EANS/UEMS European Examination in Neurosurgery Part I (Written) Variants of Questions with Answers (Compilation - Vyacheslav S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cory Newman Thesis 5-2021 Signed.Pdf (1.303Mb)
DocuSign Envelope ID: 4851A328-CF63-4770-A833-B4246E7E5D23 Simulating Homonymous Hemianopsia for the Care Team by Cory Newman May 2021 Presented to the Division of Science, Information Arts, and Technologies University of Baltimore In Partial Fulfillment of the Requirements for the Degree of Master of Science 5/25/2021 Approved by: ________________________________ [name, Thesis Advisor] ________________________________5/25/2021 [name, Committee Member] i DocuSign Envelope ID: 4851A328-CF63-4770-A833-B4246E7E5D23 Abstract Homonymous hemianopsia is a visual impairment that involves the bilateral loss of a complete visual field. While research has been done to ascertain the details of cause and prognosis of homonymous hemianopsia, an obvious disparity arose in the research on how to educate the supporting care team of a person with homonymous hemianopsia to maximize the creation of educational and rehabilitation plans. This research presents two studies focused on closing that gap by providing an alternative method of understanding. In the initial study 16 participants with a confirmed caregiver relationship to one or more persons with homonymous hemianopsia were surveyed on their personal knowledge of the visual impairment. These participants were asked to express any visual obstacles they have encountered, and to ascertain the availability of a device or program that could provide an interactive interpretation of how their homonymous hemianopsia patient views their surroundings. Survey results confirmed the need for a program that could easily simulate homonymous hemianopsia for the care provider. An additional usability study was completed by eight of the 16 previous participants on a mobile homonymous hemianopsia simulation application prototype. User tests showed that participants gained a significant increase in understanding of how those with a homonymous hemianopsia visual impairment view the environment. -

Homonymous Hemianopsia
Source: CLEVELAND CLINIC OHIO USA FACTSHEET Homonymous Hemianopsia Homonymous hemianopsia is a condition in which a person sees only one side - right or left of the visual world of each eye; results from a problem in brain function rather than a disorder of the eyes themselves. This can happen after a head or brain injury. What is homonymous hemianopsia? Homonymous hemianopsia is a condition in which a person sees only one side―right or left―of the visual world of each eye. The person may not be aware that the vision loss is happening in both eyes, not just one. Under normal circumstances, the left half of the brain processes visual information from both eyes about the right side of the world. The right side of the brain processes visual information from both eyes about the left side of the world. A visual world of someone with normal vision A visual world of someone with homonymous hemianopsia In homonymous hemianopsia, an injury to the left part of the brain results in the loss of the right half of the visual world of each eye. An injury to the right part of the brain produces loss of the left side of the visual world of each eye. This condition is created by a problem in brain function rather than a disorder of the eyes themselves. What causes homonymous hemianopsia? The most common cause of this type of vision loss is stroke. However, any disorder that affects the brain—including tumours, inflammation, and injuries--can be a cause. Source: CLEVELAND CLINIC OHIO USA It is estimated that 70% of the injuries leading to hemianopsias are due to an obstruction (blockage) of the blood supply (stroke). -
Oct Institute
Low Vision, Visual Dysfunction and TBI – Treatment, Considerations, Adaptations Andrea Hubbard, OTD, OTR/L, LDE Objectives • In this course, participants will: 1. Learn about interventions involving specialized equipment to adapt an environment for clients with low vision. 2. Learn about the most typical low vision presentations/conditions. 3. Gain increased knowledge of eye anatomy and the visual pathway. Overview of TBI Reference: Centers for Disease Control and Prevention Overview of TBI Risk Factors for TBI Among non-fatal TBI-related injuries for 2006–2010: • Men had higher rates of TBI hospitalizations and ED visits than women. • Hospitalization rates were highest among persons aged 65 years and older. • Rates of ED visits were highest for children aged 0-4 years. • Falls were the leading cause of TBI-related ED visits for all but one age group. – Assaults were the leading cause of TBI-related ED visits for persons 15 to 24 years of age. • The leading cause of TBI-related hospitalizations varied by age: – Falls were the leading cause among children ages 0-14 and adults 45 years and older. – Motor vehicle crashes were the leading cause of hospitalizations for adolescents and persons ages 15-44 years. Reference: Centers for Disease Control and Prevention Overview of TBI Risk Factors for TBI Among TBI-related deaths in 2006–2010: • Men were nearly three times as likely to die as women. • Rates were highest for persons 65 years and older. • The leading cause of TBI-related death varied by age. – Falls were the leading cause of death for persons 65 years or older. -
VISUAL FIELD Pathway Extends from the „Front‟ to the „Back‟ of the RETINA Brain
NOTE: To change the image on this slide, select the picture and delete it. Then click the Pictures icon in the placeholde r to insert your own image. Visual Pathway Disorders Amr Hassan, MD, FEBN Associate professor of Neurology - Cairo University Optic nerve • Anatomy of visual pathway • How to examine • Visual pathway disorders • Quiz 2 Optic nerve • Anatomy of visual pathway • How to examine • Visual pathway disorders • Quiz 3 Optic nerve The Visual Pathway VISUAL FIELD Pathway extends from the „front‟ to the „back‟ of the RETINA brain. ON OC OT LGN OPTIC RADIATIONS ON = Optic Nerve OC = Optic Chiasm OT = Optic Tract LGN = Lateral Geniculate Nucleus of Thalamus VISUAL CORTEX 5 The Visual Pathway Eyes & Retina Light >> lens >> retina (inverted and reversed image). Eyes & Retina Eyes & Retina • Macula: oval region approximately 3-5 mm that surrounds the fovea, also has high visual acuity. • Fovea: central fixation point of each eye// region of the retina with highest visual acuity. Eyes & Retina • Optic disc: region where axons leaving the retina gather to form the Optic nerve. Eyes & Retina • Blind spot located 15° lateral and inferior to central fixation point of each eye. Object to be seen Peripheral Retina Central Retina (fovea in the macula lutea) 12 Photoreceptors © Stephen E. Palmer, 2002 Photoreceptors Cones • Cone-shaped • Less sensitive • Operate in high light • Color vision • Less numerous • Highly represented in the fovea >> have high spatial & temporal resolution >> they detect colors. © Stephen E. Palmer, 2002 Photoreceptors Rods • Rod-shaped • Highly sensitive • Operate at night • Gray-scale vision • More numerous than cons- 20:1, have poor spatial & temporal resolution of visual stimuli, do not detect colors >> vision in low level lighting conditions © Stephen E. -

Visual Field Recovery - Case Report of a Patient with Left Homonymous Hemianopsia Post-Stroke
CopyrightMedical © Marsha & Davis Surgical Benshir CRIMSON PUBLISHERS C Wings to the Research Ophthalmology Research ISSN 2578-0360 Case Report Visual Field Recovery - Case Report of a Patient with Left Homonymous Hemianopsia Post-Stroke Marsha Davis Benshir* Center for Vision Development, USA *Corresponding author: Marsha Davis Benshir, Center for Vision Development, 164 W Main St Ste. B New Market, MD 21774, USA Submission: February 06, 2018; Published: March 23, 2018 Abstract have spontaneous recovery and others will adapt through physical and occupational therapy. Vision rehabilitation modeled on other widely used types of therapyVisual post-strokefield loss from has stroke been demonstratedoccurs in up to to 50% restore of patients peripheral requiring vision hospitalization in some patients for beyond rehabilitation the expected after stroke window [1]. for Of spontaneousthese patients recovery many will of peripheral vision. Introduction Optometrists specializing in Neuro-optometric rehabilitation study in Rotterdam, Netherlands, glaucoma was the leading cause have been working with physiatrists, neurologists and other falling. In patients over 85 the incidence is closer to 1:6. In one rehabilitation specialist for decades, and have demonstrated that [5]. of visual field loss followed by other optic nerve disease and stroke expected time for recovery. The research proving that therapy can Case Report visual field recovery is possible for many patients beyond the be effective is being done by neurologists who have demonstrated This patient was a previously healthy 60 y.o. right-handed male re-wiring of neural pathways with improved performance after who developed sudden left side facial weakness, confusion and repetitive visual-motor tasks and recovery of somatosensory and disorientation on the way home from work. -

Visual Impairment Age-Related Macular
VISUAL IMPAIRMENT AGE-RELATED MACULAR DEGENERATION Macular degeneration is a medical condition predominantly found in young children in which the center of the inner lining of the eye, known as the macula area of the retina, suffers thickening, atrophy, and in some cases, watering. This can result in loss of side vision, which entails inability to see coarse details, to read, or to recognize faces. According to the American Academy of Ophthalmology, it is the leading cause of central vision loss (blindness) in the United States today for those under the age of twenty years. Although some macular dystrophies that affect younger individuals are sometimes referred to as macular degeneration, the term generally refers to age-related macular degeneration (AMD or ARMD). Age-related macular degeneration begins with characteristic yellow deposits in the macula (central area of the retina which provides detailed central vision, called fovea) called drusen between the retinal pigment epithelium and the underlying choroid. Most people with these early changes (referred to as age-related maculopathy) have good vision. People with drusen can go on to develop advanced AMD. The risk is considerably higher when the drusen are large and numerous and associated with disturbance in the pigmented cell layer under the macula. Recent research suggests that large and soft drusen are related to elevated cholesterol deposits and may respond to cholesterol lowering agents or the Rheo Procedure. Advanced AMD, which is responsible for profound vision loss, has two forms: dry and wet. Central geographic atrophy, the dry form of advanced AMD, results from atrophy to the retinal pigment epithelial layer below the retina, which causes vision loss through loss of photoreceptors (rods and cones) in the central part of the eye. -

Definition of Stroke/Brain Attack
Definition of Stroke/Brain Attack Stroke II: • A syndrome caused by disruption in the flow of Diagnosis, Evaluation, and Prevention blood to part of the brain due to either: – occlusion of a blood vessel • ischemic stroke Lenore N. Joseph, MD – rupture of a blood vessel Neurology Service Chief, McGuire VAMC • hemorrhagic stroke Assistant Professor of Neurology • The interruption in blood flow deprives the brain VCU Health System of nutrients and oxygen resulting in injury to cells Medical College of Virginia in the affected vascular territory of the brain 1 2 Stroke: The Problem Stroke: The Problem • Third leading cause of death in US • Among 6 month or longer survivors: – after heart disease and cancer – 48% have a hemiparesis • 740,000 new strokes each year – 22% cannot walk • 4.5 million stroke survivors – 24-53% report complete or partial • Leading cause of disability in adults in US dependence for activities • $45.5 billion per year in the USA – 12-18% are aphasic • 1 of 6 Americans will be affected – 32% are clinically depressed – only 10% fully recover 3 4 Symptoms of Brain Attack: Symptoms of Brain Attack: Teach your patients! Teach your patients! • Sudden weakness, paralysis, or numbness of: • Sudden unexplained dizziness –face – especially when associated with other – arm and the leg on one or both sides of the neurologic symptoms body – unsteadiness • Sudden loss of speech, or difficulty speaking or – sudden falls understanding speech • Sudden severe headache and/or loss of • Sudden dimness or loss of vision consciousness – -

Rehabilitation of Patients with Acquired Brain Injury Introduction
Introduction - TIRR • The Institute for Rehabilitation of Patients Rehabilitation and Research – In-patient & with Acquired Brain Injury Out-patient Programs • Ranked within the top 5 rehabilitation hospitals in Kia B. Eldred, OD, FAAO, the US for 20 years Diplomate in Low Vision • Affiliation with University of Michael E. DeBakey VA Medical Center Houston College of University of Houston College of Optometry Optometry for 23 years Michael E. DeBakey HVAMC & Project Victory Categories of Brain Injuries • ~30,680 US soldiers wounded in Iraq & • Traumatic Brain injury Afghanistan – TBI is the “signature wound” • Non- traumatic brain injury – 20% of injuries are serious ABI or SCI – 1800 troops suffering from penetrating TBI • Now defined as “Acquired” (ABI) –> – 3000 soldiers being treated for severe TBI Includes stroke – 30% of troops engaged in combat > 4 – Ischemic: 80% months are at risk for disabling neurologic disorders from blast waves of IEDs – Hemorrhagic: 20% – 60% of injuries are due to roadside bombs & IEDs (improvised explosive devices) – 30% of soldiers develop mental health problems (PTSD) within 3-4 months of returning to the US Shearing & Traumatic Brain Injury Contusions • Closed head injury – denotes that the dura remains intact • Open head injury – denotes that the dura was opened • Penetrating head injury – denotes that a foreign object penetrated the dura and entered the brain http://www.biak.us/images/brain2.jpg http://www.doctorlawyer.net/images/ClosedHeadInjury.jpg 1 Subdural & Epidural Hemorrhages Non- traumatic -

West Los Angeles VA Health Care Center, Los Angeles, CA
West Los Angeles VA Health Care Center, Los Angeles, CA LECTURE/EDUCATIONAL PRESENTATIONS BY WLAVA OPTOMETRY RESIDENTS 2017-2018 Dr. Holly Hickerson Anemic retinopathy (August 2017) Polypoidal choroidal vascularization (October, December 2017; April 2018; June 2018) “Heavy eye” and “sagging eye” syndromes (October 2017, February 2018) Dr. Mark Lii Outer retinal tubulation (September, December 2017; March, June 2018) Mucus fishing syndrome (March 2018) Dr. Benjamin Magno Ocular nutrition (September 2017) Ocular manifestations of sarcoidosis (November 2017, March, June 2018) Neuro-optometry case presentation (March 2018) Dr. Sandra Zhang Uveal Effusion syndrome (September 2017, November 2017, March 2018) Retinitis Pigmentosa case presentation (March 2018) 2016-2017 Dr. Piper Bahr Pigment Dispersion Syndrome (August 2016) Systemic Imaging case presentation (September 2016) Lipemia Retinalis (November 2016, March 2017, May 2017, June 2017) Dr. Ellen McCrary Lymphoproliferative disorders (August 2016, November 2016, March 2017, May 2017, June 2017) Low Vision Overview (December 2016) Horner’s Syndrome (March 2017) Dr. Lisa Kim Nguyen Pachychoroid (September 2016, December 2016, June 2017) Toxic optic neuropathy (September 2016, January 2017) Low Vision Overview (December 2016) Neuromyelitis Optica (May 2017) Dr. Shelley Phoun Choroidal metastasis (September 2016, December 2016, March 2017) Keeping up with Keratoconus (March 2017) Paracentral acute middle maculopathy (May 2017, June 2017) 2015-2016 Dr.Christine Chien Retinal astrocytic hamartoma (August 2015, November 2015, March 2016, May 2016, June 2016) Thygeson’s SPK (February 2016) Neuro-optometry case presentation (March 2016) 08.18 Dr. Charles Lee Optic nerve melanocytoma (August 2015, November 2015, March 2016, May 2016, June 2016) Homonymous hemianopsia secondary to recent stroke (December 2015) Vitelliform lesions (December 2015) Dr. -
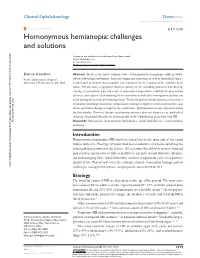
Homonymous Hemianopia Open Access to Scientific and Medical Research DOI
Journal name: Clinical Ophthalmology Article Designation: Review Year: 2014 Volume: 8 Clinical Ophthalmology Dovepress Running head verso: Goodwin Running head recto: Homonymous hemianopia open access to scientific and medical research DOI: http://dx.doi.org/10.2147/OPTH.S59452 Open Access Full Text Article REVIEW Homonymous hemianopia: challenges and solutions Denise Goodwin Abstract: Stroke is the most common cause of homonymous hemianopia (HH) in adults, Pacific University College of followed by trauma and tumors. Associated signs and symptoms, as well as visual field charac- Optometry, Forest Grove, OR, USA teristics such as location and congruity, can help determine the location of the causative brain lesion. HH can have a significant effect on quality of life, including problems with driving, reading, or navigation. This can result in decreased independence, inability to enjoy leisure activities, and injuries. Understanding these restrictions, as well as the management options, can aid in making the best use of remaining vision. Treatment options include prismatic correction to expand the remaining visual field, compensatory training to improve visual search abilities, and vision restoration therapy to improve the vision itself. Spontaneous recovery can occur within the first months. However, because spontaneous recovery does not always occur, methods of reducing visual disability play an important role in the rehabilitation of patients with HH. For personal use only. Keywords: hemianopia, homonymous hemianopia, visual field defects, visual training, perimetry Introduction Homonymous hemianopia (HH) involves vision loss on the same side of the visual field in both eyes. This type of visual field loss is indicative of a lesion involving the visual pathway posterior to the chiasm. -

Clinical Consequences of Stroke
EBRSR [Evidence-Based Review of Stroke Rehabilitation] 2 Clinical Consequences of Stroke Robert Teasell MD, Norhayati Hussein MBBS Last updated: March 2018 Abstract Cerebrovascular disorders represent the third leading cause of mortality and the second major cause of long-term disability in North America (Delaney and Potter 1993). The impairments associated with a stroke exhibit a wide diversity of clinical signs and symptoms. Disability, which is multifactorial in its determination, varies according to the degree of neurological recovery, the site of the lesion, the patient's premorbid status and the environmental support systems. Clinical evidence is reviewed as it pertains to stroke lesion location (cerebral, right & left hemispheres; lacunar and brain stem), related disorders (emotional, visual spatial perceptual, communication, fatigue, etc.) and artery(s) affected. 2. Clinical Consequences of Stroke pg. 1 of 29 www.ebrsr.com Table of Contents Abstract .............................................................................................................................................1 Table of Contents ...............................................................................................................................2 Introduction ......................................................................................................................................3 2.1 Localization of the Stroke ...........................................................................................................3 2.2 Cerebral -

Residents Weekend Case Report-Anaheim 2016 Amy Puerto, O.D
Residents Weekend Case Report-Anaheim 2016 Amy Puerto, O.D. School Affiliation: Southern College of Optometry- Family Practice Residency Name/Location: Bond Wroten Eye Clinic, Denham Springs, Louisiana TITLE: For Crying Out Loud! Unilateral Epiphora Reveals Unexpected Macular Hole and Pituitary Tumor ABSTRACT: A 68 year old male presented with excessive tearing and blurred vision in the left eye. Confrontational visual fields and dilated fundus exam revealed both homonymous inferior hemianopsia and macular hole. Neuroimaging confirmed pituitary adenoma. I. Case History A 68 year old Caucasian male presented for a comprehensive eye exam stating his left eye was constantly watering. The patient reported a history of punctal irrigation and dilation in the left eye. Interestingly the patient also complained of blurred vision in the left eye, like looking through water, and blinking more frequently over the past five months to help focus vision in the left eye. The patient’s last eye exam was five year ago. The patient reported symptoms began soon after he had a sinus cold. The patient used +2.00 OTC readers and took Refresh Optive lubricating artificial tears two-three times per day but was not on any systemic medications. He denied any previous eye trauma or eye surgery. He reported no medication allergies. The patient denied pain and was alert and oriented to time and place during the eye exam. II. Pertinent findings Entering uncorrected visual acuities were 20/30- OD and 20/70 OS at distance and 20/40 OU at near. Manifest Refraction revealed little improvement with +1.00 - 1.25 x 085 OD and – 0.25 – 1.25 x 085 OS and VA’s 20/30- and 20/60-, respectfully.