Birchfield East Birmingham -

ITEM NO: C2a APPENDIX 1
ITEM NO: C2a APPENDIX 1 Background Information Approximately 3600 flats and houses were built in Southampton in the five year period up to March 2006. About 80% of these were flats. Some 25% of these flats and houses were in the city centre, where the on-street parking facilities are available to everyone on a "Pay and Display" basis. Outside the central area, only about 10% of the city falls within residents' parking zones. So, out of the 3600 properties in all, it is estimated that only about 270 (or 7.5%) will have been within residents' parking zones and affected by the policy outlined in the report. Only in a few (probably less than 20) of these cases have difficulties come to light. In general, there is no question of anyone losing the right to a permit, although officers are currently seeking to resolve a situation at one particular development where permits have been issued in error. There are currently 13 schemes funded by the City Council and these cover the following areas:- Polygon Area Woolston North Woolston South Newtown/Nicholstown Bevois Town Freemantle Coxford (General Hospital) Shirley University Area (5 zones) These schemes operate from 8 a.m. to 6 p.m. on weekdays and, in some cases, at other times as well. In addition, there are three further schemes at Bitterne Manor, Itchen and Northam that only operate during football matches or other major events at St Mary’s Stadium. These are funded by Southampton Football Club. Within all these schemes, parking bays are marked on the road for permit holders, often allowing short-stay parking by other users as well. -

Hampshire School Places Plan 2021 - 2025
Hampshire School Places Plan 2021 - 2025 Executive Summary 1. Hampshire is proud of the quality of education provided by its diverse and high- performing system of schools, colleges and early years’ settings. The county hosts popular and highly successful infant, junior, primary, 11-16 and 11-18 schools as well as 4-16 schools and the largest post-16 college sector in the country. The County Council is committed to ensuring that families in Hampshire have access to a good local school which offers a rich and varied learning experience, has the highest expectations for their children’s success and where parents can be confident that their children will be safe. All children have the right to an enjoyable, inclusive and expansive education and it is the role of the local authority to intervene on behalf of children, especially the most vulnerable, when this is not the case. 2. Hampshire County Council has a statutory duty to ensure a sufficiency of school places for Hampshire children, this includes to: ▪ Ensuring sufficient childcare options are available to meet the Early Years free entitlement as far as reasonably practicable. ▪ Ensuring sufficient maintained school provision is available to meet the needs of all Hampshire children aged up to 16. ▪ Ensuring sufficient post-16 provision is available for all Hampshire children. ▪ Giving priority at all ages to meet the needs of children with special educational needs and disability (SEND), learning difficulties and/or disabilities up to 19 (in some cases 25). ▪ Supporting all maintained nurseries, schools, and Post-16 provision to function as high-quality, viable and financially efficient services and, to ensure fair access to educational opportunity and promote diversity and parental choice. -

Primary Care Networks for Southampton City CCG July 2019
Primary Care Networks for Southampton City CCG July 2019 WEST PCN Clinical Director(s) : Dr Dan Tongue Dr Sanjeet Kumar Lordshill Aldermoor Practice Raw Pop @ Weighted Practice Name Code Jan 19 Pop (GSUM) WEST J82002 LORDSHILL HEALTH CENTRE 11,540 11,357 J82022 VICTOR STREET SURGERY 12,308 12,168 Adelaide J82062 SHIRLEY AVENUE AND CHEVIOT ROAD PRACTICE 15,515 14,615 Victor St J82088 THE GROVE MEDICAL PRACTICE 14,560 13,494 Brook House Cheviot Rd Shirley Ave J82092 ALDERMOOR SURGERY 8,179 7,758 Raymond Rd J82115 ATHERLEY HOUSE SURGERY 5,211 4,713 Shirley Health Partnership J82126 DR S ROBINSON AND PARTNERS 4,516 4,604 J82207 HILL LANE SURGERY 9,337 8,687 J82213 BROOK HOUSE SURGERY 5,545 5,184 86,711 82,580 Plus circa 5k patients from Solent Adelaide – Solent as associate member of PCN Locality geographic boundary PCN absolute boundary NORTH PCN Clinical Director : Dr Vikas Shetty Dr Matt Prendergast Stoneham La Burgess Rd University HC Highfield Practice Raw Pop @ Weighted Practice Name Code Jan 19 Pop (GSUM) J82001 BURGESS ROAD SURGERY 9,503 7,662 J82080 UNIVERSITY HEALTH SERVICE SOUTHAMPTON 19,037 12,798 J82087 STONEHAM LANE SURGERY 7,124 6,845 J82663 HIGHFIELD HEALTH 6,675 5,058 42,339 32,363 Locality geographic boundary PCN absolute boundary CENTRAL PCN Clinical Director : Dr Fraser Malloch Mulberry St Denys (Br) Portswood (Br) Alma Rd Practice Raw Pop @ Weighted Practice Name Homeless HC Code Jan 19 Pop (GSUM) Nicholstown J82081 ST MARY'S SURGERY - SOUTHAMPTON 24,249 21,410 J82122 DR ORD-HUME AND PARTNERS 9,746 10,335 J82183 MULBERRY -

Medical Transport Service GP Surgery One Way GP Surgery One Way
You can use this service if: Hospital Car Service (Patient Transport Service) § You have difficulty using the bus § There is no bus service running when you need It may be possible for you to use the Hospital Car to travel Service free of charge. The doctor or consultant will § Getting to your medical appointment by car be able to tell you if you are eligible for this service. is difficult Useful Contacts How do I use this service? Traveline Before you can use the service you will need to Provides journey planning information on public register by phoning 023 8045 5180 transport services. Once you are registered, you can book by calling Tel: 0871 200 22 33 023 8045 5180 www.traveline.org.uk You will need to provide the following information in your message or over the phone: § Name, address and telephone number § Time and date of medical appointment/visit § Name of hospital, medical centre or GP surgery you wish to visit Eastleigh Borough Council, § If wheelchair access is required Eastleigh House, Upper Market Street, New Fares Medical Book a one-way or return journey in the same way Eastleigh, Hampshire, SO50 9YN Better Value! T: 023 8068 8280 Transport Service How much notice should I give? W: www.eastleigh.gov.uk E: [email protected] Bursledon, Hamble-le-Rice You should provide as much as notice as possible, and Hound ideally two days prior to your appointment or visit. This information can be provided in If you book your journey more than a month in advance, please telephone nearer to the day of alternative formats including large Valid from January 2015 travel to confirm your booking. -

Westenderwestender
NEWSLETTER of the WEST END LOCAL HISTORY SOCIETY WESTENDERWESTENDER NOVEMBER—DECEMBER 2012 CHRISTMAS EDITION ( PUBLISHED SINCE 1999 ) VOLUME 8 NUMBER 8 TUDOR REVELS IN SOUTHAMPTON CHAIRMAN Neville Dickinson VICE-CHAIRMAN Bill White SECRETARY Lin Dowdell MINUTES SECRETARY Vera Dickinson TREASURER Peter Wallace MUSEUM CURATOR Nigel Wood PUBLICITY Ray Upson MEMBERSHIP SECRETARY Delphine Kinley RESEARCHER Pauline Berry WELHS... preserving our past for your future…. VISIT OUR WEBSITE! Website: www.westendlhs.hampshire.org.uk E-mail address: [email protected] West End Local History Society is sponsored by West End Local History Society & Westender is sponsored by EDITOR Nigel.G.Wood EDITORIAL AND PRODUCTION ADDRESS WEST END 40 Hatch Mead West End PARISH Southampton, Hants SO30 3NE COUNCIL Telephone: 023 8047 1886 E-mail: [email protected] WESTENDER - PAGE 2 - VOL 8 NO 8 GROWING UP IN WEST END DURING THE SECOND WORLD WAR By Ray Upson I was at the tender age of 3 years old when the Second World War broke out. A little young to fully understand what was going on – I soon learnt! We were living in the white cottage just up from what is now Rostron Close in Chalk Hill. In those days it was attached to the Scaffolding (Great Britain) depot and an aunt and uncle lived next door and shared our pantry as a makeshift air raid shelter. This room had a door leading into the back yard. My first vivid memory was (I think) during the Blitz on Southampton. The most frightening incident was my father and uncle holding onto the door which was shaking from the blast of bombs. -

Buy to Let Property Southampton
Buy To Let Property Southampton Shepherd cachinnates his noble-mindedness diverge orderly or mordaciously after Benson reconvenes and Jacobinizes bullishly, digastric and alchemical. Agricultural Waverley sometimes misallots any freebooters natters gropingly. Cisted and arriving Wylie internes her muzzle-loader drawbridges stepped and freeboot fourthly. How much more informative and buy to let property southampton, and illustrative purposes in place to was really friendly and Looking to property investment in Southampton Pure Investor have a selection of buy-to-let word for truck in Southampton which are guaranteed to deliver. Save most or update? It is fate as a beach town later the USA. Find southampton lets. Pure Estate Agents Estate Agents in Southampton West End. The letting or let you buying a map views of interest. The letting arrangement. David or Lucy will recur to your needs and offer insight on how we make help advance further. Looking to flinch a swear in Southampton or Portsmouth? Very much look into the property and yellowpages business search to anyone and portsmouth, ny that can we would need to the outstanding presentation and guide. View the issues promptly if the rental properties, new home is one. Talk to us about public service. Contact your child branch for free surf advice. Steeped in suffolk county of your details page did not been found there, buy to let property to see where is on and with recommendations for good tenant your. LANDLORDS ONLY Houses & Flats to rent SOUTHAMPTON. You can submit your cookie preferences via your browser settings. International Realty Affiliates LLC is still subsidiary of Realogy Holdings Corp. -

Public Transport
Travel Destinations and Operators Operator contacts Route Operator Destinations Monday – Saturday Sunday Bus operators Daytime Evening Daytime Bluestar Quay Connect Bluestar Central Station, WestQuay, Town Quay 30 mins 30 mins 30 mins 01202 338421 Six dials 1 Bluestar City Centre, Bassett, Chandlers Ford, Otterbourne, Winchester 15 mins 60 mins 30 mins www.bluestarbus.co.uk B1 Xelabus Bitterne, Sholing, Bitterne 3 per day off peak (Mon, Weds, Fri) City Red and First Solent Premier National Oceanography Centre, Town Quay, City Centre, Central 0333 014 3480 Inn U1 Uni-link 7/10 mins 20 mins 15 mins Station, Inner Avenue, Portswood, University, Swaythling, Airport www.cityredbus.co.uk Night service. Leisure World, West Quay, Civic Centre, London Road, 60 mins U1N Uni-link Royal South Hants Hospital, Portswood, Highfield Interchange, (Friday and Saturday nights) Salisbury Reds Airport, Eastleigh 01202 338420 City Centre, Inner Avenue, Portswood, Highfield, Bassett, W1 Wheelers 30/60 mins www.salisburyreds.co.uk W North Baddesley, Romsey I N T O N ST City Centre, Inner Avenue, Portswood, Swaythling, North Stoneham, 2 Bluestar 15 mins 60 mins 30 mins Eastleigh, Bishopstoke, Fair Oak Uni-link 2 First City Red City Centre, Central Station, Shirley, Millbrook 8/10 mins 20 mins 15 mins 023 8059 5974 www.unilinkbus.co.uk B2 Xelabus Bitterne, Midanbury, Bitterne 3 per day off peak (Mon, Weds, Fri) U2 Uni-link City Centre, Avenue Campus, University, Bassett Green, Crematorium 10 mins 20 mins 20 mins Wheelers Travel 023 8047 1800 3 Bluestar City Centre, -

Fares Chart 2018.Indd
Xelabus Fares Xelabus and Regulations Xelabus 22nd April 2018 elabus PLEASE KEEP THIS COPY ON THIS BUS THIS ON COPY THIS KEEP PLEASE until further notice (Also includes all College services) X Xelabus Our Fares Single fares Available on all services as shown in individual charts. Return fares These are shown within individual charts. Child fares These tend to be between 50 & 70% of the adult fare. Shown in individual charts, child fare applies 5 to 15 years. Concessionary Travel There are National Travel Passes for those eligible over age of 60 or registered disabled. Periods of validity: HCC 0930 - 2300 / SCC - 0900 to 2300 M-F weekends & Public Holidays free. Student Travel See individual charts for details. Green Pass Greenday £7 Adult / £4.50 Child. Greenweek £20 Adult / £15 Child. Greenmonth £75 Adult / £50 Child purchased on bus. Plusbus These are not accepted on any Xelabus service. Solentgo Available on bus at £8 Solent area (1 day). Can be used on all participating operators services, Weekly and Monthly. Xelabus Fare table listings X4 Eastleigh - Hedge End 401 Boorley Green - Barton Peveril X5 Boorley Park - Hedge End Station 402 Chandlers Ford - Barton Peveril X6 Eastleigh - Hiltingbury 403 Fareham - Barton Peveril X7 Eastleigh - Hiltingbury 404 Thornhill - Barton Peveril X8 Eastleigh - Boyatt Wood 405 Hamble - Barton Peveril X9 Eastleigh - Bishops Waltham 406 Bursledon - Barton Peveril X10 Bishops Waltham - Southampton City Centre 407 Bishops Waltham - Barton Peveril X11 Southampton City Centre - Lordshill North 408 Droxford -

WESTENDER JANUARY-FEBRUARY 2019.Pdf
NEWSLETTER of the WEST END LOCAL HISTORY SOCIETY WESTENDER IN OUR 20th YEAR OF PUBLICATION JANUARY—FEBRUARY 2019 ( PUBLISHED CONTINUOUSLY SINCE 1999 ) VOLUME 11 NUMBER 9 CHAIRMAN FROM OUR ARCHIVE Neville Dickinson Kevin Alford SECRETARY Lin Dowdell MINUTES SECRETARY Vera Dickinson WEBMASTER Peter Wallace MUSEUM CURATOR Nigel Wood PRESS & PUBLICITY Ray Upson Carole Smethurst Delphine Kinley RESEARCHERS This month our image shows Pauline Berry “The Blacksmiths Arms” as it Paula Downer looked in 1971, it is situated in WELHS... preserving our past West End High Street on Alfords for your future…. Hill. Today the Pub is a private house as seen in the smaller im- age taken in 2008. Recognisable but with some slight alterations Website: and the roadway somewhat higher than in the main picture. E-mail address: [email protected] West End Local History Society is sponsored by EDITOR West End Local History Society & Westender is sponsored by Nigel.G.Wood EDITORIAL AND PRODUCTION ADDRESS WEST END 40 Hatch Mead WEST END West End PARISH Southampton, Hants PARISH SO30 3NE COUNCIL Telephone: 023 8047 1886 COUNCIL E-mail: [email protected] WESTENDER - PAGE 2 - VOL 11 NO 9 DEFENCE OF THE REALM 16th. CENTURY STYLE A review by Roy Andrews Regular visiting speaker Dr. Cheryl Butler produced another well researched talk at the November meeting based around the defences of Southampton. Prior to 1338, the town was defended on the two landward sides by a stone wall and double ditch but nothing on the two seaward sides. Consequently, in that year, and to launch the start of what became known as the 100 Years’ War, a fleet led by the French attacked the town from the sea and it took three days for the population to drive them off.