Inhibition of IRF4 in Dendritic Cells by PRR-Independent
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Detection of Interacting Transcription Factors in Human Tissues Using
Myšičková and Vingron BMC Genomics 2012, 13(Suppl 1):S2 http://www.biomedcentral.com/1471-2164/13/S1/S2 PROCEEDINGS Open Access Detection of interacting transcription factors in human tissues using predicted DNA binding affinity Alena Myšičková*, Martin Vingron From The Tenth Asia Pacific Bioinformatics Conference (APBC 2012) Melbourne, Australia. 17-19 January 2012 Abstract Background: Tissue-specific gene expression is generally regulated by combinatorial interactions among transcription factors (TFs) which bind to the DNA. Despite this known fact, previous discoveries of the mechanism that controls gene expression usually consider only a single TF. Results: We provide a prediction of interacting TFs in 22 human tissues based on their DNA-binding affinity in promoter regions. We analyze all possible pairs of 130 vertebrate TFs from the JASPAR database. First, all human promoter regions are scanned for single TF-DNA binding affinities with TRAP and for each TF a ranked list of all promoters ordered by the binding affinity is created. We then study the similarity of the ranked lists and detect candidates for TF-TF interaction by applying a partial independence test for multiway contingency tables. Our candidates are validated by both known protein-protein interactions (PPIs) and known gene regulation mechanisms in the selected tissue. We find that the known PPIs are significantly enriched in the groups of our predicted TF-TF interactions (2 and 7 times more common than expected by chance). In addition, the predicted interacting TFs for studied tissues (liver, muscle, hematopoietic stem cell) are supported in literature to be active regulators or to be expressed in the corresponding tissue. -

Cultured Human Langerhans Cells Resemble Lymphoid Dendritic Cells in Phenotype and Function
Cultured Human Langerhans Cells Resemble Lymphoid Dendritic Cells in Phenotype and Function Nikolaus Romani, Ph.D., Angela Lenz, Herta Glassel, Ph.D., Hella Stossel, Ursula Stanzl, Otto Majdic, M.D., Peter Fritsch, M.D., and Gerold Schuler, M.D. D~p2rnnent$ of DerlTl2tology and Internal Medicine (HG). University of lnnsbrud:.. Innsbruck. :and Inscirute of Immunology (OM). University of Vienna. Vienn2, Austria Freshly isolated murine epidermal Langerhans cells (LC) are rured human LC resembled human lymphoid dendritic cells weak stimulators of resting T cells. Upon culture their phe in morphology, phenotype, and function. Specifically, LC notype changes, their stimulatory activity increases signifi became non-adherent upon culture and developed sheet-like cantly. and they come to resemble lymphoid dendritic cells. processes (so-called "veils"), decreased their surface ATP / Resident murine Le, therefore. might represent a reservoi.r ADP'ase acti vity, and lost nonspecific esterase activity. As in of immature dendritic cells. We have now used enzyme cyto the mouse, surface expression of MHC class I and 11 an tigens chemistry. a panel of some 80 monoclonal antibodies, and increased significantly. and Fell receptors were significantly immunofluorescence microscopy or two-color flow cytom reduced. Markers that are expressed by dendritic cells (like eery, as well as transmission electron microscopy. CO analyse CD40) appeared on LC following culrure. Cultured human the phenotype and morphology of human LC before and LC were potem T-cell stimulators. Our findings support the after 2 - 4 d of bulk epidermal cell culrure. In addition, LC view that resident human Le, like murine Le, represent were enriched from bulk epidermal cell culrures, and their immature precursors of lymphoid dendritic cells in skin stimulatory capacity was tested in the allogeneic mixed leu draining lymph nodes.] It,vest DermatoI93:600-609, 1989 kocyte reaction and the oxidative mitogenesis assay. -

Comprehensive Study of Nuclear Receptor DNA Binding Provides a Revised Framework for Understanding Receptor Specificity
ARTICLE https://doi.org/10.1038/s41467-019-10264-3 OPEN Comprehensive study of nuclear receptor DNA binding provides a revised framework for understanding receptor specificity Ashley Penvose 1,2,4, Jessica L. Keenan 2,3,4, David Bray2,3, Vijendra Ramlall 1,2 & Trevor Siggers 1,2,3 The type II nuclear receptors (NRs) function as heterodimeric transcription factors with the retinoid X receptor (RXR) to regulate diverse biological processes in response to endogenous 1234567890():,; ligands and therapeutic drugs. DNA-binding specificity has been proposed as a primary mechanism for NR gene regulatory specificity. Here we use protein-binding microarrays (PBMs) to comprehensively analyze the DNA binding of 12 NR:RXRα dimers. We find more promiscuous NR-DNA binding than has been reported, challenging the view that NR binding specificity is defined by half-site spacing. We show that NRs bind DNA using two distinct modes, explaining widespread NR binding to half-sites in vivo. Finally, we show that the current models of NR specificity better reflect binding-site activity rather than binding-site affinity. Our rich dataset and revised NR binding models provide a framework for under- standing NR regulatory specificity and will facilitate more accurate analyses of genomic datasets. 1 Department of Biology, Boston University, Boston, MA 02215, USA. 2 Biological Design Center, Boston University, Boston, MA 02215, USA. 3 Bioinformatics Program, Boston University, Boston, MA 02215, USA. 4These authors contributed equally: Ashley Penvose, Jessica L. Keenan. Correspondence -

IRF5 Gene Interferon Regulatory Factor 5
IRF5 gene interferon regulatory factor 5 Normal Function The protein produced from the IRF5 gene, called interferon regulatory factor 5 (IRF5), acts as a transcription factor, which means that it attaches (binds) to specific regions of DNA and helps control the activity of certain genes. When a virus is recognized in the cell, the IRF5 gene is turned on (activated), which leads to the production of IRF5 protein. The protein binds to specific regions of DNA that regulate the activity of genes that produce interferons and other cytokines. Cytokines are proteins that help fight infection by promoting inflammation and regulating the activity of immune system cells. In particular, interferons control the activity of genes that help block the replication of viruses, and they stimulate the activity of certain immune system cells known as natural killer cells. Health Conditions Related to Genetic Changes Systemic scleroderma Several normal variations in the IRF5 gene have been associated with an increased risk of developing systemic scleroderma, which is an autoimmune disorder characterized by the buildup of scar tissue (fibrosis) in the skin and internal organs. Although the IRF5 gene is known to stimulate the immune system in response to viruses, it is unknown how the gene variations contribute to the increased risk of systemic scleroderma. Researchers believe that a combination of genetic and environmental factors may play a role in development of the condition. Rheumatoid arthritis MedlinePlus Genetics provides information about Rheumatoid arthritis Systemic lupus erythematosus MedlinePlus Genetics provides information about Systemic lupus erythematosus Ulcerative colitis MedlinePlus Genetics provides information about Ulcerative colitis Reprinted from MedlinePlus Genetics (https://medlineplus.gov/genetics/) 1 Autoimmune disorders Studies have associated normal variations in the IRF5 gene with an increased risk of several autoimmune disorders. -

Tolerance to Sustained Activation of the Camp/Creb Pathway Activity in Osteoblastic Cells Is Enabled by Loss of P53 Mannu K
Walia et al. Cell Death and Disease (2018) 9:844 DOI 10.1038/s41419-018-0944-8 Cell Death & Disease ARTICLE Open Access Tolerance to sustained activation of the cAMP/Creb pathway activity in osteoblastic cells is enabled by loss of p53 Mannu K. Walia1, Scott Taylor1,PatriciaW.M.Ho1,T.JohnMartin1,2 and Carl R. Walkley 1,2,3 Abstract The loss of p53 function is a central event in the genesis of osteosarcoma (OS). How mutation of p53 enables OS development from osteoblastic lineage cells is poorly understood. We and others have reported a key role for elevated and persistent activation of the cAMP/PKA/Creb1 pathway in maintenance of OS. In view of the osteoblast lineage being the cell of origin of OS, we sought to determine how these pathways interact within the context of the normal osteoblast. Normal osteoblasts (p53 WT) rapidly underwent apoptosis in response to acute elevation of cAMP levels or activity, whereas p53-deficient osteoblasts tolerated this aberrant cAMP/Creb level and activity. Using the p53 activating small-molecule Nutlin-3a and cAMP/Creb1 activator forskolin, we addressed the question of how p53 responds to the activation of cAMP. We observed that p53 acts dominantly to protect cells from excessive cAMP accumulation. We identify a Creb1-Cbp complex that functions together with and interacts with p53. Finally, translating these results we find that a selective small-molecule inhibitor of the Creb1-Cbp interaction demonstrates selective toxicity to OS cells where this pathway is constitutively active. This highlights the cAMP/Creb axis as a potentially actionable therapeutic vulnerability in p53-deficient tumors such as OS. -

Induction of Myeloid Colony-Stimulating Activity in Murine Monocyte Tumor Cell Lines by Macrophage Activators and in a T-Cell Line by Concanavalin A1
[CANCER RESEARCH 38, 1414-1419, May 1978] Induction of Myeloid Colony-stimulating Activity in Murine Monocyte Tumor Cell Lines by Macrophage Activators and in a T-Cell Line by Concanavalin A1 Peter Ralph, Hal E. Broxmeyer,2 Malcolm A. S. Moore, and Ilona Nakoinz Sloan-Kettering Institute for Cancer Research, Rye, New York 10580 ABSTRACT activating agents and in T-lymphomas by T-lymphocyte mitogens. Certain fibrosarcoma lines in culture and the WEHI-3 myelomonocytic leukemia cell line have previously been shown to secrete myeloid colony-stimulating activity MATERIALS AND METHODS (CSA) spontaneously. We describe here other hemato- Murine Tumor Cell Lines. Monocyte and macrophage poietic tumor cell lines in which CSA is either produced tumor cell lines are described in Ref. 32, except for Abelson constitutively or inducible by immunostimulators. CSA leukemia virus-induced line RAW264 (33). T-lymphoma lines production in macrophage and monocyte tumor lines is EL4, RBL-5, BW5147, and S49; myelomas P3 and induced by lipopolysaccharide, zymosan, Mycobacterium MOPC315; mastocytoma P815; lymphoma P388; and Abel- strain Bacillus Calmette-Guerin, tuberculin purified pro son line R8 are described in Ref. 31. Rauscher leukemia tein-derivative preparation from mycobacteria, and dex- virus line RBL-3 and chemically induced leukemia L1210 tran sulfate. Myeloma, mastocytoma, and T-lymphoma (39) were obtained from K. Chang (NIH, Bethesda, Md.); lines do not produce CSA with or without these agents. In fibrosarcoma L929 (5) was obtained from B. Williams contrast, the T-lymphocyte mitogen concanavalin A (but (Sloan-Kettering Institute, Rye, N. Y.); bone marrow fibro- not phytohemagglutinin) induces CSA synthesis in one of blast JLSV9 and Rauscher leukemia virus-infected JLSV9- seven T-lymphomas tested. -

Genetics of Gene Expression in Primary Immune Cells Identifies Cell
ARTICLES Genetics of gene expression in primary immune cells identifies cell type–specific master regulators and roles of HLA alleles Benjamin P Fairfax1, Seiko Makino1, Jayachandran Radhakrishnan1, Katharine Plant1, Stephen Leslie2, Alexander Dilthey3, Peter Ellis4, Cordelia Langford4, Fredrik O Vannberg1,5 & Julian C Knight1 Trans-acting genetic variants have a substantial, albeit poorly characterized, role in the heritable determination of gene expression. Using paired purified primary monocytes and B cells, we identify new predominantly cell type–specific cis and trans expression quantitative trait loci (eQTLs), including multi-locus trans associations to LYZ and KLF4 in monocytes and B cells, respectively. Additionally, we observe a B cell–specific trans association of rs11171739 at 12q13.2, a known autoimmune disease locus, with IP6K2 (P = 5.8 × 10−15), PRIC285 (P = 3.0 × 10−10) and an upstream region of CDKN1A (P = 2 × 10−52), suggesting roles for cell cycle regulation and peroxisome proliferator-activated receptor γ (PPARγ) signaling in autoimmune pathogenesis. We also find that specific human leukocyte antigen (HLA) alleles form trans associations with the expression of AOAH and ARHGAP24 in monocytes but not in B cells. In summary, we show that mapping gene expression in defined primary cell populations identifies new cell type–specific trans-regulated networks and provides insights into the genetic basis of disease susceptibility. Defining the genetic determinants of gene expression is crucial to especially pertinent in the elucidation of trans-acting eQTLs, where understanding the biological and medical significance of genetic var- context specificity may be of greater relevance12. iation. This is particularly relevant in the drive to identify functional Here we sought to determine cell type–specific eQTLs relevant to variants underlying observed disease associations from genome- immunity and inflammation in paired samples of primary monocytes wide association studies (GWAS)1. -

Transcription Factor IRF4 Drives Dendritic Cells to Promote Th2 Differentiation
ARTICLE Received 30 May 2013 | Accepted 21 Nov 2013 | Published 20 Dec 2013 DOI: 10.1038/ncomms3990 Transcription factor IRF4 drives dendritic cells to promote Th2 differentiation Jesse W. Williams1, Melissa Y. Tjota2,3, Bryan S. Clay2, Bryan Vander Lugt4, Hozefa S. Bandukwala2, Cara L. Hrusch5, Donna C. Decker5, Kelly M. Blaine5, Bethany R. Fixsen5, Harinder Singh4, Roger Sciammas6 & Anne I. Sperling1,2,5 Atopic asthma is an inflammatory pulmonary disease associated with Th2 adaptive immune responses triggered by innocuous antigens. While dendritic cells (DCs) are known to shape the adaptive immune response, the mechanisms by which DCs promote Th2 differentiation remain elusive. Herein we demonstrate that Th2-promoting stimuli induce DC expression of IRF4. Mice with conditional deletion of Irf4 in DCs show a dramatic defect in Th2-type lung inflammation, yet retain the ability to elicit pulmonary Th1 antiviral responses. Using loss- and gain-of-function analysis, we demonstrate that Th2 differentiation is dependent on IRF4 expression in DCs. Finally, IRF4 directly targets and activates the Il-10 and Il-33 genes in DCs. Reconstitution with exogenous IL-10 and IL-33 recovers the ability of Irf4-deficient DCs to promote Th2 differentiation. These findings reveal a regulatory module in DCs by which IRF4 modulates IL-10 and IL-33 cytokine production to specifically promote Th2 differentiation and inflammation. 1 Committee on Molecular Pathogenesis and Molecular Medicine, University of Chicago, 924 E. 57th Street, Chicago, Illinois 60637 USA. 2 Committee on Immunology, University of Chicago, 924 E. 57th Street, Chicago, Illinois 60637 USA. 3 Medical Scientist Training Program, University of Chicago, 924 E. -

Molecular Pathogenesis and Regulation of the Mir-29-3P-Family: Involvement of ITGA6 and ITGB1 in Intra-Hepatic Cholangiocarcinoma
cancers Article Molecular Pathogenesis and Regulation of the miR-29-3p-Family: Involvement of ITGA6 and ITGB1 in Intra-Hepatic Cholangiocarcinoma Yuto Hozaka 1 , Naohiko Seki 2,* , Takako Tanaka 1, Shunichi Asai 2, Shogo Moriya 3, Tetsuya Idichi 1, Masumi Wada 1, Kiyonori Tanoue 1, Yota Kawasaki 1, Yuko Mataki 1 , Hiroshi Kurahara 1 and Takao Ohtsuka 1 1 Department of Digestive Surgery, Breast and Thyroid Surgery, Graduate School of Medical and Dental Sciences, Kagoshima University, Kagoshima 890-8520, Japan; [email protected] (Y.H.); [email protected] (T.T.); [email protected] (T.I.); [email protected] (M.W.); [email protected] (K.T.); [email protected] (Y.K.); [email protected] (Y.M.); [email protected] (H.K.); [email protected] (T.O.) 2 Department of Functional Genomics, Graduate School of Medicine, Chiba University, Chiba 260-8670, Japan; [email protected] 3 Department of Biochemistry and Genetics, Graduate School of Medicine, Chiba University, Chiba 260-8670, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-43-226-2971 Simple Summary: Even today, there are no effective targeted therapies for intrahepatic cholan- giocarcinoma (ICC) patients. Clarifying the molecular pathogenesis of ICC will contribute to the Citation: Hozaka, Y.; Seki, N.; development of treatment strategies for this disease. In this study, we searched for the role of the Tanaka, T.; Asai, S.; Moriya, S.; Idichi, miR-29-3p-family and its association with oncogenic pathway. Interestingly, aberrant expression of T.; Wada, M.; Tanoue, K.; Kawasaki, ITGA6 and ITGB1 was directly regulated by the miR-29-3p-family which are involved in multiple Y.; Mataki, Y.; et al. -
Genequery™ Human Stem Cell Transcription Factors Qpcr Array
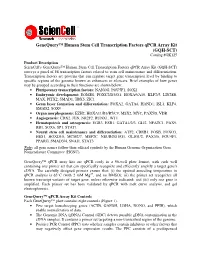
GeneQuery™ Human Stem Cell Transcription Factors qPCR Array Kit (GQH-SCT) Catalog #GK125 Product Description ScienCell's GeneQuery™ Human Stem Cell Transcription Factors qPCR Array Kit (GQH-SCT) surveys a panel of 88 transcription factors related to stem cell maintenance and differentiation. Transcription factors are proteins that can regulate target gene transcription level by binding to specific regions of the genome known as enhancers or silencers. Brief examples of how genes may be grouped according to their functions are shown below: • Pluripotency transcription factors: NANOG, POU5F1, SOX2 • Embryonic development: EOMES, FOXC2/D3/O1, HOXA9/A10, KLF2/5, LIN28B, MAX, PITX2, SMAD1, TBX5, ZIC1 • Germ layer formation and differentiation: FOXA2, GATA6, HAND1, ISL1, KLF4, SMAD2, SOX9 • Organ morphogenesis: EZH2, HOXA11/B3/B5/C9, MSX2, MYC, PAX5/8, VDR • Angiogenesis: CDX2, JUN, NR2F2, RUNX1, WT1 • Hematopoiesis and osteogenesis: EGR3, ESR1, GATA1/2/3, GLI2, NFATC1, PAX9, RB1, SOX6, SP1, STAT1 • Neural stem cell maintenance and differentiation: ATF2, CREB1, FOSB, FOXO3, HES1, HOXD10, MCM2/7, MEF2C, NEUROD1/G1, OLIG1/2, PAX3/6, POU4F1, PPARG, SMAD3/4, SNAI1, STAT3 Note : all gene names follow their official symbols by the Human Genome Organization Gene Nomenclature Committee (HGNC). GeneQuery™ qPCR array kits are qPCR ready in a 96-well plate format, with each well containing one primer set that can specifically recognize and efficiently amplify a target gene's cDNA. The carefully designed primers ensure that: (i) the optimal annealing temperature in qPCR analysis is 65°C (with 2 mM Mg 2+ , and no DMSO); (ii) the primer set recognizes all known transcript variants of target gene, unless otherwise indicated; and (iii) only one gene is amplified. -

Epigenetic Services Citations
Active Motif Epigenetic Services Publications The papers below contain data generated by Active Motif’s Epigenetic Services team. To learn more about our services, please give us a call or visit us at www.activemotif.com/services. Technique Target Journal Year Reference Justin C. Boucher et al. CD28 Costimulatory Domain- ATAC-Seq, Cancer Immunol. Targeted Mutations Enhance Chimeric Antigen Receptor — 2021 RNA-Seq Res. T-cell Function. Cancer Immunol. Res. doi: 10.1158/2326- 6066.CIR-20-0253. Satvik Mareedu et al. Sarcolipin haploinsufficiency Am. J. Physiol. prevents dystrophic cardiomyopathy in mdx mice. RNA-Seq — Heart Circ. 2021 Am J Physiol Heart Circ Physiol. doi: 10.1152/ Physiol. ajpheart.00601.2020. Gabi Schutzius et al. BET bromodomain inhibitors regulate Nature Chemical ChIP-Seq BRD4 2021 keratinocyte plasticity. Nat. Chem. Biol. doi: 10.1038/ Biology s41589-020-00716-z. Siyun Wang et al. cMET promotes metastasis and ChIP-qPCR FOXO3 J. Cell Physiol. 2021 epithelial-mesenchymal transition in colorectal carcinoma by repressing RKIP. J. Cell Physiol. doi: 10.1002/jcp.30142. Sonia Iyer et al. Genetically Defined Syngeneic Mouse Models of Ovarian Cancer as Tools for the Discovery of ATAC-Seq — Cancer Discovery 2021 Combination Immunotherapy. Cancer Discov. doi: doi: 10.1158/2159-8290 Vinod Krishna et al. Integration of the Transcriptome and Genome-Wide Landscape of BRD2 and BRD4 Binding BRD2, BRD4, RNA Motifs Identifies Key Superenhancer Genes and Reveals ChIP-Seq J. Immunol. 2021 Pol II the Mechanism of Bet Inhibitor Action in Rheumatoid Arthritis Synovial Fibroblasts. J. Immunol. doi: doi: 10.4049/ jimmunol.2000286. Daniel Haag et al. -

PU.1 Cooperates with IRF4 and IRF8 to Suppress Pre-B-Cell Leukemia
Leukemia (2016) 30, 1375–1387 © 2016 Macmillan Publishers Limited All rights reserved 0887-6924/16 www.nature.com/leu ORIGINAL ARTICLE PU.1 cooperates with IRF4 and IRF8 to suppress pre-B-cell leukemia SHM Pang1,2, M Minnich3, P Gangatirkar1,2, Z Zheng1, A Ebert3, G Song4, RA Dickins1,2,5, LM Corcoran1,2, CG Mullighan4, M Busslinger3, ND Huntington1,2, SL Nutt1,2 and S Carotta1,2,6 The Ets family transcription factor PU.1 and the interferon regulatory factor (IRF)4 and IRF8 regulate gene expression by binding to composite DNA sequences known as Ets/interferon consensus elements. Although all three factors are expressed from the onset of B-cell development, single deficiency of these factors in B-cell progenitors only mildly impacts on bone marrow B lymphopoiesis. Here we tested whether PU.1 cooperates with IRF factors in regulating early B-cell development. Lack of PU.1 and IRF4 resulted in a partial block in development the pre-B-cell stage. The combined deletion of PU.1 and IRF8 reduced recirculating B-cell numbers. Strikingly, all PU.1/IRF4 and ~ 50% of PU.1/IRF8 double deficient mice developed pre-B-cell acute lymphoblastic leukemia (B-ALL) associated with reduced expression of the established B-lineage tumor suppressor genes, Ikaros and Spi-B. These genes are directly regulated by PU.1/IRF4/IRF8, and restoration of Ikaros or Spi-B expression inhibited leukemic cell growth. In summary, we demonstrate that PU.1, IRF4 and IRF8 cooperate to regulate early B-cell development and to prevent pre-B-ALL formation.