A Bidirectional Analysis of Noncompliant Bedtime Behavior Desiree J
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

EPISODE 147: Loving Math with Read-Alouds
® EPISODE 147: Loving Math with Read-Alouds Kortney: 00:00 The scientist Margaret Wertheim says, "Mathematics, in a sense, is logic let loose in the field of the imagination." Sarah: 00:19 You're listening to the Read-Aloud Revival Podcast. This is the podcast that helps you make meaningful and lasting connections with your kids through books. Sarah: 00:37 Hello, hello, Sarah Mackenzie here. Happy to have you with us for episode 147 of the podcast. I am here today with the Read-Aloud Revival team, that includes our Community Director Kortney Garrison and our Podcast Manager, Kara Anderson. We're here today to talk about math. Sarah: 00:58 Now don't shut off the podcast. I know you want to. On the Read-Aloud Revival, we're going to talk about math? Yes, we are. We're going to do it in the best way we know how. We're going to talk about stories to share with our kids that are mathematically related, stories that deepen our kids' appreciation for math or maybe even deepen our own, and some of us could use some of that. Isn't that right? Sarah: 01:19 But also books that help them understand tricky mathematical concepts and teach math in a really delightful way. We have a whole brand new book list hot off the presses. If you are on the email list, you already got it. If you're not on the email list, you can go grab it. The book list is at readaloudrevival.com/147. -

The Return of the 1950S Nuclear Family in Films of the 1980S
University of South Florida Scholar Commons Graduate Theses and Dissertations Graduate School 2011 The Return of the 1950s Nuclear Family in Films of the 1980s Chris Steve Maltezos University of South Florida, [email protected] Follow this and additional works at: https://scholarcommons.usf.edu/etd Part of the American Studies Commons, and the Film and Media Studies Commons Scholar Commons Citation Maltezos, Chris Steve, "The Return of the 1950s Nuclear Family in Films of the 1980s" (2011). Graduate Theses and Dissertations. https://scholarcommons.usf.edu/etd/3230 This Thesis is brought to you for free and open access by the Graduate School at Scholar Commons. It has been accepted for inclusion in Graduate Theses and Dissertations by an authorized administrator of Scholar Commons. For more information, please contact [email protected]. The Return of the 1950s Nuclear Family in Films of the 1980s by Chris Maltezos A thesis submitted in partial fulfillment of the requirements for the degree of Master of Liberal Arts Department of Humanities College Arts and Sciences University of South Florida Major Professor: Daniel Belgrad, Ph.D. Elizabeth Bell, Ph.D. Margit Grieb, Ph.D. Date of Approval: March 4, 2011 Keywords: Intergenerational Relationships, Father Figure, insular sphere, mother, single-parent household Copyright © 2011, Chris Maltezos Dedication Much thanks to all my family and friends who supported me through the creative process. I appreciate your good wishes and continued love. I couldn’t have done this without any of you! Acknowledgements I’d like to first and foremost would like to thank my thesis advisor Dr. -

Bedtime Story by Anita Amin
Name: _________________________________ Rosie’s Bedtime Story By Anita Amin Rosie loved bedtime. Her dad always told her stories. Sometimes, he told fairy tales. Sometimes, he told animal stories. And sometimes, he told sports stories. Rosie couldn’t wait to hear Dad’s next story. But that night, Mom tucked Rosie into bed instead. “Dad is sick,” Mom told Rosie. “But I can tell you a story if you want me to.” So Mom told Rosie a story. But to Rosie, it wasn’t the same. She felt sad. She didn’t want Dad to be sick, and she missed story time with Dad. She thought maybe Dad missed story time, too. This gave her an idea. Rosie hopped out of bed. She went to Dad’s room. She knocked on his door. “Come in,” Dad said. When Rosie opened the door, Dad smiled weakly. “I’m sorry. I’m going to miss story time tonight.” Rosie sat on Dad’s bed. “No you won’t. I’m going to tell you a story.” So Rosie told Dad a story about a castle, a dragon, and a princess. Dad loved the story and he fell asleep with a smile on his face. “Get well quickly, Dad,” Rosie whispered. Super Teacher Worksheets - www.superteacherworksheets.com Name: ___________________________________ Rosie’s Bedtime Story By Anita Amin 1. Complete the graphic organizer. 3 Types of Stories that Dad Tells Rosie 2. Why didn’t Rosie’s dad tuck her into bed? ________________________________________________________________ 3. What type of story did Rosie tell her dad? a. a true story b. -

Bedtime) Story Ever Told
The Greatest (Bedtime) Story Ever Told By Brian T. Schultz The Greatest (Bedtime) Story Ever Told By Brian T. Schultz CAST of CHARACTERS (in order of appearance) Greta Jane Hank Esmerelda Katherine Jasmine Prunella Pocohontas Tortoise Megara Pirate Alice Evil Queen Sleeping Beauty 1st Little Pig Ariel ’Mother 2nd Little Pig Narco Handsome Prince Manic Driselda Smiley Papa Bear Fabio Goldilocks Crazy Old Dwarf Hare Drippy Fox Special Big Bad Wolf King Snow White Wicked Stepmother 3rd Little Pig Fairy Godmother Mama Bear Puss in Boots Jack Belle Cinderella Mulan Gingerbread Man Wendy Baby Bear TIME Now and Once Upon a Time PLACE Greta and ’bedroom The Forest The Castle The Bridge …and beyond “Greatest (Bedtime) Story Ever ”was originally produced by Aberdeen Community ’Young ’Theatre under the direction of Brian T. Schultz. It premiered on August 29, 2009 at the Capitol Theatre, Aberdeen, South Dakota. © 2009 Renaissance Artists Aberdeen, South Dakota, USA CAUTION: Professionals and amateurs are hereby warned that performance of this script (the "Play) is subject to payment of a royalty. It is fully protected under the copyright laws of the United States of America; all countries covered by the International Copyright Union (including the Dominion of Canada and the rest of the British Commonwealth); all countries covered by the Pan-American Copyright Convention, the Universal Copyright Convention and the Berne Convention; and of all countries with which the United States has reciprocal copyright relations. All rights, including without limitation professional/amateur stage rights, motion picture, recitation, lecturing, public reading, radio broadcasting, television, video or sound recording, all other forms of mechanical, electronic and digital reproduction, transmission and distribution, such as CD, DVD, Internet, private and file-sharing networks, information storage and retrieval systems, photocopying or any other form now known or yet to be invented and the rights of translation into foreign languages are strictly reserved. -

It's Bedtime! Your Child’S Doctor
Resources OTHER RESOURCES It's Bedtime! Your child’s doctor. School Social Worker, counselor, psychologist or BOOKS FOR KIDS nurse. Tell Me Something Happy Before I Go to Counselors in the community. See both the yellow Sleep* by Debi Gliori and blue pages of the Lincoln Telephone book. Sea Otter Cove: A Relaxation Story by Lori Lite The Goodnight Caterpillar: A Children’s Relaxation Story by Lori Lite Be the Boss of Your Sleep by Timothy Culbert M.D. No Such Thing* by Jackie French Koller Sleep, Big Bear, Sleep* by Maureen Wright Dr. Seuss’s Sleep Book* by Dr. Seuss BOOKS FOR PARENTS Good Night, Sweet Dreams, I Love You by Patrick Friman Simplicity Parenting by Kim John Payne and Lisa Ross Solve your Child’s Sleep Problems* by Richard Ferber Healthy Sleep Habits, Happy Child* by Marc Weissbluth Starbright: Meditations for Children* by Maureen Garth The Sleep Lady’s Good Night, Sleep Tight: Gentle Proven Solutions to Help your Child Need help? Don’t know where to start? Bedtime. Sleep Well and Wake up Happy* by Kim West & Joanne Kenen Dial 2-1-1 or go to www.ne211.org. It's a word dreaded by many children. Inside are ideas to help bedtime be a pleasant time for families. Provided by LPS School Social Workers * Books available at Lincoln City Libraries BECAUSE FAMILIES MATTER Rev. 7/2015 routine to allow her time to finish what she is Share in your child’s bedtime routine. Your Bedtime doing. Sometimes setting a timer can be helpful. nurturing can help your child feel secure and be “Bedtime” is a word dreaded by many children. -

Why Fathers Matter to Their Children's Literacy
Why Fathers Matter to Their Children’s Literacy Christina Clark National Literacy Trust June 2009 Table of contents Introduction............................................................................................................... 3 Changing outlook on fatherhood ............................................................................. 3 Obstacles to family time.......................................................................................... 4 Father’s involvement in literacy............................................................................... 5 How are fathers involved with their children’s literacy activities? ...................... 7 Family life in Britain................................................................................................. 7 Father’s involvement in literacy............................................................................... 8 Defining literacy ...................................................................................................... 9 Mother vs. father involvement ............................................................................... 10 Involvement at different stages ............................................................................. 10 The benefits of father involvement ....................................................................... 11 The effects of father involvement on educational attainment and on literacy in particular .............................................................................................................. -

Best Books for 4'S And
Ants in My Pants by Wendy Mould Vocabulary Jacob comes up with lots of silly excuses not to go shopping with his Narrative Skills Help kids learn specific words for things and ideas. mom. Help children understand and retell stories Bubble Gum, Bubble Gum by Lisa Wheeler by using repeating, predicting, Actual Size by Steve Jenkins Yuck! Who gets stuck? See how big or small these wild animals really are. Castles, Caves and Honeycombs by Linda Ashman sequencing and summarizing questions Alice the Fairy by David Shannon Try to guess the animals that live in each house. to talk about books. She’s a creative girl who knows all kinds of magical words. Clara Caterpillar by Pamela Duncan Can You See What I See? Cool Collections by WalterWick In this story about hidden talents, learn how caterpillars change Can you spy all the robots, dinosaurs and letters? into butterflies and count the ‘C’ words. Sequencing Do Frogs Have Fur? With these books, ask questions like: ‘What happened first? And then? What happened in the end?’ Arrowhawk by Lola Schaefer A hawk is injured and struggles to survive in this true story. A Book About Coats and Coverings by Michael Dahl I Ain’t Gonna Paint No More! by Karen Beaumont Calabash Cat and His Amazing Journey by James Rumford Laugh and learn with these fun facts. Picture Window Books To the tune of "It Ain't Gonna Rain No More," one creative kid floods This is an African tale of wisdom and perspective. If I Were a Lion by Sarah Weeks his world with color, painting first the walls, then the ceiling, and then Cat Who Came for Tacos by Diana Star Helmer Learn lots of adjectives and attitude in this smart and himself. -
Adventuring with Books: a Booklist for Pre-K-Grade 6. the NCTE Booklist
DOCUMENT RESUME ED 311 453 CS 212 097 AUTHOR Jett-Simpson, Mary, Ed. TITLE Adventuring with Books: A Booklist for Pre-K-Grade 6. Ninth Edition. The NCTE Booklist Series. INSTITUTION National Council of Teachers of English, Urbana, Ill. REPORT NO ISBN-0-8141-0078-3 PUB DATE 89 NOTE 570p.; Prepared by the Committee on the Elementary School Booklist of the National Council of Teachers of English. For earlier edition, see ED 264 588. AVAILABLE FROMNational Council of Teachers of English, 1111 Kenyon Rd., Urbana, IL 61801 (Stock No. 00783-3020; $12.95 member, $16.50 nonmember). PUB TYPE Books (010) -- Reference Materials - Bibliographies (131) EDRS PRICE MF02/PC23 Plus Postage. DESCRIPTORS Annotated Bibliographies; Art; Athletics; Biographies; *Books; *Childress Literature; Elementary Education; Fantasy; Fiction; Nonfiction; Poetry; Preschool Education; *Reading Materials; Recreational Reading; Sciences; Social Studies IDENTIFIERS Historical Fiction; *Trade Books ABSTRACT Intended to provide teachers with a list of recently published books recommended for children, this annotated booklist cites titles of children's trade books selected for their literary and artistic quality. The annotations in the booklist include a critical statement about each book as well as a brief description of the content, and--where appropriate--information about quality and composition of illustrations. Some 1,800 titles are included in this publication; they were selected from approximately 8,000 children's books published in the United States between 1985 and 1989 and are divided into the following categories: (1) books for babies and toddlers, (2) basic concept books, (3) wordless picture books, (4) language and reading, (5) poetry. (6) classics, (7) traditional literature, (8) fantasy,(9) science fiction, (10) contemporary realistic fiction, (11) historical fiction, (12) biography, (13) social studies, (14) science and mathematics, (15) fine arts, (16) crafts and hobbies, (17) sports and games, and (18) holidays. -

Complete Wellbeing
Decide sleep claims the lives of thousands of American babies each year. SIDS is marked by parents finding their infant The bedtime story child dead in its sleep, often without explanation. By n India, it has been a practice, since centuries, moving children into their parents’ beds, scientists at to put the baby to sleep with the mother. By and the University of Notre Dame found that SIDS risks were l far, this is quite safe. However, there is a theoreti- significantly reduced. Around the same time, interests cal danger of the baby being smothered or getting in ‘Attachment parenting’ forwarded by paediatrician choked. This is especially true if either of the par- William Sears—have reintroduced parents to a style of ents is on medications, or are habituated to taking sleep that people around the world practise without alcohol or drugs, which cause sleepiness. In such hesitation. Americans are still unsure about bedsharing, cases, sleeping with the baby should be avoided. and many paediatricians and parenting experts also Also, putting the baby to sleep in a crib is crticise it. But the evidence from James McKenna’s usually a safe practice, preferred more in foreign countries than in India. Abroad, children are made laboratory at Notre Dame is fairly clear: careful parents, to sleep in a crib separately, right from the day who take the necessary precautions, might receive up to they are born. However in India and in many South two extra hours of sleep each night. Eastern countries, it is not common to separate the For those parents who are still wary about sharing mother and child so soon, and most babies sleep their beds, placing the child’s bed in his or her parents’ with the mother, at least for the first few months. -

Bedtime Stories
BEDTIME STORIES Bedtime Stories Bedtime stories that teach godly character and that show how the truths of the Bible play out in daily life are an incredible tool for instilling spiritual values in your child. The following section contains 6 bedtime stories, one for each week of this series. WELCOME Bible Bedtime Stories Bible Bedtime Stories are simple and easy quick-read stories Hebrews 11 that you can share with your child straight out of God's Word. Is Faith’s Hall of Fame. It's another great part of a bedtime ritual. Children need consistency but also variety. The consistency is that you read a But read it slowly, bedtime story each night or on certain nights...the variety is And look at each name. that you use different kinds of stories on different nights and what better stories are there than the stories that God has given us in His Word. What a great way for children to know These were not superheroes, and understand the heroes of the Bible better. Who could soar through the sky. Bedtime Bible Readings They were ordinary people, Week 1 –Hebrews 12:1 – 2 Just like you and I. Week 2 –Hebrews 11:1 – 7 Week 3 –Hebrews 11:8 – 16 Week 4 –Hebrews 11:17 – 22 The difference with them, Week 5 –Hebrews 11:23 – 31 Was their trust in the Lord, Week 6 –Hebrews 11:32 – 40 How they held to the truths, That we find in His Word. Use Your Own Experiences as Bedtime Stories Children love to hear about your "adventures" and experiences when you were a child. -
Step Parenting
ONLINE SUPPORT FOR YOU AND FAMILIES YOU KNOW Supportwww.careforthefamily.org.uk/supportnetNet Step-parenting Stepfamilies are on the increase and, with much love and hard work, a blended family home can be a happy and positive place to be. You get talking to a mum, dad and their four kids while with their other parent. This couple may have only been you’re queueing for cinema tickets and - without really married for two years - he was a widower and she had been thinking about it - you assume Mum is mother of all the divorced. They may be struggling with the effects of her children, Dad is father of all the children, and the children first husband on this family, resentment from grandparents are all brothers and sisters. If you gave it any thought, you and lack of space and time. You just don’t know. might guess they’d been married about 16 years - the oldest However second families are made up, it’s hard work to child looks about 13 or 14. get them to blend. It takes time, effort, patience and lots of But maybe only two of the children live with them love. But it can - and very often does - work. all the time. The other two stay at weekends - they live Second marriage stability When I met Christine she was hugely pregnant with her third I sensed resentment towards me in the early days. I owe so child. Her husband had recently left her and their two sons, much to Christine for the way she guided their thoughts and Andrew (9) and Mark (6), for another woman. -
Bedtime Story Reading Guide 3
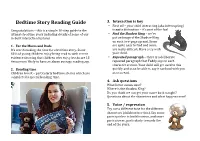
Bedtime Story Reading Guide 3. Interaction is key • First off – your child interacting (aka interrupting) Congratulations – this is a simple 10‐step guide to the is not a distraction – it’s part of the fun! ultimate bedtime story including details of some of our • Find the Shadow King – we’ve in‐built interaction features put an image of the Shadow King on each two‐page spread. Some 1. For the Mums and Dads are quite easy to find and some It’s worth making the time for a bedtime story. Some are really difficult. Have a try with 83% of young children enjoy being read to with recent your child. evidence showing that children who enjoy books are 13 • Repeated paragraph – there is a deliberate times more likely to have an above average reading age. repeated paragraph that Teddy says in each character section. Your child will get used to this 2. Bonding time quickly and soon be able to say it out loud with you Children love it – particularly bedtime stories which are as you read. considered a special bonding time. 4. Ask questions What letter comes next? Where is the Shadow King? Do you think we can get your name back tonight? Questions about the characters and what happens next? 5. Voice / expression Try use a different tone for the different characters (children love this). Say some parts quicker to build tension, and some parts slower, particularly towards the end of the story. 10. Get comfortable 6. Illustrations We love stories in bed but comfy chairs work For young children it’s hard to beat a quality picture really well too.