Primary Care in Southampton - August 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Mileage and Admissions
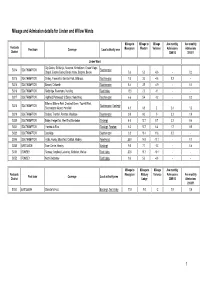
Mileage and Admission details for Linden and Willow Wards Mileage to Mileage to Mileage Ave monthly Ave monthly Postcode Post town Coverage Local authority area Moorgreen Western Variance Admissions Admissions District 2009/10 2010/11 Linden Ward City Centre, St. Mary's, Newtown, Nicholstown, Ocean Village, SO14 SOUTHAMPTON Southampton Chapel, Eastern Docks, Bevois Valley, Bargate, Bevois 5.6 5.0 -0.6 - 0.2 SO15 SOUTHAMPTON Shirley, Freemantle, Banister Park, Millbrook, Southampton 7.6 3.0 -4.6 0.2 - SO16 SOUTHAMPTON Bassett, Chilworth Southampton 8.4 3.5 -4.9 - 0.1 SO16 SOUTHAMPTON Redbridge, Rownhams, Nursling Test Valley 13.0 2.0 -11 - - SO17 SOUTHAMPTON Highfield, Portswood, St Denys, Swaythling Southampton 6.6 5.4 -1.2 - 0.2 Bitterne, Bitterne Park, Chartwell Green, Townhill Park, SO18 SOUTHAMPTON Southampton , Eastleigh Southampton Airport, Harefield 4.5 6.5 2 2.4 1.2 SO19 SOUTHAMPTON Sholing, Thornhill, Peartree, Woolston Southampton 9.0 9.0 0 3.2 1.9 SO30 SOUTHAMPTON Botley, Hedge End, West End, Bursledon Eastleigh 4.0 12.7 8.7 2.2 0.4 SO31 SOUTHAMPTON Hamble-le-Rice Eastleigh , Fareham 6.3 12.7 6.4 1.7 0.5 SO32 SOUTHAMPTON Curdridge Southampton 3.8 15.4 11.6 0.2 - SO45 SOUTHAMPTON Hythe, Fawley, Blackfield, Calshot, Hardley New Forest 25.9 14.8 -11.1 - 0.1 SO50 EASTLEIGH Town Centre, Hamley Eastleigh 9.0 7.7 -1.3 - 0.6 SO51 ROMSEY Romsey, Ampfield, Lockerley, Mottisfont, Wellow Test Valley 20.8 10.7 -10.1 - - SO52 ROMSEY North Baddesley Test Valley 9.6 5.0 -4.6 - - Mileage to Mileage to Mileage Ave monthly Postcode Moorgreen Melbury Variance Admissions Ave monthly Post town Coverage Local authority area District Lodge 2009/10 Admissions 2010/11 SO53 EASTLEIGH Chandler's Ford Eastleigh , Test Valley 11.0 9.0 -2 1.8 0.6 1 Mileage to Mileage to Mileage Ave monthly Ave monthly Postcode Post town Coverage Local authority area Moorgreen Western Variance Admissions Admissions District 2009/10 2010/11 Willow Ward City Centre, St. -

Neighbourhoods in England Rated E for Green Space, Friends of The
Neighbourhoods in England rated E for Green Space, Friends of the Earth, September 2020 Neighbourhood_Name Local_authority Marsh Barn & Widewater Adur Wick & Toddington Arun Littlehampton West and River Arun Bognor Regis Central Arun Kirkby Central Ashfield Washford & Stanhope Ashford Becontree Heath Barking and Dagenham Becontree West Barking and Dagenham Barking Central Barking and Dagenham Goresbrook & Scrattons Farm Barking and Dagenham Creekmouth & Barking Riverside Barking and Dagenham Gascoigne Estate & Roding Riverside Barking and Dagenham Becontree North Barking and Dagenham New Barnet West Barnet Woodside Park Barnet Edgware Central Barnet North Finchley Barnet Colney Hatch Barnet Grahame Park Barnet East Finchley Barnet Colindale Barnet Hendon Central Barnet Golders Green North Barnet Brent Cross & Staples Corner Barnet Cudworth Village Barnsley Abbotsmead & Salthouse Barrow-in-Furness Barrow Central Barrow-in-Furness Basildon Central & Pipps Hill Basildon Laindon Central Basildon Eversley Basildon Barstable Basildon Popley Basingstoke and Deane Winklebury & Rooksdown Basingstoke and Deane Oldfield Park West Bath and North East Somerset Odd Down Bath and North East Somerset Harpur Bedford Castle & Kingsway Bedford Queens Park Bedford Kempston West & South Bedford South Thamesmead Bexley Belvedere & Lessness Heath Bexley Erith East Bexley Lesnes Abbey Bexley Slade Green & Crayford Marshes Bexley Lesney Farm & Colyers East Bexley Old Oscott Birmingham Perry Beeches East Birmingham Castle Vale Birmingham Birchfield East Birmingham -

ITEM NO: C2a APPENDIX 1
ITEM NO: C2a APPENDIX 1 Background Information Approximately 3600 flats and houses were built in Southampton in the five year period up to March 2006. About 80% of these were flats. Some 25% of these flats and houses were in the city centre, where the on-street parking facilities are available to everyone on a "Pay and Display" basis. Outside the central area, only about 10% of the city falls within residents' parking zones. So, out of the 3600 properties in all, it is estimated that only about 270 (or 7.5%) will have been within residents' parking zones and affected by the policy outlined in the report. Only in a few (probably less than 20) of these cases have difficulties come to light. In general, there is no question of anyone losing the right to a permit, although officers are currently seeking to resolve a situation at one particular development where permits have been issued in error. There are currently 13 schemes funded by the City Council and these cover the following areas:- Polygon Area Woolston North Woolston South Newtown/Nicholstown Bevois Town Freemantle Coxford (General Hospital) Shirley University Area (5 zones) These schemes operate from 8 a.m. to 6 p.m. on weekdays and, in some cases, at other times as well. In addition, there are three further schemes at Bitterne Manor, Itchen and Northam that only operate during football matches or other major events at St Mary’s Stadium. These are funded by Southampton Football Club. Within all these schemes, parking bays are marked on the road for permit holders, often allowing short-stay parking by other users as well. -

1992 Southampton Wildlife Link Peartree Green
,~ ,,-_ /,,- 1 1 ' /.....,;l A NATURAL HISTORY \....,;' OF PEARTREE GREEN I ' I I ..._._ - .. - A REPORT BY SOUTHAMPTON WILDLIFE LINK •b... -. _' ....... ._J Broadlands Valley Conservation Group, Hampshire Badger Link, Hampshire & lOW I 1 ." Naturalist's Trust, Southampton Commons and Parks Protection Society, .. - Southampton Natural History Society, Southampton Schools Conservation Corps, Hawthorns Wildlife Association, British Butterfly Conservation Society, R.S.P.B. ..._ British Trust for 'Ornithology, English Nature . Hon. Sec. Mrs P. Loxton, 3 Canton St, Southampton J February 1992 - /~ c !-> r=f. ~- ; j L - I 1 I....,. -. I ~ l -~ 1- 1-' L,' - j - Q L c_, 1 Field Rose 5 • 2 Soapwort L s: 3 Hedge B'r o wn . Butterfly . ~4 4 White Mullein L ~ . A3 5 Small Heath Butterfly ~ 6 Field Scabious i .. 7 Musk Mallow '-- ' ~J('.~ ~ . 8 Common Mallow 9 Field Grasshopper ( ,, . 10 Restharrow .._ ~ f:\f)~~lftBfiB ;.,r~._6 11 Kidney Vetch J - ... ;;1~11 ~ 9 j , ~ II 'IlI_ ~UI II. ~.r-'L-I ~~,,~,J J' L --- -- • -.. -I ,~ .,_;'\ , -" ~ -. , . .' o - _J --.. I r-« / -.... Pear tree I G..~_Green ......., I ~ j--'" ,.-... ,. --. I /-.. - - j J ~.,7~~ /- I -I SOUTHAMPTON WILDLIFE LINK I THE" NATURAL HISTORY OF PEARTREE GREEN 1....1 .. , A REPORT I I INTRODUCTION - Peartree Green is a remnant of the Ridgeway Heath that today consists of two parts; the original "village green" (express-ly excluded from. the L enolosure of common land c 1814) and the land below it that is bounded by the railway and Sea Roatl. The Old Common has long been valued as a recreational I L amenity. It was safeguarded from encroachment in 1872 by a Court of Chancery Award, and was duly registered under the 1965 Commons Registration Act as a Town Green. -

Primary Care Networks for Southampton City CCG July 2019
Primary Care Networks for Southampton City CCG July 2019 WEST PCN Clinical Director(s) : Dr Dan Tongue Dr Sanjeet Kumar Lordshill Aldermoor Practice Raw Pop @ Weighted Practice Name Code Jan 19 Pop (GSUM) WEST J82002 LORDSHILL HEALTH CENTRE 11,540 11,357 J82022 VICTOR STREET SURGERY 12,308 12,168 Adelaide J82062 SHIRLEY AVENUE AND CHEVIOT ROAD PRACTICE 15,515 14,615 Victor St J82088 THE GROVE MEDICAL PRACTICE 14,560 13,494 Brook House Cheviot Rd Shirley Ave J82092 ALDERMOOR SURGERY 8,179 7,758 Raymond Rd J82115 ATHERLEY HOUSE SURGERY 5,211 4,713 Shirley Health Partnership J82126 DR S ROBINSON AND PARTNERS 4,516 4,604 J82207 HILL LANE SURGERY 9,337 8,687 J82213 BROOK HOUSE SURGERY 5,545 5,184 86,711 82,580 Plus circa 5k patients from Solent Adelaide – Solent as associate member of PCN Locality geographic boundary PCN absolute boundary NORTH PCN Clinical Director : Dr Vikas Shetty Dr Matt Prendergast Stoneham La Burgess Rd University HC Highfield Practice Raw Pop @ Weighted Practice Name Code Jan 19 Pop (GSUM) J82001 BURGESS ROAD SURGERY 9,503 7,662 J82080 UNIVERSITY HEALTH SERVICE SOUTHAMPTON 19,037 12,798 J82087 STONEHAM LANE SURGERY 7,124 6,845 J82663 HIGHFIELD HEALTH 6,675 5,058 42,339 32,363 Locality geographic boundary PCN absolute boundary CENTRAL PCN Clinical Director : Dr Fraser Malloch Mulberry St Denys (Br) Portswood (Br) Alma Rd Practice Raw Pop @ Weighted Practice Name Homeless HC Code Jan 19 Pop (GSUM) Nicholstown J82081 ST MARY'S SURGERY - SOUTHAMPTON 24,249 21,410 J82122 DR ORD-HUME AND PARTNERS 9,746 10,335 J82183 MULBERRY -

U6H Bus Time Schedule & Line Route
U6H bus time schedule & line map U6H Highƒeld View In Website Mode The U6H bus line (Highƒeld) has 2 routes. For regular weekdays, their operation hours are: (1) Highƒeld: 11:35 PM (2) Lordswood: 6:01 AM - 10:35 PM Use the Moovit App to ƒnd the closest U6H bus station near you and ƒnd out when is the next U6H bus arriving. Direction: Highƒeld U6H bus Time Schedule 27 stops Highƒeld Route Timetable: VIEW LINE SCHEDULE Sunday 11:35 PM Monday 11:35 PM Southampton Nocs, Eastern Docks Tuesday 11:35 PM Platform Tavern, Town Quay Wednesday 11:35 PM Telephone House, Town Quay Thursday 11:35 PM High Street, Southampton Friday 11:35 PM Holyrood Church, Southampton City Centre 135 High Street, Southampton Saturday 11:35 PM Westquay, Southampton City Centre Portland Terrace, Southampton Asda & Marlands, Southampton City Centre U6H bus Info Direction: Highƒeld Civic Centre, Southampton City Centre Stops: 27 Windsor Terrace, Southampton Trip Duration: 27 min Line Summary: Southampton Nocs, Eastern Docks, Park Walk, Southampton City Centre Platform Tavern, Town Quay, Telephone House, Town Quay, Holyrood Church, Southampton City Centre, Solent University, Southampton City Centre Westquay, Southampton City Centre, Asda & Marlands, Southampton City Centre, Civic Centre, Rsh Hospital, Nicholstown Southampton City Centre, Park Walk, Southampton St Marys Road, Southampton City Centre, Solent University, Southampton City Centre, Rsh Hospital, Nicholstown, Denzil Avenue, Denzil Avenue, Bevois Valley Bevois Valley, Aldi Store, Bevois Valley, Spring 54 Onslow -

Board of Directors
February 2020 Board of Directors Non Executive Directors Executive Directors Non Executive Chief Executive Chief Finance Officer Chair Director Officer and Deputy CEO Catherine Mason Jon Pittam Sue Harriman Andrew Strevens Non Executive Non Executive Interim Medical Chief Nurse Director Director Director Jackie Ardley Mike Watts Stephanie Elsy Dr Jonathan Prosser Non Executive Non Executive Chief People Officer Director Director Helen Ives Gaurav Kumar Thoreya Swage Chief Operating Chief Operating Officer Portsmouth Officer Southampton and Commercial and County Services Director David Noyes Sarah Austin (non voting) (non voting) Executive Assistant to Chief Executive Chief Executive Officer Executive Team Belinda Brown Sue Harriman February 2020 Structure Strategy Chair Accountable Officer Catherine Mason Statutory roles *PSEH ICS System Convener *Chair Local Workforce Action Board System / other (LWAB) appointed roles *SRO STP Workforce *Member STP Exec Delivery Group Working with the Executive Team: Chief Operating Chief Operating Associate Director of Chief Finance Officer Interim Medical Officer Southampton Officer Portsmouth & Corporate Affairs & and Deputy CEO Chief Nurse Director Chief People Officer & County Services Commercial Director Company Secretary Andrew Strevens Jackie Ardley Jonathan Prosser Helen Ives David Noyes Sarah Austin Rachel Cheal Professional lead Doctors Operational lead for Clinical and Dentists Services – Southampton and Operational lead for Clinical Professional lead Nurses and County wide services Services -

Ward Councilors: (See Also Google Map)
Ward Councilors: (See also Google Map) Name Ward/Next standing Party Councillor Sarah Bogle Bargate ‘18 L Councillor John Noon Bargate ‘19 L Councillor Darren Paffey Bargate ‘20 L Councillor Beryl Harris Bassett ‘18 C Councillor Les Harris Bassett ‘19 C Councillor John Hannides Bassett ‘20 C Councillor Derek Burke Bevois ‘18 L Councillor Jacqui Rayment Bevois ‘19 L Councillor Stephen Barnes-Andrews Bevois ‘20 L Councillor Simon Letts Bitterne ‘18 L Councillor John Jordan Bitterne ‘19 L Councillor Frances Murphy - New Bitterne ‘20 L Councillor John Inglis Bitterne Park ‘18 C Councillor David Fuller Bitterne Park ‘19 C Councillor Ivan White Bitterne Park ‘20 C Councillor Keith Morrell Coxford ’18 IL Councillor Don Thomas Coxford ‘19 IL Councillor Tammy Thomas - New Coxford ‘20 IL Councillor Jeremy Moulton Freemantle ‘18 C Councillor Brian Parnell Freemantle ‘19 C Councillor David Shields Freemantle ‘20 L Councillor Val Laurent - New Harefield ‘18 C Councillor Daniel Fitzhenry Harefield ‘19 C Councillor Peter Baillie Harefield ‘20 C Councillor Mike Denness Millbrook ‘18 L Councillor David Furnell Millbrook ‘19 L Councillor Sarah Taggart - New Millbrook ‘20 L Councillor Paul Lewzey Peartree ‘18 L Councillor Alex Houghton Peartree ‘19 C Councillor Eammonn Keogh Peartree ‘20 L Councillor Paul O’Neill Portswood ‘18 C Councillor Matthew Claisse Portswood ‘19 C Councillor John Savage - New Portswood ‘20 L Councillor Cathie McEwing Redbridge ‘18 L Councillor Andrew Pope Redbridge ‘19 IL Councillor Lee Whitbread Redbridge ‘20 L Councillor Hannah Coombs Shirley ‘18 L Councillor Satvir Kaur Shirley ‘19 L Councillor Mark Chaloner Shirley ’20 L Councillor Nigel Hecks Sholing ‘18 C Councillor Graham Wilkinson Sholing ‘19 C Councillor James Baillie - New Sholing ‘20 C Councillor Bob Painton Swaythling ‘18 C Councillor Spiros Vassiliou Swaythling ‘19 C Councillor Sharon Mintoff Swaythling ‘20 L Councillor Sue Blatchford Woolston ‘18 L Councillor Warwick Payne Woolston ‘19 L Councillor Christopher Hammond Woolston ‘20 L . -

223 Peartree Avenue Bitterne Southampton SO19 7RD
223 Peartree Avenue Bitterne Southampton SO19 7RD 223 Peartree Avenue Bitterne Southampton SO19 7RD £335,000 INTRODUCTION A beautifully presented and thoughtfully extended family home, situated in the very heart of Bitterne's thriving town centre. The property has a lovely light and airy feel throughout with accommodation on the ground floor briefly comprising a lovely bright sitting room, with an attractive bay window and wood burning stove, dining room, family room, modern cloakroom and 20ft kitchen/breakfast room. On the first floor there are then three well-proportioned bedrooms, a beautifully appointed bathroom with additional benefits including a driveway providing ample off road parking for two cars, covered patio area and an attractive garden. To fully appreciate both the accommodation on offer and the property's location, an early viewing is a must. LOCATION The property is only a short walk away from Bitterne's infant and junior schools along with being only a short stroll away from Bitterne's broad range of shops and amenities. Southampton with its vibrant city centre is also close by, as is Hamble and its marina, as well as the Royal Victoria Country Park which is set in over two hundred acres of grassy parkland and woodland. All main motorway access routes are also within easy reach, enabling easy access to Portsmouth, Fareham and Winchester. INSIDE The property is approached via a driveway leading to an attractive double glazed front door with diamond style double glazed windows, which then opens directly through to a lovely bright entrance hall with ceramic tiled flooring, stairs leading to the first floo r, an under stairs cupboard providing useful storage space and a door leading through to a modern downstairs cloakroom. -

Southampton Forest Hills Driving Test Centre Routes
Southampton Forest Hills Driving Test Centre Routes To make driving tests more representative of real-life driving, the DVSA no longer publishes official test routes. However, you can find a number of recent routes used at the Southampton Forest Hills driving test centre in this document. While test routes from this centre are likely to be very similar to those below, you should treat this document as a rough guide only. Exact test routes are at the examiners’ discretion and are subject to change. Route Number 1 Road Direction Driving Test Centre Left Forest Hills Drive Mini roundabout right Woodmill Lane Mini roundabout ahead Woodmill Lane Traffic light left Portswood Rd Right Harefield Rd End of road left Woodcote Rd Left Harrison Rd End of road right Woodcote Rd End of road left Burgess Rd Right Tulip Rd End of road left Honeysuckle Rd Right Daisy Rd/Lobelia Rd End of road left Bassett Green Rd Roundabout left Bassett Avenue Roundabout ahead, 2nd traffic light left Highfield Avenue/Highfield Lane Mini roundabout ahead Highfield Lane Traffic light crossroads right Portswood Rd Traffic light ahead, traffic light left Slip Rd Left Thomas Lewis Way Traffic light ahead, traffic light right St Denys Rd/Cobden Bridge Traffic light left Manor Farm Rd Mini roundabout right Woodmill Lane Mini roundabout left Forest Hills Drive Right Driving Test Centre Route Number 2 Road Direction Driving Test Centre Right Forest Hills Drive/Meggeson Avenue End of road right Townhill Way Roundabout left West End Rd Right Hatley Rd/Taunton Drive Left Somerton -

Final Recommendations on the Future Electoral Arrangements for Southampton in Hampshire
Final recommendations on the future electoral arrangements for Southampton in Hampshire Report to the Secretary of State for the Environment, Transport and the Regions July 2000 LOCAL GOVERNMENT COMMISSION FOR ENGLAND LOCAL GOVERNMENT COMMISSION FOR ENGLAND This report sets out the Commission’s final recommendations on the electoral arrangements for the city of Southampton in Hampshire. Members of the Commission are: Professor Malcolm Grant (Chairman) Professor Michael Clarke CBE (Deputy Chairman) Peter Brokenshire Kru Desai Pamela Gordon Robin Gray Robert Hughes CBE Barbara Stephens (Chief Executive) © Crown Copyright 2000 Applications for reproduction should be made to: Her Majesty’s Stationery Office Copyright Unit. The mapping in this report is reproduced from OS mapping by the Local Government Commission for England with the permission of the Controller of Her Majesty’s Stationery Office, © Crown Copyright. Unauthorised reproduction infringes Crown Copyright and may lead to prosecution or civil proceedings. Licence Number: GD 03114G. This report is printed on recycled paper. Report no: 165 ii LOCAL GOVERNMENT COMMISSION FOR ENGLAND CONTENTS page LETTER TO THE SECRETARY OF STATE v SUMMARY vii 1 INTRODUCTION 1 2 CURRENT ELECTORAL ARRANGEMENTS 5 3 DRAFT RECOMMENDATIONS 9 4 RESPONSES TO CONSULTATION 11 5 ANALYSIS AND FINAL RECOMMENDATIONS 13 6 NEXT STEPS 29 APPENDIX A Draft Recommendations for Southampton (January 2000) 31 A large map illustrating the proposed ward boundaries for Southampton is inserted inside the back cover of this report. LOCAL GOVERNMENT COMMISSION FOR ENGLAND iii iv LOCAL GOVERNMENT COMMISSION FOR ENGLAND Local Government Commission for England 25 July 2000 Dear Secretary of State On 20 July 1999 the Commission began a periodic electoral review of Southampton under the Local Government Act 1992. -
Declaration of Result of Poll
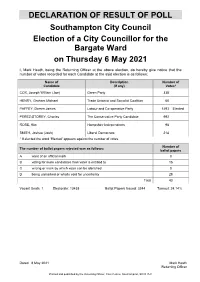
DECLARATION OF RESULT OF POLL Southampton City Council Election of a City Councillor for the Bargate Ward on Thursday 6 May 2021 I, Mark Heath, being the Returning Officer at the above election, do hereby give notice that the number of votes recorded for each Candidate at the said election is as follows: Name of Description Number of Candidate (if any) Votes* COX, Joseph William (Joe) Green Party 338 HENRY, Graham Michael Trade Unionist and Socialist Coalition 66 PAFFEY, Darren James Labour and Co-operative Party 1493 Elected PEREZ-STOREY, Charles The Conservative Party Candidate 992 ROSE, Kim Hampshire Independents 98 SMITH, Joshua (Josh) Liberal Democrats 214 * If elected the word 'Elected' appears against the number of votes. Number of The number of ballot papers rejected was as follows: ballot papers A want of an official mark 0 B voting for more candidates than voter is entitled to 15 C writing or mark by which voter can be identified 0 D being unmarked or wholly void for uncertainty 28 Total 43 Vacant Seats: 1 Electorate: 13438 Ballot Papers Issued: 3244 Turnout: 24.14% Dated 8 May 2021 Mark Heath Returning Officer Printed and published by the Returning Officer, Civic Centre, Southampton, SO14 7LY DECLARATION OF RESULT OF POLL Southampton City Council Election of a City Councillor for the Bassett Ward on Thursday 6 May 2021 I, Mark Heath, being the Returning Officer at the above election, do hereby give notice that the number of votes recorded for each Candidate at the said election is as follows: Name of Description Number of Candidate (if any) Votes* BLACKMAN, Richard Liberal Democrat 1373 GORE, Stephen George (Steve) Green Party 204 HANNIDES, John Michael Local Conservatives 1795 Elected MARX, Michael (Mike) Trade Unionist and Socialist Coalition 24 MINTO, Ashley Mark Labour Party 614 * If elected the word 'Elected' appears against the number of votes.