Board of Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
COVID-19 Vaccine Implementation Committee – Sudbury East
COVID-19 Vaccine Implementation Committee – Sudbury East TERMS OF REFERENCE O: January 2021 As a local public health agency with responsibilities under the Ontario Public Health Standards for immunization and infectious and communicable disease control, Public Health Sudbury & Districts has the overall responsibility for the unprecedented COVID-19 Vaccination Program. This responsibility is executed in close collaboration with others in health care and non-health care sectors. The work of the COVID-19 Vaccine Implementation Committee for Sudbury East will be informed by the Public Health Sudbury & Districts COVID-19 Vaccination Program Playbook which provides the essential pillars/overarching framework for the development of geographic and sector-specific implementation plans to outline a coordinated approach for vaccine program. This monumental collective effort will ensure that the overall objectives of the Public Health Sudbury & Districts COVID-19 Vaccination Program are achieved. These objectives include: 1. Minimize societal disruptions, including infrastructure and economic impacts. 2. Implement sustained public education and community outreach efforts. 3. Maintain public confidence. 4. Achieve a coverage rate of 75% of those eligible for vaccine by the provincially prescribed timelines. Purpose To ensure the implementation of the Public Health Sudbury & Districts Vaccination Program in the Sudbury East area. The Vaccine Implementation Committees are established for the five geographic clusters within Public Health Sudbury & Districts. This committee structure recognizes that while adherence to core elements of the Vaccination Program is required (e.g. sequencing of priority groups, vaccine storage and handling, COVID-safe measures, key communications, etc.), actual implementation will look different across the region. Health system capacity, vaccine availability, administrative supports, population density, and community infrastructure are all characteristics that will impact on how vaccines are most effectively delivered across the region. -

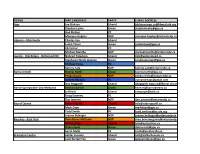
2018 Election New Democratic Party of Ontario Candidates
2018 Election New Democratic Party of Ontario Candidates NAME RIDING CONTACT INFORMATION Monique Hughes Ajax [email protected] Michael Mantha Algoma-Manitoulin [email protected] Pekka Reinio Barrie-Innisfil [email protected] Dan Janssen Barrie-Springwater-Ono- [email protected] Medonte Joanne Belanger Bay of Quinte [email protected] Rima Berns-McGown Beaches-East York [email protected] Sara Singh Brampton Centre [email protected] Gurratan Singh Brampton East [email protected] Jagroop Singh Brampton West [email protected] Alex Felsky Brantford-Brant [email protected] Karen Gventer Bruce-Grey-Owen Sound [email protected] Andrew Drummond Burlington [email protected] Marjorie Knight Cambridge [email protected] Jordan McGrail Chatham-Kent-Leamington [email protected] Marit Stiles Davenport [email protected] Khalid Ahmed Don Valley East [email protected] Akil Sadikali Don Valley North [email protected] Joel Usher Durham [email protected] Robyn Vilde Eglinton-Lawrence [email protected] Amanda Stratton Elgin-Middlesex-London [email protected] NAME RIDING CONTACT INFORMATION Taras Natyshak Essex [email protected] Mahamud Amin Etobicoke North [email protected] Phil Trotter Etobicoke-Lakeshore [email protected] Agnieszka Mylnarz Guelph [email protected] Zac Miller Haliburton-Kawartha lakes- [email protected] -

September 26, 2002
Manitoulin-Sudbury DSSAB September 26, 2002 MINUTES of the DSSAB BOARD MEETING held in its Espanola Office Boardroom September 26, 2002 Present: Jack Barr, Pat Best, Gary Brown, Raymond Chénier, Earle Freeborn, Les Gamble, Frank Gillis, Willy Léveillée, Marcel Rancourt, Dale Van Every, Janet Whissell Staff: Gary Champagne, CAO Suzanne Bouchard, E.A. (Recording Secretary) Connie Morphet, Finance and Administration Manager Fern Dominelli, Ontario Works Program Manager Peter Bradley, Housing Services Manager Dan Hammond, EMS Manager Karen Dominick, Community Services Manager Regrets: Ken Ferguson, Vince Lacroix, Lucie Lemieux Media: Cheryl Waugh, Manitoulin Expositor 1.0 CALL TO ORDER The Chair, Ray Chénier, called the meeting to order at 9:05 a.m. 2.0 CLOSED SESSION Resolution No. 02-129 Moved by: Willy Léveillée Seconded by: Jack Barr THAT the Board move into closed session to discuss Property and Human Resource matters. Carried Resolution No. 02-130 Moved by: Earle Freeborn Seconded by: Frank Gillis THAT the Board adjourn this closed session. Carried 3.0 ADOPTION OF AGENDA Resolution No. 02-131 Moved by: Earle Freeborn Seconded by: Jack Barr That the agenda be adopted with the addition of Karen Dominick re EYC in item #5 – Delegations. Carried 1 Manitoulin-Sudbury DSSAB September 26, 2002 Announcement - Raymond Chénier announced that Frank Gillis has been elected President of NOSDA for the coming twelve months. 4.0 DECLARATIONS OF CONFLICT OF INTEREST There were no declarations of conflict of interest. 5.0 DELEGATIONS 5.1 - M.C. Faggioni & Assoc. – Pay Equity Gary Champagne introduced Mr. Marcel Faggioni, the consultant engaged to look into the Pay Equity question for the DSSAB. -

Ontario Members of Provincial Parliament
Ontario Members of Provincial Parliament Government Office Constituency Office Government Office Constituency Office Sophia Aggelonitis, Parliamentary Assistant to the Laura Albanese, Parliamentary Assistant to the Minister of Small Business and Entrepreneurship Minister of Culture Hamilton Mountain, Liberal York South-Weston, Liberal Ministry of Small Business and Unit 2 - 952 Concession St Ministry of Culture Unit 102 - 2301 Keele St Entrepreneurship Hamilton ON L8V 1G2 900 Bay Street, 4th Floor, Toronto ON M6M 3Z9 1309 - 99 Wellesley St W, 1st Tel : 905-388-9734 Mowat Block Tel : 416-243-7984 Flr, Whitney Block Fax : 905-388-7862 Toronto ON M7A 1L2 Fax : 416-243-0327 Toronto ON M7A 1W2 saggelonitis.mpp.co Tel : 416-325-1800 [email protected] Tel : 416-314-7882 @liberal.ola.org Fax : 416-325-1802 Fax : 416-314-7906 [email protected] [email protected] Ted Arnott Wayne Arthurs, Parliamentary Assistant to the Wellington-Halton Hills, Progressive Conservative Minister of Finance Rm 420, Main Legislative 181 St. Andrew St E, 2nd Flr Pickering-Scarborough East, Liberal Building Fergus ON N1M 1P9 Ministry of Finance 13 - 300 Kingston Rd Toronto ON M7A 1A8 Tel : 519-787-5247 7 Queen's Park Cres, 7th Flr, Pickering ON L1V 6Z9 Tel : 416-325-3880 Fax : 519-787-5249 Frost Bldg South Tel : 905-509-0336 Fax : 416-325-6649 Toll Free : 1-800-265-2366 Toronto ON M7A 1Y7 Fax : 905-509-0334 [email protected] [email protected] Tel : 416-325-3581 Toll-Free: 1-800-669-4788 Fax : 416-325-3453 [email protected] -
Greater Sudbury Source Protection Area Assessment Report
Greater Sudbury Source Protection Area Assessment Report Approved on September 2, 2014 Greater Sudbury Source Protection Area Assessment Report The Greater Sudbury Source Protection Area Assessment Report Introduction Limitations of this Report ......................................................................................... 13 Executive Summary ................................................................................................. 14 Sommaire ................................................................................................................ 18 Acknowledgements ................................................................................................. 21 Foreword ................................................................................................................. 22 Preface .................................................................................................................... 24 Part 1 – Report Overview and Methodology Chapter 1 - Overview of the Assessment Report .................................................... 1-5 Chapter 2 - Water Quality Risk Assessment ........................................................... 1-9 Chapter 3 - Water Quantity Risk Assessment ...................................................... 1-23 Part 2 – The Greater Sudbury Source Protection Area Chapter 4 - The Greater Sudbury Source Protection Area: A Tale of Three Rivers 2-5 Chapter 5 - Drinking Water Systems ...................................................................... 2-7 Chapter -

PEO GOVERNMENT LIAISON PROGRAM Volume 14, 2020 GLP WEEKLY Issue 28
August 21, PEO GOVERNMENT LIAISON PROGRAM Volume 14, 2020 GLP WEEKLY Issue 28 PEO PRESIDENT SHARES GOALS WITH THE GOVERNMENT LIAISON COMMITTEE The PEO Government Liaison Committee (GLC) held its monthly meeting online on August 19. Joining them was PEO President Marisa Sterling, P.Eng (above), who discussed her 10 year vision for PEO with the Committee. Also attending the meeting were PEO’s GLC Chair Warren Turnbull, P.Eng., Councillor Lorne Cutler, P.Eng., Engineers Canada rep Changiz Sadr, P.Eng., Chapter rep Gabe Tse, P.Eng., Advisory Committee Volunteer rep Vicki Hilborn, P.Eng., active riding association member Jeffrey Lee, P.Eng., EIT rep Alex Weryha, EIT, student rep Shawn Yanni, Manager, Government Liaison Programs Jeannette Chau, P.Eng. and Government Relations Consultant Howard Brown. For more on this story, see page 3. Through the Professional Engineers Act, PEO governs over 89,000 licence and certificate holders, and regulates and advances engineering practice in Ontario to protect the public interest. Professional engineering safeguards life, health, property, economic interests, the public welfare and the environment. Past issues are available on the PEO Government Liaison Program (GLP) website at https://www.peo.on.ca/index.php/about-peo/glp-weekly- newsletter Deadline for submissions is the Thursday of the week prior to publication. The next issue will be published on August 28, 2020. 1 | PAGE TOP STORIES THIS WEEK 1. MINISTER, PARTY LEADER AND MPPS HOLD EVENTS 2. PEO GLP REP SHARES HIS INSIGHTS ON THE IMPORTANCE OF THE GLP PEO GOVERNMENT LIAISON PROGRAM WORKS The PEO Government Liaison Committee held their monthly virtual meeting this week, and were joined by PEO President Marisa Sterling, P.Eng. -
RIDING MPP CANDIDATE PARTY E-MAIL ADDRESS Ajax Joe
RIDING MPP CANDIDATE PARTY E-MAIL ADDRESS Ajax Joe Dickson Liberal [email protected] Stephen Leahy Green [email protected] Rod Phillips PC Monique Hughes NDP [email protected] Algoma—Manitoulin Charles Fox Liberal Justin Tilson Green [email protected] Jib Turner PC Michael Mantha NDP [email protected] Aurora - Oak Ridges - Richmond Hill Naheed Yaqubian Liberal [email protected] Stephanie Nicole Duncan Green [email protected] Michael Parsa PC Katrina Sale NDP [email protected] Barrie-Innisfil Bonnie North Green [email protected] Pekka Reinio NDP [email protected] Andrea Khanjin PC [email protected] Ann Hoggarth Liberal [email protected] Barrie-Springwater-Oro-Medonte Keenan Aylwin Green [email protected] Jeff Kerk Liberal [email protected] Doug Downey PC Dan Janssen NDP [email protected] Bay of Quinte Robert Quaiff Liberal [email protected] Mark Daye Green [email protected] Todd Smith PC [email protected] Joanne Belanger NDP [email protected] Beaches—East York Rima Berns-McGown NDP [email protected] Arthur Potts Liberal [email protected] Debra Scott Green [email protected] Sarah Mallo PC [email protected] Brampton Centre Safdar Hussain Liberal [email protected] Laila Zarrabi Yan Green [email protected] Harjit Jaswal PC [email protected] Sara Singh NDP [email protected] Brampton East Dr. Parminder Singh Liberal [email protected] Raquel Fronte Green [email protected] Sudeep Verma PC Gurratan -

2019 EXHIBITORS LISTING As of August 15, 2019 OUTDOOR EXHIBITORS Epicure, North Bay
2019 EXHIBITORS LISTING As of August 15, 2019 OUTDOOR EXHIBITORS Epicure, North Bay .............................................5A 32 Agriculture Tent .............................................2B 13-18 Equipment North Inc., Lively ......................... 3A 21 AJM Pellets Inc., Monetville ............................3B 19 Essential Helicopters, North Bay ............East 2 Antiques and Historical Displays .........East 3 & 4 Family Centre and Lost Persons Tent ...4A 13-14 Artisan Tent ....................................................5B 30-34 Fellowship of Christian Farmers Canada, Battery Battery, North Bay ...............................1B 32 Alexandria .....................................................3A 36 Beugger Energy Equipment, Final Furrow Lounge ...................................1A 31-38 Standbridge Station, QC .......................... 5A 18 Flexxifinger QD Industries Inc., BMO Bank of Montreal .........................4A 27-35 Assiniboia ................................................SK 2A 18 Bow & Arrow, Sturgeon Falls .......................... 5A 31 Furnishings Plus, Brantford ......................3A 27-28 Brownlee Equipment, Earlton ............2B 27-28 Future IPMs Tent ............................................4B 13-15 Bugnot Stone Crushers & Forestry Mulchers, Gospel Focus, Kirkfield .............................. 3B 31-32 Casselman ............................................... 2B 31-33 Grain Farmers of Ontario Tech Park .4A 04-08 Cambrian College .......................................1B 30 Grain -

Student Alliance
ONTARIO UNDERGRADUATE STUDENT ALLIANCE ADVOCACY CONFERENCE 2020 November 16-19th ABOUT OUSA The Ontario Undergraduate Student Alliance (OUSA) represents the interests of approximately 150,000 professional and undergraduate, full-time and part-time university students at eight student associations across Ontario. Our vision is for an accessible, affordable, accountable and high quality post-secondary education in Ontario. OUSA’s approach to advocacy is based on creating substantive, student driven, and evidence-based policy recommendations. INTRODUCTION Student leaders representing over 150,000 undergraduate students from across Ontario attended OUSA’s annual Student Advocacy Conference from November 16th to the 19th. Delegates met with over 50 MPPs from four political parties and sector stakeholders to discuss the future of post-secondary education in Ontario and advance OUSA’s advocacy priorities. Over five days, the student leaders discussed student financial aid, quality of education, racial equity, and student mental health. As we navigate the global pandemic, OUSA recommends improvements to the Ontario Student Assistance Program (OSAP), guidance and support for quality online learning, training and research to support racial equity, and funding for student mental health services. Overall, OUSA received a tremendous amount of support from members and stakeholders. ATTENDEES Julia Periera (WLUSU) Eric Chappell (SGA-AGÉ) Devyn Kelly (WLUSU) Nathan Barnett (TDSA) Mackenzy Metcalfe (USC) Rayna Porter (TDSA) Matt Reesor (USC) Ryan Tse (MSU) Megan Town (WUSA) Giancarlo Da-Ré (MSU) Abbie Simpson (WUSA) Tim Gulliver (UOSU-SÉUO) Hope Tuff-Berg (BUSU) Chris Yendt (BUSU) Matthew Mellon (AMS) Alexia Henriques (AMS) Malek Abou-Rabia (SGA-AGÉ) OUSA MET WITH A VARIETY OF STAKEHOLDERS MPPS CABINET MINISTERS Minister Michael Tibollo MPP Stephen Blais Office of Minister Monte McNaughton MPP Jeff Burch Office of Minister Peter Bethlenfalvy MPP Teresa Armstrong . -

Second Report from the Mayor's Economic And
We’re all in this together Second Report from the Mayor’s Economic and Social Impact and Recovery Task Forces 8 May 2020 Introduction 2 Progress so far 3 Ideas for Action 6 During the shutdown 6 Grants rather than loans or deferrals for commercial rent (already actioned) 6 Pooling resources or collaborating to allow smaller organizations access to EAP services like counselling 6 Insurance companies should reduce premiums to reflect changes in economic activity and mobility 7 Consider distributing funds though existing organizations like Regional Innovation Centres 7 Delivery food on a regular basis to agencies that provide food to people 7 Maximize number of people receiving support through discretionary benefits 7 Supporting physical distancing by people who are living unsheltered 7 Communicate government programs via widely available print publications that are delivered 7 Continuing transit service to make sure people can continue to move around the city for essential trips 8 Significant increases in funding for mental health for children and youth 8 Clarify how psychotherapists can provide emergency counselling 8 Broaden distribution of comfort stations to include Hamilton Road 8 Providing blankets to agencies working with people experiencing homelessness 8 Expand the number of monthly rent supplements 8 Creating more space to provide shelter 8 Connecting faith communities to support service agencies 9 Supporting the specific needs of international students 9 During the recovery 9 Rapid shift to office employees working remotely should -

COVID-19 Vaccine Implementation Committee – Sudbury East
COVID-19 Vaccine Implementation Committee – Sudbury East TERMS OF REFERENCE O: January 2021 As a local public health agency with responsibilities under the Ontario Public Health Standards for immunization and infectious and communicable disease control, Public Health Sudbury & Districts has the overall responsibility for the unprecedented COVID-19 Vaccination Program. This responsibility is executed in close collaboration with others in health care and non-health care sectors. The work of the COVID-19 Vaccine Implementation Committee for Sudbury East will be informed by the Public Health Sudbury & Districts COVID-19 Vaccination Program Playbook which provides the essential pillars/overarching framework for the development of geographic and sector-specific implementation plans to outline a coordinated approach for vaccine program. This monumental collective effort will ensure that the overall objectives of the Public Health Sudbury & Districts COVID-19 Vaccination Program are achieved. These objectives include: 1. Minimize societal disruptions, including infrastructure and economic impacts. 2. Implement sustained public education and community outreach efforts. 3. Maintain public confidence. 4. Achieve a coverage rate of 75% of those eligible for vaccine by the provincially prescribed timelines. Purpose To ensure the implementation of the Public Health Sudbury & Districts Vaccination Program in the Sudbury East area. The Vaccine Implementation Committees are established for the five geographic clusters within Public Health Sudbury & Districts. This committee structure recognizes that while adherence to core elements of the Vaccination Program is required (e.g. sequencing of priority groups, vaccine storage and handling, COVID-safe measures, key communications, etc.), actual implementation will look different across the region. Health system capacity, vaccine availability, administrative supports, population density, and community infrastructure are all characteristics that will impact on how vaccines are most effectively delivered across the region. -

September 11, 2018 7:00 P.M
The Niagara Catholic District School Board through the charisms of faith, social justice, support and leadership, nurtures an enriching Catholic learning community for all to reach their full potential and become living witnesses of Christ. AGENDA AND MATERIAL COMMITTEE OF THE WHOLE MEETING TUESDAY, SEPTEMBER 11, 2018 7:00 P.M. FATHER KENNETH BURNS, C.S.C. BOARD ROOM CATHOLIC EDUCATION CENTRE, WELLAND, ONTARIO A. ROUTINE MATTERS 1. Opening Prayer – Trustee Burtnik - 2. Roll Call - 3. Approval of the Agenda - 4. Declaration of Conflict of Interest - 5. Approval of Minutes of the Committee of the Whole Meeting - 5.1 June 12, 2018 A5.1 5.2 June 20, 2018 A5.2 6. Consent Agenda Items - 6.1 Architect Selection for Monsignor Clancy Catholic Elementary School and A6.1 Our Lady of Mount Carmel Catholic Elementary School 6.2 Staff Development Department Professional Development Opportunities A6.2 6.3 In Camera Items F1.1, F1.2 and F4 - B. PRESENTATIONS C. COMMITTEE AND STAFF REPORTS 1. Director of Education and Senior Staff Introduction to the 2018-2019 School Year C1 2. Provisions of Special Education Programs and Services - Special Education Plan C2 3. Niagara Compliance Audit Committee Report C3 4. Monthly Updates 4.1 Student Senate Update - 4.2 Senior Staff Good News Update - D. INFORMATION 1. Trustee Information 1.1 Spotlight on Niagara Catholic – June 19, 2018 D1.1 1.2 Calendar of Events – September 2018 D1.2 2 1.3 Ontario Legislative Highlights – June 22, 2018, July & August 2018 D1.3 1.4 Letter to Parents and Guardians – September 2018 D1.4 1.5 Niagara Foundation for Catholic Education Golf Tournament – September 19, 2018 D1.5 1.6 OCSTA 2018 Fall Regional Meeting – September 26, 2018 D1.6 1.7 OCSTA 2018 Fall Regional Meeting Questions for Discussion D1.7 E.