Expert Roundtable Meeting: Use of Cough Suppressants in Children
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Appendix a Common Abbreviations Used in Medication
UNIVERSITY OF AMSTERDAM MASTERS THESIS Impact of Medication Grouping on Fall Risk Prediction in Elders: A Retrospective Analysis of MIMIC-III Critical Care Database Student: SRP Mentor: Noman Dormosh Dr. Martijn C. Schut Student No. 11412682 – SRP Tutor: Prof. dr. Ameen Abu-Hanna SRP Address: Amsterdam University Medical Center - Location AMC Department Medical Informatics Meibergdreef 9, 1105 AZ Amsterdam Practice teaching period: November 2018 - June 2019 A thesis submitted in fulfillment of the requirements for the degree of Master of Medical Informatics iii Abstract Background: Falls are the leading cause of injury in elderly patients. Risk factors for falls in- cluding among others history of falls, old age, and female gender. Research studies have also linked certain medications with an increased risk of fall in what is called fall-risk-increasing drugs (FRIDs), such as psychotropics and cardiovascular drugs. However, there is a lack of consistency in the definitions of FRIDs between the studies and many studies did not use any systematic classification for medications. Objective: The aim of this study was to investigate the effect of grouping medications at different levels of granularity of a medication classification system on the performance of fall risk prediction models. Methods: This is a retrospective analysis of the MIMIC-III cohort database. We created seven prediction models including demographic, comorbidity and medication variables. Medica- tions were grouped using the anatomical therapeutic chemical classification system (ATC) starting from the most specific scope of medications and moving up to the more generic groups: one model used individual medications (ATC level 5), four models used medication grouping at levels one, two, three and four of the ATC and one model did not include med- ications. -

Medicare Part D Excluded Drug List
MEDICARE PART D EXCLUDED DRUGS LIST 2016_updated July 2016 Reason: LIST = multiple reasons it's excluded; "not covered under Part D law" Reason: Not properly listed with FDA = CMS considers it best practice for Part D sponsors to consider the proper listing of a drug product with the FDA as a prerequisite for making a Part D drug coverage determination. The FDA is unable to provide regulatory status determinations through their regular processes if a drug product is not properly listed. Therefore, Part D sponsors should begin the drug coverage determination process by confirming that a prescription drug product national drug code (NDC) is properly listed with the FDA. Reason: DESI = Less Than Effective (LTE) drug for ALL indications Label Name Reason 1ST BASE CRE Bulk Ingredient 2-FUCCOSYLLA PAK LACTO-N Medical Food ABANEU-SL SUB Vitamin/Mineral ABLAVAR INJ 244MG/ML Diagnostic Agent ACACIA EXTRA SOL 1:20 Non-standardized allergenic ACCUCAINE INJ 1% LIST ACD FORMULA SOL A Blood Component ACD-A SOL Blood Component ACLARO PD EMU 4% Cosmetic ACREMONIUM SOL 20000PNU Non-standardized allergenic ACTCT FLEX 3 PAD 4"X4" Not properly listed with FDA ACTHREL INJ 100MCG Diagnostic Agent ACTI ANTIMIC PAD 2"X2" Not properly listed with FDA ACTI ANTIMIC PAD 4"X4" Not properly listed with FDA ACTICOAT 7 PAD 2"X2" Not properly listed with FDA ACTICOAT 7 PAD 4"X5" Not properly listed with FDA ACTICOAT ABS PAD 4"X5" Not properly listed with FDA ACTICOAT MOI PAD 2"X2" Surgical Supply/Medical ACTICOAT MOI PAD 4"X4" Surgical Supply/Medical ACTICOAT MOI PAD -

Blue Cross and Blue Shield January 2018 5 Tier Basic Drug List
January 2018 5 Tier Basic Drug List Please consider talking to your doctor about prescribing preferred medications, which may help reduce your out-of-pocket costs. This list may help guide you and your doctor in selecting an appropriate medication for you. The drug list is regularly updated. You can view the most up-to-date list, or the specialty drug list, at MyPrime.com. Contents Therapeutic Class Drug List Introduction ....................................................... I Anti-Infective Agents ........................................ 1 How drugs are selected .................................... I Cancer Drugs ................................................... 3 How member payment is determined ............... I Hormones, Diabetes and Related Drugs ......... 5 How to use this list ............................................ I Heart and Circulatory Drugs ............................ 9 Generic drugs .................................................. II Respiratory Agents ........................................ 14 Coverage considerations ................................ III Gastrointestinal Drugs ................................... 16 Specialty drugs .............................................. IV Genitourinary Drugs ....................................... 17 Central Nervous System Drugs ..................... 1 Abbreviation/acronym key .............................. V 8 Pain Relief Drugs ........................................... 21 Neuromuscular Drugs .................................... 23 Supplements ................................................. -

Inhibition of Cough-Reflex Sensitivity by Benzonatate and Guaifenesin In
Respiratory Medicine (2009) 103, 902e906 available at www.sciencedirect.com journal homepage: www.elsevier.com/locate/rmed Inhibition of cough-reflex sensitivity by benzonatate and guaifenesin in acute viral cough Peter V. Dicpinigaitis a,*, Yvonne E. Gayle a, Gail Solomon b, Richard D. Gilbert c a Albert Einstein College of Medicine and Montefiore Medical Center, 1825 Eastchester Road, Bronx, NY, 10461, USA b Reckitt Benckiser, Inc., 399 Interpace Parkway, Parsippany, NJ, 07054, USA c TKL Research, Inc., 365 West Passaic Street, Rochelle Park, NJ, 07662, USA Received 8 September 2008; accepted 9 December 2008 Available online 1 January 2009 KEYWORDS Summary Cough; Acute cough due to viral upper respiratory tract infection (URI) is the most common form of Antitussive; cough and accounts for tremendous expenditure on prescription and non-prescription cough Guaifenesin; products worldwide. However, few agents have been shown in properly conducted clinical Benzonatate; trials to be effective for cough due to URI. The present study evaluated the effect of benzo- Capsaicin; natate 200 mg (B), guaifenesin 600 mg (G), their combination (B þ G), and placebo (P) on Common cold capsaicin-induced cough in 30 adult nonsmokers with acute URI. On 3 separate days within a 7-day period, 1 h after ingesting randomly assigned study drug in a double-blind fashion, subjects underwent capsaicin cough challenge testing, which involved inhalation of incre- mental doubling concentrations of capsaicin until the concentration of capsaicin inducing 5 or more coughs (C5) was attained. Each subject received 3 of 4 possible study drugs. G (p Z 0.01) but not B (p Z NS) inhibited cough-reflex sensitivity (log C5)relativetoP.The combination of B þ G suppressed capsaicin-induced cough to a greater degree than B alone (p < 0.001) or G alone (p Z 0.008). -

Use of Antitussives After the Initiation of Angiotensin-Converting Enzyme Inhibitors
저작자표시-비영리-변경금지 2.0 대한민국 이용자는 아래의 조건을 따르는 경우에 한하여 자유롭게 l 이 저작물을 복제, 배포, 전송, 전시, 공연 및 방송할 수 있습니다. 다음과 같은 조건을 따라야 합니다: 저작자표시. 귀하는 원저작자를 표시하여야 합니다. 비영리. 귀하는 이 저작물을 영리 목적으로 이용할 수 없습니다. 변경금지. 귀하는 이 저작물을 개작, 변형 또는 가공할 수 없습니다. l 귀하는, 이 저작물의 재이용이나 배포의 경우, 이 저작물에 적용된 이용허락조건 을 명확하게 나타내어야 합니다. l 저작권자로부터 별도의 허가를 받으면 이러한 조건들은 적용되지 않습니다. 저작권법에 따른 이용자의 권리는 위의 내용에 의하여 영향을 받지 않습니다. 이것은 이용허락규약(Legal Code)을 이해하기 쉽게 요약한 것입니다. Disclaimer 약학 석사학위 논문 안지오텐신 전환 효소 억제제 개시 이후 진해제의 사용 분석 Use of Antitussives After the Initiation of Angiotensin-Converting Enzyme Inhibitors 2017년 8월 서울대학교 대학원 약학과 사회약학전공 권 익 태 안지오텐신 전환 효소 억제제 개시 이후 진해제의 사용 분석 Use of Antitussives After the Initiation of Angiotensin-Converting Enzyme Inhibitors 지도교수 홍 송 희 이 논문을 권익태 석사학위논문으로 제출함 2017년 4월 서울대학교 대학원 약학과 사회약학전공 권 익 태 권익태의 석사학위논문을 인준함 2017년 6월 위 원 장 (인) 부 위 원 장 (인) 위 원 (인) Abstract Use of Antitussives After the Initiation of Angiotensin-Converting Enzyme Inhibitors Ik Tae Kwon Department of Social Pharmacy College of Pharmacy, Seoul National University Background Angiotensin-converting enzyme inhibitors (ACEI) can induce a dry cough, more frequently among Asians. If healthcare professionals fail to detect coughs induced by an ACEI, patients are at risk of getting antitussives inappropriately instead of discontinuing ACEI. The purpose of this study was to examine how the initiation of ACEI affects the likelihood of antitussive uses compared with the initiation of Angiotensin Receptor Blocker (ARB) and to determine the effect of the antitussive use on the duration and adherence of therapy in a Korean population. -

Elif Fatma Sen BW.Indd
Use and Safety of Respiratory Medicines in Children E. F. Şen EEliflif FFatmaatma SSenen BBW.inddW.indd 1 003-01-113-01-11 115:175:17 The work presented in this thesis was conducted at the Department of Medical Informatics of the Erasmus University Medical Center, Rotterdam. The research reported in thesis was funded by the European Community’s 6th Framework Programme. Project number LSHB-CT-2005-005216: TEDDY: Task force in Europe for Drug Development for the Young. The contributions of the participating primary care physicians in the IPCI, Pedianet and IMS-DA project are greatly acknowledged. Financial support for printing this thesis was kindly provided by the department of Medical Informatics – Integrated Primary Care Information (IPCI) project of the Erasmus University Medi- cal Center; and by the J.E. Jurriaanse Stichting in Rotterdam. Cover: Optima Grafi sche Communicatie Printed by: Optima Grafi sche Communicatie Elif Fatma Şen Use and Safety of Respiratory medicines in Children ISBN: 978-94-6169-003-6 © E.F. Şen, Rotterdam, the Netherlands, 2011. All rights reserved. No part of this thesis may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, without prior written permission of the holder of the copyright. EEliflif FFatmaatma SSenen BBW.inddW.indd 2 003-01-113-01-11 115:175:17 Use and Safety of Respiratory Medicines in Children Het gebruik en de bijwerkingen van respiratoire medicijnen in kinderen Proefschrift Ter verkrijging van de graad van doctor aan de Erasmus Universiteit Rotterdam op gezag van de rector magnifi cus Prof.dr. -

FF #200 Nonopioid Antitussives. 3Rd Edition
! FAST FACTS AND CONCEPTS #200 NON-OPIOID ANTI-TUSSIVES Sean Marks MD and Drew A Rosielle MD Background Cough is a common and at times distressing symptom. Fast Fact #199 discussed opioids for the symptomatic treatment of cough. This Fast Fact will address non-opioid anti-tussives. Controversies Commonly used prescription and over-the-counter anti-tussive formulations which contain some combination of antihistamines (e.g. diphenhydramine), a mucolytic (e.g. guaifenesin), and/ or dextromethorphan are often used for acute cough due to upper respiratory infections and acute bronchitis. Evidence for these agents in the acute setting is poor (either no better than placebo or sweet syrup) and cannot be recommended. Due to concerns about inadvertent overdose and lack of efficacy, these products are now being actively discouraged for use in the pediatric setting. Centrally-acting non-opioid anti-tussives • Gabapentin: the pathophysiology of refractory chronic cough is thought to resemble central sensitization as seen in neuropathic pain. A randomized, double-blind placebo controlled trial demonstrated that gabapentin can meaningfully improve cough-specific quality of life and reduce cough frequency and severity compared with placebo. Doses up to 1800 mg a day were studied. • Other neuromodulating agents: paroxetine, amitriptyline, and benzodiazepines have been anecdotally reported to have efficacy in chronic, refractory cough but lack published controlled evidence. Peripherally-acting anti-tussives • Sweet syrups are commonly used as cough suppressants, whether as bases for prescription elixirs (such as codeine with guaifenesin) or home remedies (honey, simple syrup). The mechanism of action is unknown; some authors hypothesize it acts as a protective barrier to sensory receptors in the throat that heighten the cough reflex. -

Proposal for Reclassification of Cough Medicines Containing Dextromethorphan, Opium Tincture, Squill Oxymel and Pholcodine to Restricted Medicines
Proposal for reclassification of cough medicines containing dextromethorphan, opium tincture, squill oxymel and pholcodine to restricted medicines Purpose Medsafe has recently been alerted to instances of abuse of cough medicines containing dextromethorphan. Concern was raised over the easy availability of opioid (and opioid-like) cough medicines which can be bought at a pharmacy or supermarket without healthcare professional supervision. Dextromethorphan is a substance that does not belong to the opioid family but has a chemical structure closely resembling the opioids. Dextromethorphan has a history of abuse in New Zealand and other countries. There are also other cough medicines available as pharmacy medicines which have been noted as at least having a potential for abuse, for example cough medicines containing pholcodine and Gees linctus which contains anhydrous morphine. Pholcodine and anhydrous morphine are both opioids. Medsafe therefore requests that Medicines Classification Committee (MCC) considers reclassification of dextromethorphan, opium tincture, squill oxymel and pholcodine containing products to Pharmacist-Only (restricted) medicines. Medsafe considers that a reclassification to restricted medicine balances a need for better supervision whilst maintaining access for those who benefit from using these medicines. Background Dextromethorphan and misuse (1) Dextromethorphan (DXM) is the D- isomer of the codeine synthetic analogue, levorphanol. DXM also structurally resembles ketamine and phenycycline which are dissociative agents, meaning that they can be used to incite a type of general anesthesia characterized by analgesia and amnesia with minimal effect on respiratory function. DXM is an opioid, but because of its stereochemistry, DXM and its metabolites do not bind to the mu and delta opioid receptors, thus avoiding classic opioid toxicity. -
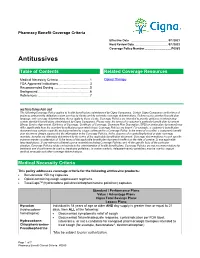
Antitussives
Pharmacy Benefit Coverage Criteria Effective Date ............................................ 9/1/2021 Next Review Date… ..................................... 9/1/2022 Coverage Policy Number ................................ P0083 Antitussives Table of Contents Related Coverage Resources Medical Necessity Criteria ................................... 1 Opioid Therapy FDA Approved Indications ................................... 3 Recommended Dosing ........................................ 5 Background .......................................................... 6 References .......................................................... 7 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies are based. For example, a customer’s benefit plan document may contain a specific exclusion related to a topic addressed in a Coverage -

Vol. 80 Monday, No. 138 July 20, 2015 Pages 42707–43006
Vol. 80 Monday, No. 138 July 20, 2015 Pages 42707–43006 OFFICE OF THE FEDERAL REGISTER VerDate Sep 11 2014 19:06 Jul 17, 2015 Jkt 235001 PO 00000 Frm 00001 Fmt 4710 Sfmt 4710 E:\FR\FM\20JYWS.LOC 20JYWS asabaliauskas on DSK5VPTVN1PROD with FRONTMATTER II Federal Register / Vol. 80, No. 138 / Monday, July 20, 2015 The FEDERAL REGISTER (ISSN 0097–6326) is published daily, SUBSCRIPTIONS AND COPIES Monday through Friday, except official holidays, by the Office PUBLIC of the Federal Register, National Archives and Records Administration, Washington, DC 20408, under the Federal Register Subscriptions: Act (44 U.S.C. Ch. 15) and the regulations of the Administrative Paper or fiche 202–512–1800 Committee of the Federal Register (1 CFR Ch. I). The Assistance with public subscriptions 202–512–1806 Superintendent of Documents, U.S. Government Publishing Office, Washington, DC 20402 is the exclusive distributor of the official General online information 202–512–1530; 1–888–293–6498 edition. Periodicals postage is paid at Washington, DC. Single copies/back copies: The FEDERAL REGISTER provides a uniform system for making Paper or fiche 202–512–1800 available to the public regulations and legal notices issued by Assistance with public single copies 1–866–512–1800 Federal agencies. These include Presidential proclamations and (Toll-Free) Executive Orders, Federal agency documents having general FEDERAL AGENCIES applicability and legal effect, documents required to be published Subscriptions: by act of Congress, and other Federal agency documents of public interest. Assistance with Federal agency subscriptions: Documents are on file for public inspection in the Office of the Email [email protected] Federal Register the day before they are published, unless the Phone 202–741–6000 issuing agency requests earlier filing. -

OPIOID COUGH MEDICATIONS Codeine with Phenylephrine And
OPIOID COUGH MEDICATIONS Codeine with phenylephrine and promethazine, Codeine with promethazine, FlowTuss* (hydrocodone bitartrate, guaifenesin), Hycofenix (hydrocodone bitartrate, pseudoephedrine, guaifenesin), Hydromet (hydrocodone bitartrate, homatropine), Obredon* (hydrocodone bitartrate, guaifenesin), TussiCaps (hydrocodone polistirex, chlorphineramine polistirex), Tussigon (hydrocodone bitartrate, homatropine), Tussionex Pennkinetic (hydrocodone bitartrate, chlorpheniramine), Tuxarin ER, Tuzistra XR (codeine, chlorpheniramine), Zutripro (hydrocodone bitartrate, pseudoephedrine, chlorpheniramine) * Prior authorization for the brand formulation applies only to formulary exceptions due to being a non-covered medication. RATIONALE FOR INCLUSION IN PA PROGRAM Background Opioids, such as codeine and hydrocodone, are often used in prescription cough medications to suppress cough. Many formulations of opioid cough medications include other drugs that treat cough and cold including chlorpheniramine (an antihistamine), pseudophedrine (a decongestant), and guaifenesin (an expectorant). The FDA has drastically increased safety measures regarding opioids in the past few years, including opioid use in children. It is now required that a contraindication label be on all codeine products stating that these products should not be used in children less than 12 years of age. Additionally, the FDA recently held an expert round table to address the use of cough and cold medications in individuals less than 18 years of age and ultimately decided that in most cases, the risks of using prescription opioid cough products outweigh the potential benefits. Specifically regarding cough medications, alternative medications should be utilized such as over the counter (OTC) cough suppressants like dextromethorphan and legend benzonatate products (1-2). Regulatory Status FDA approved indications: Opioid cough medications are indicated for the temporary relief of coughs nasal congestion, to loosen mucus and upper respiratory symptoms associated with allergy or the common cold. -

Benefit/Risk Assessment of Prescription Opioid Antitussive Products for Treatment of Cough in Pediatric Patients
Background Document Pediatric Advisory Committee Meeting September 11, 2017 Benefit/Risk Assessment of Prescription Opioid Antitussive Products for Treatment of Cough in Pediatric Patients Table of Contents 1. Introduction ..........................................................................................................................................2 2. Regulatory History of Prescription Opioid Antitussive Products .......................................................... 3 Codeine ..................................................................................................................................................... 3 Hydrocodone............................................................................................................................................. 5 Pediatric Study Requirements for Prescription Opioid Antitussives ........................................................ 8 3. Safety of Opioid Antitussive Products among Children and Adolescents ............................................ 9 Codeine and Risk of Respiratory Depression and Death Due to Ultra‐rapid Metabolism........................9 Hydrocodone and Risk of Respiratory Depression and Death................................................................ 12 Risks of misuse, abuse, addiction, overdose and death with opioid antitussives .................................. 13 4. Utilization of Products to Treat Cough in Pediatric Patients .............................................................. 14 5. Treatment Alternatives for Cough