Jrheum.201376.Full.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pathogenic Mutations Identified by a Multimodality Approach in 117 Japanese Fanconi Anemia Patients
ERRATA CORRIGE Bone Marrow Failure Pathogenic mutations identified by a multimodality approach in 117 Japanese Fanconi anemia patients Minako Mori, 1,2 Asuka Hira, 1 Kenichi Yoshida, 3 Hideki Muramatsu, 4 Yusuke Okuno, 4 Yuichi Shiraishi, 5 Michiko Anmae, 6 Jun Yasuda, 7Shu Tadaka, 7 Kengo Kinoshita, 7,8,9 Tomoo Osumi, 10 Yasushi Noguchi, 11 Souichi Adachi, 12 Ryoji Kobayashi, 13 Hiroshi Kawabata, 14 Kohsuke Imai, 15 Tomohiro Morio, 16 Kazuo Tamura, 6 Akifumi Takaori-Kondo, 2 Masayuki Yamamoto, 7,17 Satoru Miyano, 5 Seiji Kojima, 4 Etsuro Ito, 18 Seishi Ogawa, 3,19 Keitaro Matsuo, 20 Hiromasa Yabe, 21 Miharu Yabe 21 and Minoru Takata 1 1Laboratory of DNA Damage Signaling, Department of Late Effects Studies, Radiation Biology Center, Graduate School of Biostudies, Kyoto University, Kyoto, Japan; 2Department of Hematology and Oncology, Graduate School of Medicine, Kyoto University, Kyoto, Japan; 3Department of Pathology and Tumor Biology, Graduate School of Medicine, Kyoto University, Kyoto, Japan; 4Department of Pediatrics, Nagoya University Graduate School of Medicine, Nagoya, Japan; 5Laboratory of DNA Information Analysis, Human Genome Center, The Institute of Medical Science, University of Tokyo, Tokyo Japan; 6Medical Genetics Laboratory, Graduate School of Science and Engineering, Kindai University, Osaka, Japan; 7Tohoku Medical Megabank Organization, Tohoku University, Sendai, Japan; 8Department of Applied Information Sciences, Graduate School of Information Sciences, Tohoku University, Sendai, Japan; 9Institute of Development, Aging, -

Japan Ryugaku Awards Special
6 | The Japan Times | Monday, November 30, 2020 Japan Ryugaku Awards special (Sponsored content) Schools lauded for COVID-19 response, support The number of international students At that time, many students at Japanese ties and Japanese language schools, as well ments, Takushoku University received Japan’s education. pass level N2 of the JLPT before enter- enrolled in Japanese universities and voca- language schools returned to their home as affiliated business representatives. the east grand prize, while the west grand The pandemic has severely disrupted ing a program conducted in Japanese. But tional schools is on the rise. In May 2019, countries. Since then, Japanese language This year, 176 Japanese language schools prize went to the University of Market- Japanese-language schools, which play some educators observe that students this number stood at 312,214, up from schools have selected award recipients submitted 469 votes to select 50 institu- ing and Distribution Sciences. In the cat- an important role in preparing students who have passed this exam may still have 164,000 in 2011, and the number of students based on numerous criteria. Providing tions across five categories: vocational egory for private science departments, to enroll in vocational schools and uni- trouble understanding their instructors who chose to work in Japan after graduat- easy-to-understand materials, establishing schools, private liberal arts departments, Tokyo University of Science received the versities. According to surveys conducted and classmates. Japanese language schools ing has more than doubled since 2013. separate tracks for international students, private science departments, public east grand prize and Kindai University, by Japanese language schools, approxi- generally teach their curriculum over two Supporting this influx of international simplifying application procedures and universities and graduate schools. -
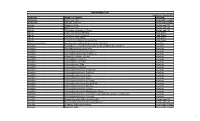
Unai Members List August 2021
UNAI MEMBER LIST Updated 27 August 2021 COUNTRY NAME OF SCHOOL REGION Afghanistan Kateb University Asia and the Pacific Afghanistan Spinghar University Asia and the Pacific Albania Academy of Arts Europe and CIS Albania Epoka University Europe and CIS Albania Polytechnic University of Tirana Europe and CIS Algeria Centre Universitaire d'El Tarf Arab States Algeria Université 8 Mai 1945 Guelma Arab States Algeria Université Ferhat Abbas Arab States Algeria University of Mohamed Boudiaf M’Sila Arab States Antigua and Barbuda American University of Antigua College of Medicine Americas Argentina Facultad de Ciencias Económicas de la Universidad de Buenos Aires Americas Argentina Facultad Regional Buenos Aires Americas Argentina Universidad Abierta Interamericana Americas Argentina Universidad Argentina de la Empresa Americas Argentina Universidad Católica de Salta Americas Argentina Universidad de Congreso Americas Argentina Universidad de La Punta Americas Argentina Universidad del CEMA Americas Argentina Universidad del Salvador Americas Argentina Universidad Nacional de Avellaneda Americas Argentina Universidad Nacional de Cordoba Americas Argentina Universidad Nacional de Cuyo Americas Argentina Universidad Nacional de Jujuy Americas Argentina Universidad Nacional de la Pampa Americas Argentina Universidad Nacional de Mar del Plata Americas Argentina Universidad Nacional de Quilmes Americas Argentina Universidad Nacional de Rosario Americas Argentina Universidad Nacional de Santiago del Estero Americas Argentina Universidad Nacional de -

An Analysis of Elliptical Phenomena Based on Non-Constituent Deletion
An Analysis of Elliptical Phenomena Based on Non-Constituent Deletion by Daisuke Hirai B. A., Kyoto University of Foreign Studies, 1997 M. S., University of Wisconsin-River Falls, 1999 A Dissertation Submitted for the Degree of Doctor of Philosophy to Kansai Gaidai University 2018 Acknowledgements It is hardly a trivial task to properly acknowledge everyone who has helped me during my research and reach this point. Without their help, this dissertation would never have come into existence or taken shape as it is. First and foremost, I would like to thank Yukio Oba, my thesis supervisor. He has given me a lot of advice and constant encouragement since I was a graduate student at Nagoya University. I am very fortunate that he invited me to study at Kansai Gaidai University and work on this topic to complete this dissertation. It has been a great pleasure to study under his guidance. I cannot thank him enough for reading my rough draft and giving me a lot of comments on it. I would also like to thank the other members of the committee, Nobuo Okada, Kansai Gaidai University, and Sadayuki Okada, Osaka University for reading my paper and giving me a lot of valuable comments. Their comments helped me look into more ellipsis-related examples. This will lead me to work on another topic as a next step. I would also like to acknowledge the past and present members of the graduate school of Kansai Gaidai University, Jun Omune and Shota Tanaka for reading my first version of this dissertation and their comments on it. -
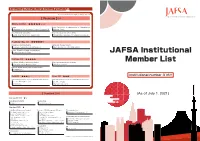
JAFSA Institutional Member List
Supporting Member(Social Business Partners) 43 ※ Classified by the company's major service [ Premium ](14) Diamond( 4) ★★★★★☆☆ Finance Medical Certificate for Visa Immunization for Studying Abroad Western Union Business Solutions Japan K.K. Hibiya Clinic Global Student Accommodation University management and consulting GSA Star Asia K.K. (Uninest) Waseda University Academic Solutions Corporation Platinum‐Exe( 3) ★★★★★☆ Marketing to American students International Students Support Takuyo Corporation (Lighthouse) Mori Kosan Co., Ltd. (WA.SA.Bi.) Vaccine, Document and Exam for study abroad Tokyo Business Clinic JAFSA Institutional Platinum( 3) ★★★★★ Vaccination & Medical Certificate for Student University management and consulting Member List Shinagawa East Medical Clinic KEI Advanced, Inc. PROGOS - English Speaking Test for Global Leaders PROGOS Inc. Gold( 2) ★★★☆ Silver( 2) ★★★ Institutional number 316!! Global Human Resources services・Study Abroad Information Global Human Resources services・Study Abroad Information Access Nextage Co.,Ltd Doorkel Co.,Ltd. DISCO Inc. Mynavi Corporation [ Standard ](29) (As of July 1, 2021) Standard20( 2) ★☆ Study Abroad Information Housing・Hotel Keibunsha MiniMini Corporation . Standard( 27) ★ Study Abroad Program and Support Insurance / Risk Management /Finance Telecommunication Arc Three International Co. Ltd. Daikou Insurance Agency Kanematsu Communications LTD. Australia Ryugaku Centre E-CALLS Inc. Berkeley House Language Center JAPAN IR&C Corporation Global Human Resources Development Fuyo Educations Co., Ltd. JI Accident & Fire Insurance Co., Ltd. JTB Corp. TIP JAPAN Fourth Valley Concierge Corporation KEIO TRAVEL AGENCY Co.,Ltd. Tokio Marine & Nichido Fire Insurance Co., Ltd. Originator Co.,Ltd. OKC Co., Ltd. Tokio Marine & Nichido Medical Service Co.,Ltd. WORKS Japan, Inc. Ryugaku Journal Inc. Sanki Travel Service Co.,Ltd. Housing・Hotel UK London Study Abroad Support Office / TSA Ltd. -

UNIVERSITY CONTACT POINTS GUIDE BOOK 2021 for INTERNATIONAL STUDENTS Undergraduate
English KANSAI UNIVERSITY CONTACT POINTS GUIDE BOOK 2021 FOR INTERNATIONAL STUDENTS Undergraduate www.kansai-u.ac.jp/English/contact/faq.htm Graduate Schools www.kansai-u.ac.jp/English/contact/faq.htm Japanese Language and Culture Program Preparatory Course (Bekka) www.kansai-u.ac.jp/English/contact/faq.htm Division of International Affairs www.kansai-u.ac.jp/Kokusai/english/ department/contact.php Kansai University Video www.kansai-u.ac.jp/Kokusai/english/ Undergraduate Faculties Graduate Schools at a Glance department/pr.php www.kansai-u.ac.jp/English/academics/fac_undergraduate.html www.kansai-u.ac.jp/English/academics/gr_school.html 13 faculties facing modern topics with 13 graduate schools and 2 professional graduate schools Kansai University, founded in 1886, is a private 'THINK × ACT' philosophy for the betterment of society with state-of-the-art educational facilities and research system university with 134 years of history. All of its campuses are located in Osaka. 30,750 1,100 470,000 Faculty of Law Graduate School of Law As the largest city in western Japan, Osaka has Students International Graduates ■Department of Law and Politics [Master's Degree Program][Ph.D. Degree Program] Law and Politics Major long been famous as a cultural center. Students Located about an hour from Kyoto, Nara, and Kobe, Faculty of Letters Graduate School of Letters [Master's Degree Program] Kansai University offers international students the ■Department of General Humanities General Humanities Major / / Department of English Linguistics and Literature/American -

Study Abroad Course Entrance Procedure <April 2019-January 2020 Term>
Study Abroad Course Entrance Procedure <April 2019-January 2020 Term> アーク京都日本語学校 ARC Academy Kyoto School 1.Characteristics of ARC Academy Page 2 2.Course Outline Page 3 3.Admission Procedure Page 4 4.Study Abroad Course Application Documents Page 5 5.Course Fees Page 6 6.Life in Japan Page 7 7.School Map / Overseas Office Page 8 - 1 - 1.Characteristics of ARC Academy 1. Communication Skills Trained by Skilled Teachers Since opening our school in 1986, ARC Academy has provided Japanese language education focusing on communication skills acquisition. We offer a variety of classroom programs designed to teach students smooth practical Japanese. Our school also features a “Japanese Language Teachers’ Training Section.” From the school opening to present, we have produced many skilled Japaese language teachers operating within and outside Japan. ARC Academy Kyoto provides the Study Abroad Course, aimed at students who wish to learn Japanese systematically for a long term to pursue higher education or to find a job in Japan, and the Intensive Course, where students can learn useful Japanese in a communicative way in a short term. 2.Multinational Students ARC Academy Kyoto receives students from over 25 countries. Through interaction with students from different countries, students are able to learn what it is like to live in a multicultural society. 3.Academic and Career Support (1)Guidance for Entering Higher Education Institutes We will give detailed guidance to students interested in entering graduate schools, universities, vocational schools, etc. We offer “Seminars”on entering higher eduation”periodically, and introduce to you the latest information on how to access higher education. -
KINKI UNIVERSITY Founding Principles
Research and Learning for the Real World 3-4-1 Kowakae, Higashiosaka City, Osaka 577-8502, Japan Tel: +81-6-6721-2332 http://www.kindai.ac.jp/ KINKI UNIVERSITY Founding Principles ‘Learning for the real world’ and ‘nurturing intellectual and emotional intelligence’ Educational Goal To develop caring, trustworthy, and respectable people Contents 03 Our Profile 05 Kindai Kinetics 07 Facts & Figures 09 Research 11 Aquaculture 13 Faculty Spotlight 15 Academics 17 Exchange 19 Collaboration 21 Medicine 23 Sports 25 President’s Message Our Profile Higashiosaka Campus (Main Campus) Nara Campus Osaka-Sayama Campus At a Glance Our Name The name “Kinki” refers to the region in western Japan where our university is located. The Kinki University was founded in 1949. Now one of Japan’s largest universities, it Kinki region covers seven prefectures and includes the cities of Kyoto, Kobe, Osaka, Wakayama, and Nara. The university is informally known as “Kindai,” a name formed by has six campuses in western Japan and boasts research facilities across the Higashiosaka Campus combining kin from Kinki with dai from daigaku, the Japanese word for university. In April nation—from Hokkaido in the north to Kagoshima in the south. Currently, Kinki 2016, “Kindai University” will become the official English name for Kinki University, and a foreign language faculty will be launched—moves that will further the university’s aims of University comprises 13 faculties with 48 departments, 11 graduate schools, a Nara Campus broadening its international profile. law school, 20 research facilities, two junior colleges, 18 associated primary and Hiroshima Campus secondary schools, and three teaching hospitals. -

METHODOLOGY for the TIMES HIGHER EDUCATION JAPAN UNIVERSITY RANKINGS 2018 March 2018
THE Japan University Rankings 2018 methodology | Times Higher Education (THE) METHODOLOGY FOR THE TIMES HIGHER EDUCATION JAPAN UNIVERSITY RANKINGS 2018 March 2018 1 THE Japan University Rankings 2018 methodology | Times Higher Education (THE) About THE: Times Higher Education (THE, part of TES Global Limited) is the data provider underpinning university excellence in every continent across the world. As the company behind the world’s most influential university ranking, and with almost five decades of experience as a source of analysis and insight on higher education, we have unparalleled expertise on the trends underpinning university performance globally. Our data and benchmarking tools are used by many of the world’s most prestigious universities to help them achieve their strategic goals. THE Japan University Rankings: The annual Times Higher Education (THE) Japan University Rankings, started in 2017, aims to provide the definitive list of the best universities in Japan, evaluated across four key pillars of Resources, Engagement, Outcomes and Environment. Times Higher Education’s data is trusted by governments and universities and is a vital resource for students, helping them choose where to study. Benesse Corporation is a publisher of educational materials in Japan, and has strong relationships throughout the Japanese education community. These rankings have been prepared by THE, together with Benesse Corporation and are published by Benesse Corporation in Japan and by THE across the world. Independent assurance by PricewaterhouseCoopers LLP: To help demonstrate the integrity of the Rankings, our application of the specific procedures (i) - (viii) has been subject to independent assurance by PricewaterhouseCoopers LLP UK (“PwC”). Their independent assurance opinion on our application of specific procedures (i) – (viii) is set out on the final page of this document. -

11. International Law and Organizations
108 WASEDA BULLETIN OF COMPARATIVE LAW Vol. 35 Agriculture and Forestry) (5) Discussion 11. International Law and Organizations The Japanese Society of International Law held its 2015 Annual Meeting at Nagoya Congress Center during September 18-20, 2015. Day One: Plenary Session: The “Changes” of the System of Sovereign States Chair: Kazuhiro Nakatani, Professor, University of Tokyo 1. Japanese Practice in State Recognition Masahiro Kato, Official, Ministry of Foreign Affairs of Japan 2. Secession in International Law: How Should We Understand the Challenge to the Territorial Sovereignty? Zhi-an Wang, Professor, Komazawa University 3. Reconsideration of the Legal Criteria for Statehood in the International System of State Recognition: Focusing on the Cases in the Non- European States Eiichi Usuki, Professor, Daito Bunka University 4. The Relationship between State( Government) Recognition under International Law and International Private Law Hiroshi Taki, Professor, Chuo University Day Two: Plenary Session: Modern Challenges in Security Chair: Masahiko Asada, Professor, Kyoto University 1. Collective Self-Defense in Modern International Society: Requirement of Request for Assistance and the Legal Character of the Right to Collective Self-Defense Tadashi Mori, Professor, University of Tokyo 2. Rethinking of the Conditions of Occurrence of the International Armed Conflict: The Functions of the Status of Combatant Masahiro Kurosaki, Associate Professor, National Defense Academy DEVELOPMENTS IN 2015 ̶ ACADEMIC SOCIETIES 109 of Japan 3. The Changes in the Security Environment and the Use of Force: From the Viewpoint of International Politics Hiroshi Nakanishi, Professor, Kyoto University Group Session 1: Fragmentation and Unification of International Law Chair: Satoru Taira, Professor, Osaka City University 1. -

CEEP Working Paper Series Working Paper Number 18 August 2021
CEEP Working Paper Series Working Paper Number 18 August 2021 North-South Displacement Effects of Environmental Regulation: The Case of Battery Recycling Shinsuke Tanaka, Kensuke Teshima, and Eric Verhoogen https://ceep.columbia.edu/sites/default/files/content/papers/n18.pdf North-South Displacement Effects of Environmental Regulation: The Case of Battery Recycling* Shinsuke Tanaka Kensuke Teshima Eric Verhoogen§ Aug. 2021 Abstract This study examines the effect of a tightening of the U.S. air-quality standard for lead in 2009 on the relocation of battery recycling to Mexico and on infant health in Mexico. In the U.S., airborne lead dropped sharply near affected plants, most of which were battery-recycling plants. Exports of used batteries to Mexico rose markedly. In Mexico, production increased at battery-recycling plants, relative to comparable industries, and birth outcomes deteriorated within two miles of those plants, relative to areas slightly farther away. The case provides a salient example of a pollution-haven effect between a developed and a developing country. Keywords: pollution-haven hypothesis, environmental regulation, infant health JEL Codes: F18, Q56, O15 *We thank the editor, Rohini Pande, four anonymous referees, Manuela Angelucci, Yutaka Arimoto, Shin-Yi Chou, Lucas Davis, Melissa Dell, Dave Donaldson, Manuel Estay, Alan Finkelstein, Laura Gee, Marco Gonzalez- Navarro, Gene Grossman, Rema Hanna, Danae Hern´andez-Cort´es, Akira Hibiki, Koichiro Ito, Michael Klein, Michikazu Kojima, Arik Levinson, Enrique Mart´ınez-Garc´ıa, -

International Exchange 2019
KINDAI 近畿大学国際交流 UNIVERSITY INTERNATIONAL EXCHANGE 2019 E 3 [e-cube] KUDOS Kindai bluefin tuna The Village-English, Enjoyment, Education ACADEMIC THEATER (Center for Data Processing Education) Kindai University Introduction of Kindai University Kindai University, also referred to as Kindai, has six campuses around western Japan and is one of the nation’s largest universities. Its main campus is located in Osaka and is officially called the Higashiosaka Campus. The university has a total of 14 faculties, nine of which are situated at the Higashiosaka campus. Among the 14 faculties, the Faculty of Business Administration, the Faculty of Applied Sociology and the Faculty of Science and Engineering attract many international students. The Higashiosaka campus is ideally locat- ed in that one can reach the business center of Osaka via train in less than fifteen minutes. Moreover, it takes only one hour to Kyoto, Nara or Kobe by train. Therefore, while you study at Kindai during the week, you can easily visit and enjoy many of Japan’s oldest and most historical cities on the weekend. The Higashiosaka campus is rather large (470,000m2 ) for an urban Japanese university. It is a modern university with up-to-date fa- cilities. The Central Library has more than 1.5 million books, including many rare and valuable manuscripts. A new library with a large proportion of manga opened in 2017, which is home to around 70,000 books including about 22,000 comics, with a 2400-seat self- study space open for 24 hours. One of the great academic achievements of Kindai University is the full-cycle aquaculture method used to farm the endangered Blue- fin tuna.