Preseptal and Orbital Cellulitis UHL Childrens Hospital Guideline
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Differentiate Red Eye Disorders
Introduction DIFFERENTIATE RED EYE DISORDERS • Needs immediate treatment • Needs treatment within a few days • Does not require treatment Introduction SUBJECTIVE EYE COMPLAINTS • Decreased vision • Pain • Redness Characterize the complaint through history and exam. Introduction TYPES OF RED EYE DISORDERS • Mechanical trauma • Chemical trauma • Inflammation/infection Introduction ETIOLOGIES OF RED EYE 1. Chemical injury 2. Angle-closure glaucoma 3. Ocular foreign body 4. Corneal abrasion 5. Uveitis 6. Conjunctivitis 7. Ocular surface disease 8. Subconjunctival hemorrhage Evaluation RED EYE: POSSIBLE CAUSES • Trauma • Chemicals • Infection • Allergy • Systemic conditions Evaluation RED EYE: CAUSE AND EFFECT Symptom Cause Itching Allergy Burning Lid disorders, dry eye Foreign body sensation Foreign body, corneal abrasion Localized lid tenderness Hordeolum, chalazion Evaluation RED EYE: CAUSE AND EFFECT (Continued) Symptom Cause Deep, intense pain Corneal abrasions, scleritis, iritis, acute glaucoma, sinusitis, etc. Photophobia Corneal abrasions, iritis, acute glaucoma Halo vision Corneal edema (acute glaucoma, uveitis) Evaluation Equipment needed to evaluate red eye Evaluation Refer red eye with vision loss to ophthalmologist for evaluation Evaluation RED EYE DISORDERS: AN ANATOMIC APPROACH • Face • Adnexa – Orbital area – Lids – Ocular movements • Globe – Conjunctiva, sclera – Anterior chamber (using slit lamp if possible) – Intraocular pressure Disorders of the Ocular Adnexa Disorders of the Ocular Adnexa Hordeolum Disorders of the Ocular -

A Description of the Clinical Features of Brimonidine- Associated Uveitis Alyssa Louie Primary Care Resident, San Francisco VA
Drug-induced intraocular inflammation: A description of the clinical features of brimonidine- associated uveitis Alyssa Louie Primary Care Resident, San Francisco VA Abstract: A description of the clinical features, diagnostic work-up, and management of acute anterior uveitis caused by brimonidine, a widely used glaucoma medication. I. Case History a. Patient demographics: 74 year-old white male b. Chief complaint: eye pain, redness, irritation for last 2 weeks c. Ocular and medical history: i. Ocular history 1. Primary open angle glaucoma OU, diagnosed 8 years ago 2. Senile cataracts OU, not visually significant 3. Type 2 Diabetes without retinopathy OU 4. No prior history of uveitis ii. Medical history: Diabetes Mellitus Type 2 iii. No known drug allergies d. Medications i. Ocular: dorzolamide BID OU (1.5 years), brimonidine BID OU (11 months), travatan QHS OU (5.5 years) ii. Medical: metformin 500mg tab BID PO II. Pertinent Findings a. Clinical exam i. Visual acuities: OD 20/20-, OS 20/20- ii. Goldmann applanation tonometry: 13 mm Hg OD, 13 mm Hg OS iii. Anterior segment 1. OU: 3+ diffuse conjunctival injection 2. OU: central and inferior granulomatous keratic precipitates 3. OU: Grade 1+ cell, 1+ flare 4. OU: No synechiae or iris changes were present iv. Posterior segment 1. Optic Nerve a. OD: Cup-to-disc ratio 0.70H/V, distinct margins b. OS: Cup-to-disc ratio 0.75H/V, distinct margins 2. Posterior pole, periphery, vitreous: unremarkable OU b. Laboratory Studies i. ACE, Lysozyme, FTA-ABS, VDRL, HLA-B27, Rheumatoid Factor, ANA, PPD, Chest X- ray: all negative/unreactive III. -

MRSA Ophthalmic Infection, Part 2: Focus on Orbital Cellulitis
Clinical Update COMPREHENSIVE MRSA Ophthalmic Infection, Part 2: Focus on Orbital Cellulitis by gabrielle weiner, contributing writer interviewing preston h. blomquist, md, vikram d. durairaj, md, and david g. hwang, md rbital cellulitis is a poten- Acute MRSA Cellulitis tially sight- and life-threat- ening disease that tops the 1A 1B ophthalmology worry list. Add methicillin-resistant OStaphylococcus aureus (MRSA) to the mix of potential causative bacteria, and the level of concern rises even higher. MRSA has become a relatively prevalent cause of ophthalmic infec- tions; for example, one study showed that 89 percent of preseptal cellulitis S. aureus isolates are MRSA.1 And (1A) This 19-month-old boy presented with left periorbital edema and erythema preseptal cellulitis can rapidly develop five days after having been diagnosed in an ER with conjunctivitis and treated into the more worrisome condition of with oral and topical antibiotics. (1B) Axial CT image of the orbits with contrast orbital cellulitis if not treated promptly shows lacrimal gland abscess and globe displacement. and effectively. Moreover, the community-associ- and Hospital System in Dallas, 86 per- When to Suspect ated form of MRSA (CA-MRSA) now cent of those with preseptal cellulitis MRSA Orbital Cellulitis accounts for a larger proportion of and/or lid abscesses had CA-MRSA. Patients with orbital cellulitis com- ophthalmic cases than health care– These studies also found that preseptal monly complain of pain when moving associated MRSA (HA-MRSA). Thus, cellulitis was the most common oph- the eye, decreased vision, and limited many patients do not have the risk fac- thalmic MRSA presentation from 2000 eye movement. -

Chronic Conjunctivitis
9/8/2017 Allergan Pharmaceuticals Speaker’s Bureau Bio-Tissue BioDLogics, LLC Katena/IOP Seed Biotech COA Monterey Symposium 2017 Johnson and Johnson Vision Care, Inc. Shire Pharmaceuticals Nicholas Colatrella, OD, FAAO, Dipl AAO, ABO, ABCMO Jeffrey R. Varanelli, OD, FAAO, Dipl ABO, ABCMO Text NICHOLASCOLA090 to 22333 to join Live Text Poll Nicholas Colatrella, OD, FAAO, Dipl AAO, Jeffrey Varanelli, OD, FAAO, Dipl ABO, ABO, ABCMO ABCMO Text NICHOLASCOLA090 to 22333 once to join Then text A, B, C, D, E or write in your answer Live Immediate Accurate Chronic conjunctivitis is one of the most frustrating reasons that patients present to the office (1) Time course Often times patients will seek multiple providers searching for a solution The chronicity of their symptoms is extremely frustrating to the (2) Morphology patient and treating physician alike Some conditions can seriously affect vision and create ocular morbidity (3) Localization of disease process Many of these diseases do not respond to commonly used topical antibiotics, topical steroids, artificial tears, and other treatments for external ocular disease (4) Type of discharge or exudate Our hope during this one-hour lecture is to present a process to help aid in the diagnosis of chronic conjunctivitis help you determine the most likely etiology 1 9/8/2017 Three weeks is the dividing point as it is the upper limit for cases of viral infection and most bacterial infections to resolve without treatment. Acute Conjunctivitis Conjunctivitis that has been present for less than 3 weeks -

Oral Contraception and Eye Disease: findings in Two Large Cohort Studies
538 Br J Ophthalmol 1998;82:538–542 Oral contraception and eye disease: findings in two large cohort studies M P Vessey, P Hannaford, J Mant, R Painter, P Frith, D Chappel Abstract over.4 Given the sparsity of the epidemiological Aim—To investigate the relation between evidence available, we have undertaken an oral contraceptive use and certain eye dis- analysis of the data on eye disease in the two eases. large British cohort studies of the benefits and Methods—Abstraction of the relevant data risks of oral contraception—namely, the Royal from the two large British cohort studies College of General Practitioners’ (RCGP) Oral of the eVects of oral contraception, the Contraception Study5 and the Oxford-Family Royal College of General Practitioners’ Planning Association (Oxford-FPA) contra- (RCGP) Oral Contraception Study and ceptive study.6 We summarise our findings the Oxford-Family Planning Association here. (Oxford-FPA) Contraceptive Study. Both cohort studies commenced in 1968 and were organised on a national basis. Be- Material and methods tween them they have accumulated over ROYAL COLLEGE OF GENERAL PRACTITIONERS’ 850 000 person years of observation in- ORAL CONTRACEPTION STUDY volving 63 000 women. During a 14 month period beginning in May 1968, 1400 British general practitioners re- Results—The conditions considered in the analysis were conjunctivitis, keratitis, iri- cruited 23 000 women using oral contracep- tives and a similar number who had never done tis, lacrimal disease, strabismus, cataract, 5 glaucoma, retinal detachment, and retinal so. The two groups were of similar age and all vascular lesions. With the exception of subjects were married or living as married. -

Ophthalmology Ophthalomolgy
Ophthalmology Ophthalomolgy Description ICD10-CM Documentation Tips Description ICD10-CM Documentation Tips Cataracts Code Tip Glaucoma Code Tip Cortical age-related cataract, right eye H25.011 Right, left, or bilateral; Presenile, Open angle with borderline H40.011 Suspect, Open angle, Primary senile, traumatic, complicated; findings, low risk, right eye angle closure; type; acute vs., specific type (cortical, anterior or chronic; mild, moderate, severe, Cortical age-related cataract, left eye H25.012 Open angle with borderline H40.012 posterior subcapsular polar, etc) indeterminate findings, low risk, left eye Cortical age-related cataract, bilateral eye H25.013 Open angle with borderline H40.013 findings, low risk, bilateral eye Anterior subcapsular polar age-related H25.031 Anatomical narrow angle, right H40.031 cataract,right eye eye Anterior subcapsular polar age-related H25.032 Anatomical narrow angle, right H40.032 cataract, left eye eye Anterior subcapsular polar age-related H25.033 Anatomical narrow angle, H40.033 cataract, bilateral bilateral Age-related nuclear cataract, right eye H25.11 Primary open-angle H40.11x2 glaucoma, moderate stage Age-related nuclear cataract, left eye H25.12 Globe Rupture Code Tip Age-related nuclear cataract, bilateral eye H25.13 Penetrating wound without S05.62xS Contusion vs. laceration; If foreign body of left eyeball, laceration, with or without sequela prolapsed or loss of intraocular tissue; penetrating wound, with or Combined forms of age-related cataract, H25.811 Contusion of eyeball and -

Treatment of Peripheral Corneal Ulcers by Limbal Conjunctivectomy
Brit. 7. Ophthal. (I 976) 6o, 713 Br J Ophthalmol: first published as 10.1136/bjo.60.10.713 on 1 October 1976. Downloaded from Treatment of peripheral corneal ulcers by limbal conjunctivectomy FRED M. WILSON II, MERRILL GRAYSON, AND FORREST D. ELLIS From the Department of Ophthalmology, Indiana University School of Medicine, Indianapolis, Indiana Peripheral corneal ulcers can still pose difficult appear within the ulcer about one week later, followed clinical problems despite therapeutic advances such in a few days by superficial vascularization. The ulcer as specific antimicrobial agents, collagenase inhibi- had healed and epithelialized three weeks after surgery tors, heparin, ocular lubricants, biological adhe- (Fig. ib) and L-cysteine and heparin drops were con- sives, and soft contact lenses. This paper reports tinued for three weeks after it had healed. The ulcer has the healing of several types of progressive marginal ulcers after the excision and recession of adjacent limbal conjunctiva (limbal conjunctivectomy), in some cases after other modes of treatment had been unsuccessful. copyright. Case reports CASE I, MOOREN )S ULCER A 54-year-old Black woman developed a severely painful, largely non-infiltrative ulcer of the nasal left cornea. The ulcer had an overhanging central edge and progressed circumferentially during a period of one year to involve nearly the entire comeal periphery http://bjo.bmj.com/ (Fig. ia). Progression occurred despite treatment at various times with acetylcysteine drops, L-cysteine drops, topical and subconjunctival heparin, artificial soft contact a short trial of tears, lens, topical cortico- (Ia.) steroids, and a trial without any treatment to minimize the possibility of overtreatment. -

The Definition and Classification of Dry Eye Disease
DEWS Definition and Classification The Definition and Classification of Dry Eye Disease: Report of the Definition and Classification Subcommittee of the International Dry E y e W ork Shop (2 0 0 7 ) ABSTRACT The aim of the DEWS Definition and Classifica- I. INTRODUCTION tion Subcommittee was to provide a contemporary definition he Definition and Classification Subcommittee of dry eye disease, supported within a comprehensive clas- reviewed previous definitions and classification sification framework. A new definition of dry eye was devel- T schemes for dry eye, as well as the current clinical oped to reflect current understanding of the disease, and the and basic science literature that has increased and clarified committee recommended a three-part classification system. knowledge of the factors that characteriz e and contribute to The first part is etiopathogenic and illustrates the multiple dry eye. Based on its findings, the Subcommittee presents causes of dry eye. The second is mechanistic and shows how herein an updated definition of dry eye and classifications each cause of dry eye may act through a common pathway. based on etiology, mechanisms, and severity of disease. It is stressed that any form of dry eye can interact with and exacerbate other forms of dry eye, as part of a vicious circle. II. GOALS OF THE DEFINITION AND Finally, a scheme is presented, based on the severity of the CLASSIFICATION SUBCOMMITTEE dry eye disease, which is expected to provide a rational basis The goals of the DEWS Definition and Classification for therapy. These guidelines are not intended to override the Subcommittee were to develop a contemporary definition of clinical assessment and judgment of an expert clinician in dry eye disease and to develop a three-part classification of individual cases, but they should prove helpful in the conduct dry eye, based on etiology, mechanisms, and disease stage. -
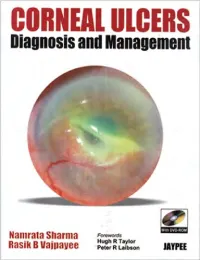
CORNEAL ULCERS Diagnosis and Management
CORNEAL ULCERS Diagnosis and Management System requirement: • Windows XP or above • Power DVD player (Software) • Windows Media Player 10.0 version or above • Quick time player version 6.5 or above Accompanying DVD ROM is playable only in Computer and not in DVD player. Kindly wait for few seconds for DVD to autorun. If it does not autorun then please do the following: • Click on my computer • Click the drive labelled JAYPEE and after opening the drive, kindly double click the file Jaypee CORNEAL ULCERS Diagnosis and Management Namrata Sharma MD DNB MNAMS Associate Professor of Ophthalmology Cornea, Cataract and Refractive Surgery Services Dr. Rajendra Prasad Centre for Ophthalmic Sciences All India Institute of Medical Sciences, New Delhi India Rasik B Vajpayee MS FRCSEd FRANZCO Head, Corneal and Cataract Surgery Centre for Eye Research Australia Royal Victorian Eye and Ear Hospital University of Melbourne Australia Forewords Hugh R Taylor Peter R Laibson ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD New Delhi • Ahmedabad • Bengaluru • Chennai • Hyderabad • Kochi • Kolkata • Lucknow • Mumbai • Nagpur Published by Jitendar P Vij Jaypee Brothers Medical Publishers (P) Ltd B-3 EMCA House, 23/23B Ansari Road, Daryaganj New Delhi 110 002, India Phones: +91-11-23272143, +91-11-23272703, +91-11-23282021, +91-11-23245672 Rel: +91-11-32558559, Fax: +91-11-23276490, +91-11-23245683 e-mail: [email protected] Visit our website: www.jaypeebrothers.com Branches • 2/B, Akruti Society, Jodhpur Gam Road Satellite Ahmedabad 380 015, Phones: +91-79-26926233, -

Nasolacrimal Duct Obstruction Review
Mini Review JOJ Ophthal Volume 3 Issue 4 - July 2017 Copyright © All rights are reserved by Velasco Y Levy Adriana DOI: 10.19080/JOJO.2017.03.555619 Nasolacrimal Duct Obstruction Review Nava Castañeda Angel1 and Velasco Y Levy Adriana2* 1lacrimal Surgeon, Ophthalmology Institute, Mexico 2lacrimal system resident, Ophthalmology Institute, Mexico Submission: February 14, 2017; Published: July 06, 2017 *Corresponding author: Velasco Y Levy Adriana, Ophthalmologist, orbit, oculoplastic and lacrimal system resident. “Conde de Valenciana I.A.P”. Ophthalmology Institute, Chimampopoca 14, Col Obrera, Mexico, Tel: ; Email: Abstract surgery,Anatomical trauma obstructionor scarring, andrefers infection to any structural must be obtained pathology for in determine the lacrimal the outflow etiology pathway and the whichpossible hinders nasolacrimal tear drainage1. pathway It blocking can be congenital site. This or acquired. It is mostly presented in infants under 2 years old and in adults over 50. A detailed history of any systemic or topical medication, isKeywords: a short review about the congenital and acquired forms, how it is diagnosed and its main features. Congenital lacrimal obstruction; Acquired lacrimal obstruction; Acute dacryocistitis; Chronic dacryocistitis Introduction malposition, position of the punctum in the tear lake, and any The lacrimal system comprises two components the main sign of previous surgery. The Schirmer test [6], tear break up and accessory lacrimal glands and their secretions and the time [7], ocular surface staining, and tear meniscus height will lacrimal excretory system [1]. The lacrimal excretory system rule out any associated ocular surface abnormalities. Abnormal is divided into the proximal and distal sections. The proximal dye disappearance test is a very maneuver to assess abnormal section includes the punctum, canaliculus, and the common tear drainage system and is especially helpful in pediatric canaliculus [2,3]. -

Corneal Ulcers: for the General Practitioner
Corneal ulcers: For the general practitioner A corneal ulcer is a defect in the epithelial layer of the cornea. e general practitioner may play an important role in early management and appropriate referral. Incidence varies and depends on aetiology. S Ballim, MB ChB, Dip Ophth (SA), FC Ophth (SA) Department of Ophthalmology, University of KwaZulu-Natal, Durban, South Africa Correspondence to: S Ballim ([email protected]) Basic clinical assessment of the cornea clue as to the health of the posterior segment of the eye. Compare History ndings with the fellow eye. Presenting complaints include pain, irritation, decreased vision or foreign-body sensation. Ask about any history of trauma, including Fluorescein dye should be instilled. Any epithelial defects will stain nature of injury, the timing and the relationship to drop in vision. green. e stain shows up best under blue light (present on some Specic enquiry as to instillation of medication (e.g. steroid drops) ophthalmoscopes). is can, however, be adequately demonstrated or home remedies (e.g. breast milk or urine) is important, as these with a standard torch. e tear lm will become apparent and the may be important predisposing factors and give clues as to the lacus lacrimalis can be assessed. Dry eye is a very signicant factor aetiology. Contact lens use is a very common cause of corneal ulcers. in many corneal epithelial disorders. Tools for examination In general practice it is presumed that a slit-lamp and other specialised equipment is unavailable. It would be reasonable to have Topical antibiotics have been the following ophthalmic tools at one’s disposal: shown to have action against both • visual acuity chart bacterial and fungal pathogens • uorescein strips • topical anaesthetic eye drops and are suitable for preventing • direct ophthalmoscope. -

Atopic Keratoconjunctivitis
Atopic Keratoconjunctivitis Fahd Anzaar, MD, C. Stephen Foster, MD, FACS, FACR A 31 year old male patient presented to us, referred from an ophthalmologist in New York, with a diagnosis of ‘recent corneal tear in the right eye’. The patient complained of persistent ‘soreness’, excessive tearing, and photophobia. He had had these complaints intermittently, alongwith yellowish mucous discharge (especially upon awakening) for many years and many eye drops and oral medications had been prescribed by many ophthalmologists and dermatologists over the years. This particular episode was severe and unremitting, and hence the referral. The patient’s past medical history was significant for atopic dermatitis (AD or eczema) and exercise-induced asthma. The family history was significant for myocardial infarction in his father, and cancer, specifically colorectal cancer, and the patient’s mother had ovarian cancer. The patient was a non-smoker, was a student working part time as a waiter, and occasionally drank alcohol. At presentation, his medications included systemic prednisone (60 mg daily), topically applied (skin) tacrolimus cream and triamcinolone. He was also using Lotemax, Alrex and Vigamox eye drops in the right eye four times daily, Restasis in the left eye twice daily, and Celluvisc in both eyes as needed. He was allergic to Dovonex cream, and had a history of intolerance to systemic cyclosporine (hypertension and nephropathy). General physical examination disclosed eczema of the face and chest. Visual acuities were 20/200 OD and hand motion OS, intraocular pressures were 12 and 15, and slit lamp biomicroscopy showed 3+ conjunctival injection in the right eye, with ciliary flushing, and a corneal epithelial defect with stromal opacification, glue, and bilateral keratoconus.