Type of the Paper (Article
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Endo4 PRINT.Indb
Contents 1 Tumours of the pituitary gland 11 Spindle epithelial tumour with thymus-like differentiation 123 WHO classifi cation of tumours of the pituitary 12 Intrathyroid thymic carcinoma 125 Introduction 13 Paraganglioma and mesenchymal / stromal tumours 127 Pituitary adenoma 14 Paraganglioma 127 Somatotroph adenoma 19 Peripheral nerve sheath tumours 128 Lactotroph adenoma 24 Benign vascular tumours 129 Thyrotroph adenoma 28 Angiosarcoma 129 Corticotroph adenoma 30 Smooth muscle tumours 132 Gonadotroph adenoma 34 Solitary fi brous tumour 133 Null cell adenoma 37 Haematolymphoid tumours 135 Plurihormonal and double adenomas 39 Langerhans cell histiocytosis 135 Pituitary carcinoma 41 Rosai–Dorfman disease 136 Pituitary blastoma 45 Follicular dendritic cell sarcoma 136 Craniopharyngioma 46 Primary thyroid lymphoma 137 Neuronal and paraneuronal tumours 48 Germ cell tumours 139 Gangliocytoma and mixed gangliocytoma–adenoma 48 Secondary tumours 142 Neurocytoma 49 Paraganglioma 50 3 Tumours of the parathyroid glands 145 Neuroblastoma 51 WHO classifi cation of tumours of the parathyroid glands 146 Tumours of the posterior pituitary 52 TNM staging of tumours of the parathyroid glands 146 Mesenchymal and stromal tumours 55 Parathyroid carcinoma 147 Meningioma 55 Parathyroid adenoma 153 Schwannoma 56 Secondary, mesenchymal and other tumours 159 Chordoma 57 Haemangiopericytoma / Solitary fi brous tumour 58 4 Tumours of the adrenal cortex 161 Haematolymphoid tumours 60 WHO classifi cation of tumours of the adrenal cortex 162 Germ cell tumours 61 TNM classifi -
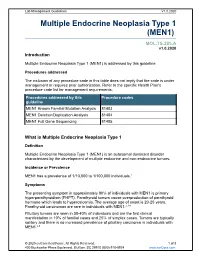
Multiple Endocrine Neoplasia Type 1 (MEN1)
Lab Management Guidelines V1.0.2020 Multiple Endocrine Neoplasia Type 1 (MEN1) MOL.TS.285.A v1.0.2020 Introduction Multiple Endocrine Neoplasia Type 1 (MEN1) is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline MEN1 Known Familial Mutation Analysis 81403 MEN1 Deletion/Duplication Analysis 81404 MEN1 Full Gene Sequencing 81405 What is Multiple Endocrine Neoplasia Type 1 Definition Multiple Endocrine Neoplasia Type 1 (MEN1) is an autosomal dominant disorder characterized by the development of multiple endocrine and non-endrocrine tumors. Incidence or Prevalence MEN1 has a prevalence of 1/10,000 to 1/100,000 individuals.1 Symptoms The presenting symptom in approximately 90% of individuals with MEN1 is primary hyperparathyroidism (PHPT). Parathyroid tumors cause overproduction of parathyroid hormone which leads to hypercalcemia. The average age of onset is 20-25 years. Parathyroid carcinomas are rare in individuals with MEN1.2,3,4 Pituitary tumors are seen in 30-40% of individuals and are the first clinical manifestation in 10% of familial cases and 25% of simplex cases. Tumors are typically solitary and there is no increased prevalence of pituitary carcinoma in individuals with MEN1.2,5 © 2020 eviCore healthcare. All Rights Reserved. 1 of 8 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2020 Prolactinomas are the most commonly seen pituitary subtype and account for 60% of pituitary adenomas. -

Familial Adenomatous Polyposis Polymnia Galiatsatos, M.D., F.R.C.P.(C),1 and William D
American Journal of Gastroenterology ISSN 0002-9270 C 2006 by Am. Coll. of Gastroenterology doi: 10.1111/j.1572-0241.2006.00375.x Published by Blackwell Publishing CME Familial Adenomatous Polyposis Polymnia Galiatsatos, M.D., F.R.C.P.(C),1 and William D. Foulkes, M.B., Ph.D.2 1Division of Gastroenterology, Department of Medicine, The Sir Mortimer B. Davis Jewish General Hospital, McGill University, Montreal, Quebec, Canada, and 2Program in Cancer Genetics, Departments of Oncology and Human Genetics, McGill University, Montreal, Quebec, Canada Familial adenomatous polyposis (FAP) is an autosomal-dominant colorectal cancer syndrome, caused by a germline mutation in the adenomatous polyposis coli (APC) gene, on chromosome 5q21. It is characterized by hundreds of adenomatous colorectal polyps, with an almost inevitable progression to colorectal cancer at an average age of 35 to 40 yr. Associated features include upper gastrointestinal tract polyps, congenital hypertrophy of the retinal pigment epithelium, desmoid tumors, and other extracolonic malignancies. Gardner syndrome is more of a historical subdivision of FAP, characterized by osteomas, dental anomalies, epidermal cysts, and soft tissue tumors. Other specified variants include Turcot syndrome (associated with central nervous system malignancies) and hereditary desmoid disease. Several genotype–phenotype correlations have been observed. Attenuated FAP is a phenotypically distinct entity, presenting with fewer than 100 adenomas. Multiple colorectal adenomas can also be caused by mutations in the human MutY homologue (MYH) gene, in an autosomal recessive condition referred to as MYH associated polyposis (MAP). Endoscopic screening of FAP probands and relatives is advocated as early as the ages of 10–12 yr, with the objective of reducing the occurrence of colorectal cancer. -

Ganglioneuroblastoma As Vasoactive Intestinal Polypeptide-Secreting10.5005/Jp-Journals-10002-1167 Tumor: Rare Case Report in a Child Case Report
WJOES Ganglioneuroblastoma as Vasoactive Intestinal Polypeptide-secreting10.5005/jp-journals-10002-1167 Tumor: Rare Case Report in a Child CASE REPORT Ganglioneuroblastoma as Vasoactive Intestinal Polypeptide-secreting Tumor: Rare Case Report in a Child 1Basant Kumar, 2Vijai D Upadhyaya, 3Ram Nawal Rao, 4Sheo Kumar ABSTRACT than 60 cases of pediatric VIP-secreting tumors.3 Most Pathologically elevated vasoactive intestinal polypeptide (VIP) of them are either adrenal pheochromocytoma or mixed plasma levels cause secretory diarrhea with excessive loss of pheochromocytoma-ganglioneuroma tumors. Mason water and electrolyte and is characterized by the typical symp- et al,4 first described the secretory nature of neuroblas- toms of hypokalemia and metabolic acidosis. It rarely occurs toma and vasoactive intestinal peptide (VIP) can be in patients with non-pancreatic disease. Despite the clinical severity, diagnosis of a VIP-secreting tumor is often delayed. produced by the mature neurogenic tumors. We herein We herein present a 14-month-old boy having prolonged present a 14 months old boy having prolonged therapy- therapy-resistant secretory diarrhea, persistent hypokalemia resistant secretory diarrhea, persistent hypokalemia with with tissue diagnosis of ganglioneuroblastoma and raised plasma VIP-levels. tissue diagnosis of ganglioneuroblastoma and briefly review the literature. Keywords: Ganglioneuroblastoma, Secretory diarrhea, VIPoma. CASE REPORT How to cite this article: Kumar B, Upadhyaya VD, Rao RN, Kumar S. Ganglioneuroblastoma as Vasoactive Intestinal A 14-month-old boy, weighing 9 kg with advanced symp- Polypeptide-secreting Tumor: Rare Case Report in a Child. World J Endoc Surg 2015;7(2):47-50. toms of persistent secretory diarrhea, hypokalemia and metabolic acidosis was referred to us with radiological Source of support: Nil (computed tomography) diagnosis of retroperitoneal Conflict of interest: None mass. -

Familial Adenomatous Polyposis and MUTYH-Associated Polyposis
Corporate Medical Policy Familial Adenomatous Polyposis and MUTYH-Associated Polyposis AHS-M2024 File Name: familial_adenomatous_polyposis_and_mutyh_associated_polyposis Origination: 1/1/2019 Last CAP Review: 8/2021 Next CAP Review: 8/2022 Last Review: 8/2021 Description of Procedure or Service Familial adenomatous polyposis (FAP) is characterized by development of adenomatous polyps and an increased risk of colorectal cancer (CRC) caused by an autosomal dominant mutation in the APC (Adenomatous Polyposis Coli) gene (Kinzler & Vogelstein, 1996). Depending on the location of the mutation in the APC gene FAP can present as the more severe classic FAP (CFAP) with hundreds to thousands of polyps developing in the teenage years associated with a significantly increased risk of CRC, or attenuated FAP (AFAP) with fewer polyps, developing later in life and less risk of CRC (Brosens, Offerhaus, & Giardiello 2015; Spirio et al., 1993). Two other subtypes of FAP include Gardner syndrome, which causes non-cancer tumors of the skin, soft tissues, and bones, and Turcot syndrome, a rare inherited condition in which individuals have a higher risk of adenomatous polyps and colorectal cancer. In classic FAP, the most common type, patients usually develop cancer in one or more polyps as early as age 20, and almost all classic FAP patients have CRC by the age of 40 if their colon has not been removed (American_Cancer_Society, 2020). MUTYH-associated polyposis (MAP) results from an autosomal recessive mutation of both alleles of the MUTYH gene and is characterized by increased risk of CRC with development of adenomatous polyps. This condition, however, may present without these characteristic polyps (M. -

Neuroendocrine Tumors of the Pancreas (Including Insulinoma, Gastrinoma, Glucogacoma, Vipoma, Somatostatinoma)
Neuroendocrine tumors of the pancreas (including insulinoma, gastrinoma, glucogacoma, VIPoma, somatostatinoma) Neuroendocrine pancreatic tumors (pancreatic NETs or pNETs) account for about 3% of all primary pancreatic tumors. They develop in neuroendocrine cells called islet cells. Neuroendocrine tumors of the pancreas may be nonfunctional (not producing hormones) or functional (producing hormones). Most pNETs do not produce hormones and, as a result, these tumors are diagnosed incidentally or after their growth causes symptoms such as abdominal pain, jaundice or liver metastasis. pNETs that produce hormones are named according to the type of hormone they produce and / or clinical manifestation: Insulinoma - An endocrine tumor originating from pancreatic beta cells that secrete insulin. Increased insulin levels in the blood cause low glucose levels in blood (hypoglycemia) with symptoms that may include sweating, palpitations, tremor, paleness, and later unconsciousness if treatment is delayed. These are usually benign and tend to be small and difficult to localize. Gastrinoma - a tumor that secretes a hormone called gastrin, which causes excess of acid secretion in the stomach. As a result, severe ulcerative disease and diarrhea may develop. Most gastrinomas develop in parts of the digestive tract that includes the duodenum and the pancreas, called "gastrinoma triangle". These tumors have the potential to be malignant. Glucagonoma is a rare tumor that secretes the hormone glucagon, which may cause a typical skin rash called migratory necrolytic erythema, elevated glucose levels, weight loss, diarrhea and thrombotic events. VIPoma - a tumor that secretes Vasoactive peptide (VIP) hormone causing severe diarrhea. The diagnosis is made by finding a pancreatic neuroendocrine tumor with elevated VIP hormone in the blood and typical clinical symptoms. -

Surgical Management of Ampullary Somatostatinoma
JOP. J Pancreas (Online) 2016 Jul 08; 17(4):406-409. CASE SERIES Surgical Management of Ampullary Somatostatinoma Nicholas Phillips, Terence Huey, Joel Lewin, Anthony W Cheng, Nicholas A O’Rourke Hepato-Pancreato-Biliary Unit, Department of General Surgery, Royal Brisbane Hospital, Brisbane, Australia ABSTRACT Introduction Somatostatinomas of the ampulla are rare neuroendocrine tumours with limited studies in the literature. These are often associated with familial genetic predisposition e.g. NF 1 and Von Hippel-Lindau Syndrome. Histology commonly shows classical features such as Psammoma bodies. The classical presentation with inhibitory syndrome is rare, but ampullary mass effects can cause an earlier presentation with potentially better outcomes with earlier intervention and treatment. Case series We report three cases of ampullary the second with recurrent pancreatitis and the third, with elevated CA19-9 levels. Various preoperative localisation techniques were employedsomatostatisnomas: and one had one an sporadic attempted and endoscopic two familial, resection associated yielding with involved neurofibromatosis margins. All type patients 1. The underwent first patient pancreaticoduodenectomy, presented with pruritus, of which one was laparoscopic assisted. The median size of the tumour was 10 mm and one patient had nodal involvement. All 3 patients have remained disease free at most recent follow up ranging from 1.5 to 11 years. Discussion Ampullary somatostatinomas can present early with mass related effects while inhibitory syndrome is rare. Early detection and intervention in ampullary somatostatinoma may contribute to better outcomes than pancreatic somatostatinomas. Long-term survival is achievable through pancreaticoduodenectomy for resectable ampullary somatostatinoma and laparoscopic approach is a feasible and viable option. INTRODUCTION cases of ampullary somatostatinoma that were treated by pancreaticoduodenectomy (PD) with good outcomes. -

Liver, Gallbladder, Bile Ducts, Pancreas
Liver, gallbladder, bile ducts, pancreas Coding issues Otto Visser May 2021 Anatomy Liver, gallbladder and the proximal bile ducts Incidence of liver cancer in Europe in 2018 males females Relative survival of liver cancer (2000 10% 15% 20% 25% 30% 35% 40% 45% 50% 0% 5% Bulgaria Latvia Estonia Czechia Slovakia Malta Denmark Croatia Lithuania N Ireland Slovenia Wales Poland England Norway Scotland Sweden Netherlands Finland Iceland Ireland Austria Portugal EUROPE - Germany 2007) Spain Switzerland France Belgium Italy five year one year Liver: topography • C22.1 = intrahepatic bile ducts • C22.0 = liver, NOS Liver: morphology • Hepatocellular carcinoma=HCC (8170; C22.0) • Intrahepatic cholangiocarcinoma=ICC (8160; C22.1) • Mixed HCC/ICC (8180; TNM: C22.1; ICD-O: C22.0) • Hepatoblastoma (8970; C22.0) • Malignant rhabdoid tumour (8963; (C22.0) • Sarcoma (C22.0) • Angiosarcoma (9120) • Epithelioid haemangioendothelioma (9133) • Embryonal sarcoma (8991)/rhabdomyosarcoma (8900-8920) Morphology*: distribution by sex (NL 2011-17) other other ICC 2% 3% 28% ICC 56% HCC 41% HCC 70% males females * Only pathologically confirmed cases Liver cancer: primary or metastatic? Be aware that other and unspecified morphologies are likely to be metastatic, unless there is evidence of the contrary. For example, primary neuro-endocrine tumours (including small cell carcinoma) of the liver are extremely rare. So, when you have a diagnosis of a carcinoid or small cell carcinoma in the liver, this is probably a metastatic tumour. Anatomy of the bile ducts Gallbladder -

Diagnostic Approach to Neuroendocrine Neoplasms of the Gastrointestinal Tract and Pancreas
Review doi: 10.5146/tjpath.2015.01319 Diagnostic Approach to Neuroendocrine Neoplasms of the Gastrointestinal Tract and Pancreas Silvia UCCELLA1, Fausto SESSA1, Stefano La ROSA2 1Department of Surgical and Morphological Sciences, University of Insubria, VARESE, ITALY, 2Department of Pathology, Ospedale di Circolo, VARESE, ITALY ABSTRACT The gastroenteropancreatic (GEP) system is the site of origin of about two thirds of all neuroendocrine neoplasms (NENs) of the human body. GEP-NENs encompass a wide spectrum of entities, from very indolent tumors to highly aggressive carcinomas. They represent a challenge for the oncologist and a correct diagnostic approach is crucial for the management of patients. The nomenclature and classification of these tumors have been a matter of debate for more than a century, since their first description by Siegfried Oberdorfer. The last WHO classification provided a robust and easy-to-use tool to prognostically stratify GEP-NENs, based on morphological aspects and on proliferation rate. This review examines current approaches to the diagnosis and prognostic classification of GEP-NENs, focusing on the critical use of morphological parameters and immunohistochemical stainings, including diagnostic, site-specific and prognostic markers. The key issues of the current classification are addressed, including the emerging topics about cases with discordant morphology and proliferative index. Finally, we attempted to highlight the diagnostic pitfalls and the caveats in the use of immunohistochemical stains. Key Words: Neuroendocrine tumors, Gastrointestinal tract, Pancreas, Diagnosis BACKGROUND finding, as only neoplasms widely metastatic to the liver are associated with this syndrome (3, 4). Neuroendocrine neoplasms (NENs) are a heterogeneous group of epithelial neoplastic proliferations arising in The high heterogeneity of the biological and clinical features a large number of body organs. -

Multiple Endocrine Neoplasia Type 1 (MEN1)
Lab Management Guidelines v2.0.2019 Multiple Endocrine Neoplasia Type 1 (MEN1) MOL.TS.285.A v2.0.2019 Introduction Multiple Endocrine Neoplasia Type 1 (MEN1) is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline MEN1 Known Familial Mutation Analysis 81403 MEN1 Deletion/Duplication Analysis 81404 MEN1 Full Gene Sequencing 81405 What is Multiple Endocrine Neoplasia Type 1 Definition Multiple Endocrine Neoplasia Type 1 (MEN1) is an inherited form of tumor predisposition characterized by multiple tumors of the endocrine system. Incidence or Prevalence MEN1 has a prevalence of 1/10,000 to 1/100,000 individuals.1 Symptoms The presenting symptom in 90% of individuals with MEN1 is primary hyperparathyroidism (PHPT). Parathyroid tumors cause overproduction of parathyroid hormone which leads to hypercalcemia. The average age of onset is 20-25 years. Parathyroid carcinomas are rare in individuals with MEN1.2,3,4 Pituitary tumors are seen in 30-40% of individuals and are the first clinical manifestation in 10% of familial cases and 25% of simplex cases. Tumors are typically solitary and there is no increased prevalence of pituitary carcinoma in individuals with MEN1.2,5 © eviCore healthcare. All Rights Reserved. 1 of 9 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines v2.0.2019 Prolactinomas are the most commonly seen pituitary subtype and account for 60% of pituitary adenomas. -

Multiple Endocrine Neoplasia Type 1: a Case Report and Review of the Literature
Cent. Eur. J. Med. • 9(3) • 2014 • 424-430 DOI: 10.2478/s11536-013-0297-8 Central European Journal of Medicine Multiple endocrine neoplasia type 1: a case report and review of the literature Case Report Audrius Šileikis1,2, Edvinas Kildušis*1,2, Ramūnas Janavičius3, Kęstutis Strupas1,2 1 Vilnius University, Faculty of Medicine, 03101, Vilnius, Lithuania 2 Vilnius University Hospital Santariskiu Klinikos, Center of Abdominal Surgery, 08661, Vilnius, Lithuania 3 Vilnius University Hospital Santariskiu Klinikos, Hematology, Oncology and Transfusion Medicine Center,, 08661, Vilnius, Lithuania Received 31 March 2013; Accepted 16 July 2013 Abstract: Multiple endocrine neoplasia syndrome, type 1 (MEN1) is an underdiagnosed autosomal dominant inherited cancer predisposition syndrome with inter- and intrafamilial variability without a known genotype-phenotype correlation. Disease is caused by mutations in the MEN1 gene located on chromosome 11, but other genes (CDKN1B, AIP) and mechanisms might be involved too. We performed retrospective case series study of MEN1 syndrome patient and his family and present our experience of management of genetically confirmed 9 MEN1 syndrome large family members from Lithuania with novel MEN1 gene mutation (MEN1 exon 6 – c. 879delT (p.Pro293Profs*76)) and delineate its clinical phenotype. At present the diagnosis of MEN1 syndrome must be established by direct mutation testing. MEN1 syndrome patients, their relatives and patients suspected of MEN1 are eligible for mutation testing. Patients with MEN1 have a shorter life expectancy than the general population. MEN1 patients and mutation carriers should be subjected to periodic screening in order to detect manifestations in an early stage. Early genetic diagnosis and subsequent periodic screening is associated with less morbidity and mortality at follow-up. -

Multiple Endocrine Neoplasia Type 2: an Overview Jessica Moline, MS1, and Charis Eng, MD, Phd1,2,3,4
GENETEST REVIEW Genetics in Medicine Multiple endocrine neoplasia type 2: An overview Jessica Moline, MS1, and Charis Eng, MD, PhD1,2,3,4 TABLE OF CONTENTS Clinical Description of MEN 2 .......................................................................755 Surveillance...................................................................................................760 Multiple endocrine neoplasia type 2A (OMIM# 171400) ....................756 Medullary thyroid carcinoma ................................................................760 Familial medullary thyroid carcinoma (OMIM# 155240).....................756 Pheochromocytoma ................................................................................760 Multiple endocrine neoplasia type 2B (OMIM# 162300) ....................756 Parathyroid adenoma or hyperplasia ...................................................761 Diagnosis and testing......................................................................................756 Hypoparathyroidism................................................................................761 Clinical diagnosis: MEN 2A........................................................................756 Agents/circumstances to avoid .................................................................761 Clinical diagnosis: FMTC ............................................................................756 Testing of relatives at risk...........................................................................761 Clinical diagnosis: MEN 2B ........................................................................756