Arum Palaestinum Poisoning: Revenge of the Witch
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evaluation of Taste, Total Phenols and Antioxidant for Fresh, Roasted, Shade Dried and Boiled Leaves of Edible Arum Palaestinum Bioss
Research Article www.marmarapharmj.com Evaluation of taste, total phenols and antioxidant for fresh, roasted, shade dried and boiled leaves of edible Arum palaestinum Bioss Mohammad Qneibi1*, Nidal Jaradat2, Abed Naser Zaid2, Nawaf Abu-Khalaf3, Abdel – Razzak Natsheh4, Fatima Hussein2 1 Department of Biomedical Sciences, Faculty of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine. 2 Department of Pharmacy, Faculty of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine. 3 Department of Horticulture and Extension, Faculty of Agricultural Sciences Technology, Palestine Technical University – Kadoorie, Tulkarm, Palestine. 4 Department of Computer Information Systems, Faculty of Engineering and Information Technology, An-Najah National University, Nablus, Palestine. ABSTRACT: Arum palaestinum is one of the famous wild plants that have been used since the ancient time in the Palestinian folk food and medicine. However, it needs particular cooking steps to decrease its numbing taste. We investigated the impact of cooking, measures on taste, total phenols and antioxidant activity of wild A. palaestinum by using an Alpha-Astree Electronic tongue (ET), which is used for food taste assessment. In this study, the A. palaestinum was cooked in different ways. We used Folin Ciocalteu’s process to compare total phenols, where radical scavenging assay was used to evaluate the antioxidant activity using 2, 2-diphenyl- 1-picrylhydrazyl-hydrate (DPPH). Our results showed that a very significant discrimination of the samples with different distances between groups (p-values < 0.001) in the ET results coupled with the principal component analysis (PCA). The samples were in the following order in term of numbing taste: Fresh > dried > cooked. -

Cytotoxic Activity and Phytochemical Analysis of Arum Palaestinum Boiss
944 Asian Pac J Trop Biomed 2015; 5(11): 944–947 HOSTED BY Contents lists available at ScienceDirect Asian Pacific Journal of Tropical Biomedicine journal homepage: www.elsevier.com/locate/apjtb Original article http://dx.doi.org/10.1016/j.apjtb.2015.07.019 Cytotoxic activity and phytochemical analysis of Arum palaestinum Boiss. Mai Mohammed Farid1, Sameh Reda Hussein1*, Lamiaa Fawzy Ibrahim1, Mohammed Ali El Desouky2, Amr Mohammed Elsayed2, Ahmad Ali El Oqlah3, Mahmoud Mohammed Saker4 1Department of Phytochemistry and Plant Systematic, National Research Center, 12311 Cairo, Egypt 2Department of Biochemistry, Cairo University, Cairo, Egypt 3Department of Biological Sciences, Yarmouk University, Jordan 4Department of Plant Biotechnology, National Research Center, 12311 Cairo, Egypt ARTICLE INFO ABSTRACT Article history: Objective: To evaluate the in vitro cytotoxic activity of the fractionated extract as well as Received 28 May 2015 isolated compounds of Arum palaestinum Boiss. (A. palaestinum) (black calla lily), and to Received in revised form 25 Jun, identify the volatile components which may be responsible for the potential antitumor 2nd revised form 26 Jun 2015 activity. Accepted 15 Jul 2015 Methods: A. palaestinum was collected from its natural habitats and subjected to Available online 18 Aug 2015 phytochemical analysis for separation of pure compounds. In vitro cytotoxic activity was investigated against four human carcinoma cell lines Hep2, HeLa, HepG2 and MCF7 for the fractionated extract and isolated compounds. While, the diethyl ether fraction was Keywords: subjected to GC–MS analysis as it exhibited the most potent cytotoxic effect to evaluate Black calla lily the active constituents responsible for the cytotoxic activities. Araceae Results: Four flavonoid compounds were isolated (luteolin, chrysoeriol, isoorientin, Flavonoids isovitexin) from the diethyl ether and ethyl acetate. -

Poverty and Charity in Roman Palestine
Poverty and charity in Roman Palestine Gildas Hamel Abstract The present book reformats the text, notes, and appendices of the origi- nal 1990 publication by the University of California Press. Its pagination is different. There is no index. i D’ur vamm ha d’ur breur aet d’an Anaon re abred A.M.G. 31 Meurzh 1975 Y.M.H. 12 Geñver 1986 Contents Contents ii List of Figures iv List of Tables iv Introduction ix 1 Daily bread 1 1.1 Food items ............................. 2 1.2 Diets ................................ 19 1.3 Diseases and death ........................ 55 1.4 Conclusion ............................ 58 2 Poverty in clothing 61 2.1 Common articles of clothing ................... 61 2.2 Lack of clothing .......................... 70 2.3 Clothing and social status .................... 81 2.4 Conclusion ............................ 104 3 Causes of poverty 107 3.1 Discourse of the ancients on yields . 108 3.2 Aspects of agriculture: climate and soil . 116 3.3 Work and technical standards . 125 3.4 Yields ............................... 145 3.5 Population of Palestine . 159 3.6 Conclusion ............................ 163 4 Taxes and rents 165 4.1 Roman taxes . 168 ii Contents iii 4.2 Jewish taxes and history of tax burden . 171 4.3 Labor and ground rents . 176 4.4 Conclusion ............................ 190 5 The vocabulary of poverty 193 5.1 Explicit vocabulary: Hebrew, Aramaic, and Greek . 196 5.2 Explicit vocabulary: self-designations . 209 5.3 Greek and Jewish views on poverty and wealth . 229 5.4 Implicit vocabulary . 239 5.5 Conclusion ............................ 248 6 Charity in Roman Palestine 251 6.1 Discourses on charity . -

Conservation, Genetic Characterization, Phytochemical and Biological Investigation of Black Calla Lily: a Wild Endangered Medicinal Plant
Asian Pac J Trop Dis 2016; 6(10): 832-836 832 Contents lists available at ScienceDirect Asian Pacific Journal of Tropical Disease journal homepage: www.elsevier.com/locate/apjtd Review article doi: 10.1016/S2222-1808(16)61141-6 ©2016 by the Asian Pacific Journal of Tropical Disease. All rights reserved. Conservation, genetic characterization, phytochemical and biological investigation of black calla lily: A wild endangered medicinal plant Mai Mohammed Farid1*, Sameh Reda Hussein1, Mahmoud Mohammed Saker2 1Department of Phytochemistry and Plant Systematic, National Research Center, Dokki, Giza, Egypt 2Department of Plant Biotechnology, National Research Center, Dokki, Giza, Egypt ARTICLE INFO ABSTRACT Article history: Scientists continue to search for and conserve plants whose medicinal properties have become Received 14 Jun 2016 crucial in the fight against diseases. Moreover, lessons from folk medicine, indigenous Received in revised form 4 Jul, 2nd knowledge and Chinese medicine on crude extracts points to possible findings of novel revised form 8 Aug, 3rd revised form promising and strong pharmaceutically bioactive constituents. Arum palaestinum, commonly 10 Aug 2016 known as black calla lily, is one of the most important medicinal plants belonging to the family Accepted 22 Aug 2016 Araceae, which has not been well studied. Little is known about its pharmaceutically bioactive Available online 25 Aug 2016 constituents and the effective conservation through the use of biotechnology. Thus, Arum Palaestinum is selected and reviewed for its phytochemical analysis and biological activities. Keywords: Besides, the tissue culture and genetic characterization developed for effective conservation of Arum palaestinum the plant were also summarized. Tissue culture Phytochemical analysis Antioxidant Anticancer 1. -

Pollination in the Genus Arum-A Review
148 AROIDEANA, Vol. 27 Pollination in the Genus Arum-a Review Marc Gibernau*, David Macquart, and Gilles Przetak Laboratoire d'Evolution & Diversite Biologique Unlversite de Toulouse m 118 Route de Narbonne, Bat. IV R 3-B 2 31062 Toulouse Cedex 4 France *e-mail: [email protected] ABSTRACT KEYWORDS insect, pollinators, inflorescence, ther The 28 species of the genus Arum (Ar mogenesis, floral odor, morphology, Ara aceae) attract and temporarily trap insects ceae. (mainly flies, and beetles in a few cases) during a complex pollination process. At INTRODUCTION anthesis, the appendix of the inflorescence produces heat and emits a specific odor History which attracts insects. The lured insects Arum have been known since Antiquity are trapped within the floral chamber (Theophrastus, Pliny and Dioscorides). when stigmas are receptive. They will be The description "Arum oificinarum" ap released about 24h later after pollen emis peared during the Middle-Ages because of sion, ensuring pollen dissemination. Stud their medicinal properties, but this term ies on the reproductive biology of the ge designated all kinds of aroids for about nus have shown some degree of variability four centuries (Prime,1960; Fridlender, in the pollination strategies: morphological 1999a). During this period several authors variations, flowering and heating periods, dealt with Arum (see Croat, 2000 for more odor types and the type of pollinating in details). The binomial name Arum macu sects. latum is attributed to Tabernaemontanus Most species of Arum have never been around 1590, but it has been used with a studied in depth but data available from taxonomic "value" only after the classifi the literature indicate quite a high diversity cation work of Linnaeus in 1753 (Boyce, of pollination strategy within this genus. -

Assessment of Phenotypic Variation of Arum Species in Jordan
Jordan Journal of Agricultural Sciences, Volume 4, No.4, 2008 Assessment of Phenotypic Variation of Arum Species in Jordan Siham Al-Lozi* , Ibrahim Makhadmeh**, Mahmud Duwayri***, Rida Shibli** and Hussein Migdadi* ABSTRACT Twenty-one locations scattered over eight provinces in Jordan were surveyed to assess the ecogeographical distribution of wild Arum species. Twenty-six morphological traits were measured on the collected species and populations to study the phenotypic diversities among and within species. Based on mean and standard deviation values, the highest variations were recorded for plant height, plant span, corm weight, spathe length, spadix length, leaf length and leaf mid-vein characters. Canonical discriminant analysis showed that leaf waxiness, spadix colour, spathe colour, leaf length, leaf width, plant span and leaf mid-vein are the main descriptors that can be used to differentiate among Arum species. Based on Euclidean distance coefficient, morphological characters showed a significant separation between Arum species with a similarity of 90.28% between A. palaestinum and A. dioscoridis, 74.90% between A. hygrophilum and A. dioscoridis and 82.18% between A. palaestinum and A. hygrophilum. The overall similarity analysis showed that the coefficient of similarity 81.40% was recorded among species over locations and 74.17% for species and locations combination. The results showed that Arum populations belonging to the same species are grouped in the same clusters regardless of collection site. In addition to the conservation of collected accessions in an operational gene bank, it is recommended to promote also the in situ conservation of Arum species. Keywords: Arum species, Phenotypic variation, Medicinal plants, ex situ conservation. -
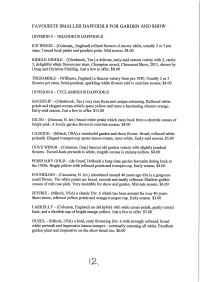
Favourite Smaller Daffodils for Garden and Show
FAVOURITE SMALLER DAFFODILS FOR GARDEN AND SHOW DIVISION 5 — TRIANDRUS DAFFODILS ICE WINGS — (Coleman„ England) refined flowers of snowy white, usually 2 or 3 per stem. Turned back petals and pendent poise. Mid season. $4.00 RIDDLE DIDDLE — (Glenbrook, Tas.) a delicate, early-mid season variety with 2, rarely 3, delightful white flowers per stein. Champion award, Claremont Show, 2011, shown by Doug and Christine Fielding. Just a few to offer. $8.00 TRESAMBLE — (Williams, England) a famous variety from pre 1930. Usually 2 or 3 flowers per stem. Semi-pendent, sparkling white flowers mid to mid-late season. $4.00 DIVISION 6 — CYCLAMINEUS DAFFODILS BACKFLIP — (Glenbrook, Tas.) very nice form and unique colouring. Reflexed white petals and elegant corona which opens yellow and turns a fascinating chrome-orange. Early-mid season. Just a few to offer. $15.00 BILBO — (Duncan, N. Ire.) broad white petals which sway back from a shortish corona of bright pink. A lovely garden flower in mid-late season. $4.00 CAZIQUE (Mitsch, USA) a wonderful garden and show flower. Broad, reflexed white perianth. Elegant trumpet-cup opens lemon-cream, turns white. Early-mid season. $5.00 DOVE WINGS — (Coleman, Eng.) famous old garden variety with slightly pendent flowers. Turned-back perianth is white, longish corona is creamy-yellow. $4.00 FEBRUARY GOLD — (de Graaf, Holland) a long-time garden favourite dating back to the 1920s. Bright yellow with reflexed petals and trumpet-cup. Early season. $4.00 FOUNDLING - (Carncairn, N. Ire.) introduced around 40 years ago this is a gorgeous small flower. The white petals are broad, smooth and neatly reflexed. -

Arum Palaestinum: an Emerging Nutraceutical from the Mediterranean
NATURAL MEDICINE JOURNAL RESEARCH GUIDE SPONSORED BY HYATT LIFE SCIENCES ARUM PALAESTINUM: AN EMERGING NUTRACEUTICAL FROM THE MEDITERRANEAN Author: Sarah Cook, ND © 2019 IMPACT Health Media, Inc. All rights reserved. This publication may not be reproduced or distributed in any form without written permission from IMPACT Health Media, Inc. Each spring, in the rocky soils of Palestine, the Black In medical traditions among Jews and Arabs in Pal- Calla Lily blooms. Known also as Solomon’s Lily or estine, Arum Palaestinum has been employed to treat Priest’s Hood, the local people of the Mediterranean conditions that range from cancer to infections to intes- region refer to this plant as “loof.” Scientists call it tinal worms. Extracts of the leaves maintain popularity Arum Palaestinum. today—as a part of Traditional Arabic Palestinian Herbal Medicine. Growing like a weed in countries of the Mediterranean Basin, the leaves of Arum palaestinum are widely known Arum palaestinum was little known in the United States and cherished as a traditional food and medicine. After until recent years. Its introduction to the US as an boiling the leaves in water and cooking them with olive herbal supplement began when it was brought to the oil and lemon, people consume them as a delicacy— attention of a chemist by the name of Gene Zaid, PhD. in part because of the belief that they might help to Dr. Zaid is a Palestinian native who had migrated to the prevent colon cancer. US in the 1960s. On a visit to the Middle East in 2005, an elder introduced him to the plant and its purported health benefits. -

Checklist of the Vascular Plants of the Arcata Marsh & Wildlife Sanctuary
Humboldt State University Digital Commons @ Humboldt State University Botanical Studies Open Educational Resources and Data 2018 Checklist of the Vascular Plants of the Arcata Marsh & Wildlife Sanctuary, Humboldt County James P. Smith Jr. Humboldt State University, [email protected] Follow this and additional works at: https://digitalcommons.humboldt.edu/botany_jps Part of the Botany Commons Recommended Citation Smith, James P. Jr., "Checklist of the Vascular Plants of the Arcata Marsh & Wildlife Sanctuary, Humboldt County" (2018). Botanical Studies. 78. https://digitalcommons.humboldt.edu/botany_jps/78 This Flora of Northwest California-Checklists of Local Sites is brought to you for free and open access by the Open Educational Resources and Data at Digital Commons @ Humboldt State University. It has been accepted for inclusion in Botanical Studies by an authorized administrator of Digital Commons @ Humboldt State University. For more information, please contact [email protected]. A CHECKLIST OF THE VASCULAR PLANTS OF THE ARCATA MARSH & WILDLIFE SANCTUARY (HUMBOLDT COUNTY, CALIFORNIA) James P. Smith, Jr. Professor Emeritus of Botany Department of Biological Sciences Humboldt State University Arcata, California 26 July 2018 The Arcata Marsh and Wildlife Sanctuary is located at SALVINIACEAE • FLOATING FERN FAMILY the north end of Humboldt Bay. It consists of 307 acres Azolla filiculoides • Mosquito fern, water velvet • NA of freshwater and salt marshes, mud flats, tidal sloughs, grassy uplands, and five miles of paths. It is CONIFERS also the home of the city’s wastewater treatment facility. The Visitor Center is just off South G St. in CUPRESSACEAE • CYPRESS FAMILY Arcata. The marsh is a popular area for birders because Chamaecyparis lawsoniana • Port Orford-cedar • NT it is located along a major migratory pathway. -

Marj Sanour Biodiversity Preliminary Report
Marj Sanour Biodiversity Preliminary Report 2010 TABLE OF CONTENT: CHAPTER1 ..............................................................................................................................................6 INTRODUCTION AND BACKGROUND .................................................................................................6 INTRODUCTION .....................................................................................................................................8 METHODOLOGY.....................................................................................................................................9 FLORA .....................................................................................................................................................9 FLOWERING PLANTS ............................................................................................................................9 MUSHROOM ........................................................................................................................................ 13 FAUNA .................................................................................................................................................. 13 MAMMALS ........................................................................................................................................... 14 BIRDS ................................................................................................................................................... 14 REPTILES -

Cytotoxic Activity of Cyclamen Persicum Ethanolic Extract on MCF-7, PC-3 and Lncap Cancer Cell Lines
Journal of Natural Sciences Research www.iiste.org ISSN 2224-3186 (Paper) ISSN 2225-0921 (Online) Vol.10, No.2, 2020 Cytotoxic Activity of Cyclamen Persicum Ethanolic Extract on MCF-7, PC-3 and LNCaP Cancer Cell Lines Walid M. Khalilia Forensic Science Department, Al- Istiqlal University, PO. Box 10, Jericho, Palestine Abstract It is important to develop new approaches to increase the efficacy of cancer treatments. Nowadays, the uses of natural products to treat cancer are very common. In addition, working with plants that are endemic to Palestine and determining the biological activities of these plant extracts, is extremely important due to the potential for new drug development . Cyclamen persicum is used in traditional medicinal to treat anti-rheumatic, diarrhea, abdominal pains, edema, abscesses, eczema, cancer and other ailments. In this study the cytotoxic effect of C. persicum tubers and leaves ethanolic extracts were studied against MCF-7, PC-3 and LNCaP cancer cell lines, using mitochondrial dehydrogenase enzyme method . Results showed the remarkable cytotoxic activity of C. persicum extracts, against breast and prostate adenocarcinoma. For tubers extract the IC 50 value was found to be 0.05 mg/ml for the three cell lines. Although the leaves extract the IC 50 value was found to be 0.25 mg/ml for PC-3 and MCF-7 cell lines, while LNCaP cell inhibition were less than 30% at all tested leaves extract concentrations. MCF-7 cells exhibited the highest sensitivity to the C. persicum extracts, compared to PC-3 and LNCaP cell lines evaluated. In contrast, LNCaP cells generally exhibited the lowest sensitivity to extracts. -

Chemical Composition, Phenolics, Anthocyanins Concentration and Antioxidant Activity of Ten Wild Edible Plants
Food and Nutrition Sciences, 2015, 6, 581-590 Published Online May 2015 in SciRes. http://www.scirp.org/journal/fns http://dx.doi.org/10.4236/fns.2015.67061 Chemical Composition, Phenolics, Anthocyanins Concentration and Antioxidant Activity of Ten Wild Edible Plants Khalil I. Ereifej1*, Hao Feng1, Taha Rababah2, Ali Almajwal3, Muhammad Alu’datt2, Sana I. Gammoh2, Layal I. Oweis2 1Department of Food Science and Human Nutrition, University of Illinois, Urbana-Champaign, Urbana, USA 2Department of Food Science and Human Nutrition, Jordan University of Science and Technology, Irbid, Jordan 3Department of Community Health Sciences, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia Email: *[email protected], *[email protected] Received 28 August 2014; accepted 30 April 2015; published 4 May 2015 Copyright © 2015 by authors and Scientific Research Publishing Inc. This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/ Abstract Plants were collected and prepared for chemical analysis, total phenolics, anthocyanins concen- trations, and free radical scavenging activity. Results showed that, protein concentration of Malva parviflora (22.9%) was the highest among the plants. Ruta chalepensis had high levels of fat and carbohydrates (4.2% and 51.7%, respectively), but had the lowest level of ash (8.7%). Mineral concentrations varied and found to have appreciable amounts of Ca, Na, K, Cu, Fe, Mg, Mn, Zn and P. Total phenolic ranged from 163.1 (Tetragonolobus palaestinus) to 1328.8 mg GAE/100g (Ruta chalepensis). Anthocyanins ranged between 18.1 (Gundelia tournefortii) and 100.1 mg/100g (Ru- mex acetosella).