Board of Health Minutes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PILOT) As Provided by G.L
Z!tlje Qtommonkua1t1j of aacIjuett AUDITOR OF THE COMMONWEALTH DIVISION OF LOCAL MANDATES 100 NASHUA STREET, ROOM 1010 A.III,,JOSEPH DENUCCI BOSTON, MASSACHUSETTS 02114 TEL. (617) 727-0980 AUOITOR 1-800-462-COST A REVIEW OF Tm FINANCIAL IMPACT OF Tiu c.58 PAYMENTS-IN-LIEU-OF-TAXES (PiJ.oT) PROGRAM ON MASSACJTUSErrS Crrws Ar Towrs OCTOBER 1994 OFFICE OF THE STATE AUDITOR DwIsIoN OF LOCAL MANDATES A. JOSEPH DENUCCI, AUDITOR 4 ZJJt- QIummnnfttpilth uf ic1urtt AUDITOR OF THE COMMONWEALTH STATE HOUSE, BOSTON 02133 A. JOSEPH DENUCCI TEL, (617) 727-2075 AUD!TOR October 27, 1994 His Excellency William F. Weld, Governor The Honorable William M. Bulger, President of the Senate The Honorable Charles F. Flaherty, Speaker of the House of Representatives Honorable Members of the General Court I respectfully submit for your consideration this review of the local fiscal impact of insufficient distributions to cities and towns for payments-in-lieu-of-taxes for state owned land (PILOT) as provided by G.L. c. 58, ss. 13-17. This study was undertaken in accordance with G.L. c. 11, s. 6B, which allows the State Auditor’s Division of Local Mandates to determine the financial effect of state laws impacting cities and towns. G.L. c. 58, s. 17 provides a reimbursement formula to assist municipalities hosting certain tax-exempt state properties. My report estimates that over the past seven years, cities and towns received $58.4 million in reimbursements rather than the $116.9 million called for by the statutory formula--or 50% of their entitlements on average. -

Of 379 Institutons Receiving a Questionnaire on Their Paramedical
DOCUMENT RESUME ED 022 442 JC 680 311 INVENTORY 1967: MASSACHUSETTS HEALTH MANPOWER TRAINING AT LESS THAN A BACCALAUREATE LEVEL. PART I. Training Center for Comprehensive Care, Jamaica Plain, Mass. Pula Date 67 Note-96p. EDRS Price MF-S0.50 HC-$3.92 Descriptors-*HEALTH OCCUPATIONS, *JUNIOR COLLEGES, *MANPOWER DEVELOPMENT, MEDICAL RECORD TECHNICIANS, fvEDICAL SERVICES, NURSES, NURSES AIDES, *PARAMEDICAL OCCUPATIONS, *SUBPROFESSIONALS, THERAPISTS, VOCATIONAL EDUCATION Identifiers *Massachusetts Of 379 institutonsreceiving a questionnaire on their paramedical training programs, 369 replied. They supplied data on 465 courses in 56 job categories. Those conducting the courses include hospitals, nursing homes, highschools, colleges, universities, technical schools, community service agencies, the State Department of Public Health, and an industrial plant. For each job category are given (1) a definition, (2) a detailed description of the curriculum, (3) the teaching staff, (4) a hst of the places offering the course, (5) the cost of the course, (6) in-training payment, if any, for taking the course, (7) length of time required for the course, and (8) ehgibility requirements for the trainee. (HH) U.S.melitillMMIN DEPARIMENTOFFICE OF HEALTH, OF EDUCATION EDUCATION &WELFARE THIS DOCUMENT HAS BEEN REPRODUCEDEXACTLY AS RECEIVED FROM THE PERSONPOSITIONSTATEDMASSACHUSETTS DO OR OR NOT ORGANIZATION POLICY. NECESSARILY ORIGINATING REPRESENT IT.OFFICIALPOINTS OFFICE OF VIEW OF EDUCATION OR OPINIONS ATHEALTH LESS THANMANPOWERAINVENTORY BACCALAUREATETRAITLEVEL ING fteb 1967 Training Center170 Mortonfor Comprehensive Street Care i Jamaica PARTPlain, ONEMass. 02130 1 MASSACHUSETTS IHEALTH N V E N T O RMANPOWER Y 19 6 7 TRAINING 1 AT LESS THAN ACONTENTS BACCALAUREATELEVEL IntroductionSponsorship of the survey Pages1-2 TheMethodDefinition Situation used ofin trainingconducting the survey 3-5 Location.JobNumberrequirements. -
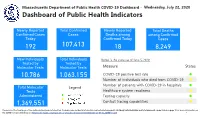
Dashboard of Public Health Indicators
7/22/2020 Duplicate of Public Health Indicators Massachusetts Department of Public Health COVID-19 Dashboard - Wednesday, July 22, 2020 Dashboard of Public Health Indicators Newly Reported Total Confirmed Newly Reported Total Deaths Confirmed Cases Cases Deaths among among Confirmed Today Confirmed Today Cases 192 107,413 18 8,249 New Individuals Total Individuals Below is the status as of June 5, 2020: Tested by Tested by Molecular Tests Molecular Tests Measure Status 10,786 1,063,155 COVID-19 positive test rate ⚫ Number of individuals who died from COVID-19 ⚫ Number of patients with COVID-19 in hospitals ⚫ Total Molecular Legend Tests Healthcare system readiness ⚫ Administered Testing capacity ⚫ 1,369,551 Contact tracing capabilities ⚫ Please note: The front page of the dashboard has been reformatted. Probable case and death information can be found on page 21. Antibody tests (individual and total numbers) can be found on page 7. For more information on the COVID-19 case definition, see https://cdn.ymaws.com/www.cste.org/resource/resmgr/2020ps/Interim-20-ID-01_COVID-19.pdf 1 1/1 7/22/2020 Public Health Indicators2 Massachusetts Department of Public Health COVID-19 Dashboard - Wednesday, July 22, 2020 Percent Change Since Dashboard of Public Health Indicators April 15th 7 Day Weighted 2.0% 2.0% 2.0% 1.9% Average of Positive 1.9% 1.9% 2.0% 1.9% 1.9% 1.9% 1.9% 1.9% 2.0% 1.8% 1.8% 1.8% 1.8% Molecular Test Rate 1.8% 1.7% 1.8% 1.9% 1.7% 1.7% 1.8% 1.7% 1.7% 1.7% 1.7% 1.7% 1.7% 1.8% -94 % 1.7% 1.6% June June June June June June June June June -

1956Acts0711.Pdf (1.092Mb)
Acts, 1956. — Chap. 711. 729 tracts and agreements and do all other things necessary to co-operate with the United States in the construction of highways now located within the area of certain projects, which are authorized by congress under the flood control acts of June twenty-second, nineteen hundred and thirty- six, June twent3''-eighth, ninet^een hundred and thirty-eight and December twent3''-second, nineteen hundred and fiftj''- five and all other acts amendatory thereto, and which are specified in chapter six hundred and thirteen of the acts of nineteen hundred and fifty-six. Land or rights in land may be acquired for such highways by eminent domain under chapter seventy-nine of the Gen- eral Laws by the department in behalf of the commonwealth, or in behalf of the city or town in which the land lies, at the option of the department. Section twenty-five of chapter eighty-one of the General Laws shall apply to highways laid out or constructed under authority of this act. Section 2. For the purposes authorized by this act the department may use any funds which may be available for the construction and maintenance of state highways, and aU reimbursements from the United States for sums so ex- pended shall be received by the state treasurer and shall be expended upon the order or approval of the department without specific appropriation. Section 3. The department is hereby authorized to aban- don to the United States any land or rights in land which may have been taken or acquu'ed by it and which are within the area of said projects; provided, that the United States has acquired the title to the abutting land in conformity with said chapter six hundred and thirteen of the acts of nineteen hundred and fifty-six. -

1974 ANNUAL TOWN REPORT TOWN of NORFOLK Norfolk County Incorporated 1870
. NORFOLK 1974 ANNUAL TOWN REPORT TOWN OF NORFOLK Norfolk County Incorporated 1870 Population-( 1970 Census) 4752 Actual Population 4005 Prison Colony Population 747 Senators in Congress Hon. Edward Kennedy of Boston Hon. Edward W. Brooke of Newton Congressional District-! 0th Hon. Margaret M. Heckler, Congresswoman, Wellesley State Representative-24th Norfolk George L. Woods, Jr., Franklin State Senatorial District-5th Norfolk & Suffolk State Senator-Joseph Timilty, Boston Councilor District-2nd Norfolk County Seat-Dedham County Commissioners James J. Collins George B. McDonald Thomas K. McManus John P. Concannon, Clerk County Treasurer James M. Collins County Engineer Alvah Downs Sheriff of Norfolk County Clifford H. Marshall, Dedham REGISTERED VOTERS 1974 Total 2260 Democrats 445 Republicans 563 Independents 1252 ()ne llundre,d Fourth Annual Statement of the Ueceipts and Expenditures of the 1'own of Norfolk Massachusett.~ FOR THE YEAR ENDING DECEMBER 31, 1974 ) With Reports of TOWN OFFICERS, SCHOOL COMMITTEE VITAL STATISTICS OF THE YEAR COPY GRAPHICS,JNC. Mc ti way, Massachusetts 1915 Ju ~lJl!ltmnriam 11111111 I LEWIS MARIANI 1896 • 1974 Fire Fighter Special Police Officer AGNES BRISTOL 1885 · 1974 Library Trustee J. HENRY SHIBLEY 1919 · 1974 Advisory Board WILLIAM T. RAY, SR. 1892 • 1974 Measurer of Wood & Bark Ju jlrmnrtam --· THOMAS HOVEY 1936 - 1974 War Memorial Study Committee EDWARD E. HALE, SR. 1896 - 1974 Selectman Civil Defense Police Officer ) LOUIS DROWNE 1907 - 1974 Dog Officer TIU+. WARDLN Term expires l 1>76 Kenne th E. Tripp fRl.lSTEE OF JOSIAH WARE FUND The Town Treasurer f:tlMMIS~!ONEHS OF TRUST FUNDS Board of Selectmen CONSTABLES, teuus to expire I 97'1 'fr ls T. -

Annual Report
PUBLIC D O C U M E N T NO. 6 (ÜmnmmutiEaltlj nî iiasHarirnsTtis DEPARTMENT OF THE AUDITOR ANNUAL REPORT FOR THE FISCAL YEAR ENDING JUNE 30, 1958 THOMAS J. BUCKLEY STATE AUDITOR 300 SETS-9-58-923632 STATE LIBRARY li- iv,^ - - OCT 23 1958 STATE HOUSE, BOSTON MASS OFT 3 3 6 , 7 ^ 3 A31r I DEPARTMENT OF THE AUDITOR A ANNUAL REPORT For the FISCAL YEAR ENDING JUNE 30, 1958 STATE AGENCY AUDITS I have the honor to submit the Annual Report of the Department of the Auditor for the fiscal year, July 1, 1957 to June 30, 1958. Section 12 of Chapter 11 of the General Laws defines the duties of the Department of the State Auditor. "SECTION 12. The department of the state auditor shall annually make a careful audit of the accounts of all departments, offices, commissions, institutions and activi ties of the commonwealth, including those of the income tax division of the department of corporations and taxa tion, and for said purpose the authorized officers and employees of said department of the state auditor shall have access to such accounts at reasonable times and said department may require the production of books, documents and vouchers, except tax returns, relating to any matter within the scope of such audit. The accounts of the last named department shall be subject at any time to such examination as the governor and council or the general court may order. Said department shall comply with any written regulations, consistent with law, relative to its duties made by the governor and council. -
On1004240031-1976.Pdf (1.825Mb)
THE CXl4MONWEALTH OF MASSACHUSETTS BO.ARD OF REGISTRATICti IN HURSING AKHUAL REPORT FISCAL 1976 MR PUBLI CATIQl s #9703-10-100•4•77-CR 614. 24MJ APPR0RD BI s illred. C. Holland, State Parcbaeing Agent ·B666r 1976 c.l 1'HE C(H(JlNWEALTH OF MASS.AOHUSRf!S BOARD OF REGISTRATiaiJ D NtJRSING ,PURPOSE---OF REPORT Through this do~t, the Board of Registraticn in Nur~ complies with Seetim 78, Chapter 112, General Laws, wbi~ re~s the Board to •:make an annual report of the condition et nursing in the {lomllcnwealth." The report CO"f'ers the fiscal year period frcm J1ll7 1, 197.5 through June JO, 1976. PURPOSE .AND FffiOlIONS OF BOARD OF REGISTRATICll IN NURSING The Board of Registration in Nursing, an adllinistrative agenc;y witbin the govermaental organizati<11 ot the Connonwealtb, is delegated the respmsibilii;y tor illplementaticm ot those statutes and sections of statutes t.bat provide legal control of nursing practice. '!'he ftmda- 11ental purpose of the Board is to sa:teguaJ'(l the welfare of the citizens of tJie Collllonwealth who require the services of professimal and practical nurses. To ful.f'ill its purpose, the ·Board has two• aajor tmct:1.cmst 1. Li.censure of prof'essimal and practical nurses; 2. Determinatim arid maintenance of nursing educatim standards that are basic to licensure of ,ea£~ practiticners through approval ot nursing education progrus. MEMBERSHIP OF THE BOARD Qua.litieatians tor membership are established by Section 1.3, Chapter 1.3, General Laws, as amended. Secticn 13 provides that the Beard aembership shall oonsist o.f five registered nurses, 011e licensed practical nurse, two qualified physicians, two hospital adll:l.nistrators, two hospital trustees and one public Jlellber. -

Directory of Labor Organizations in Massachusetts
BOSTON PUBLIC LIBRARY cm! Public Document 3 9999 06316 189 5 No. 15 <E\)t (tammaxxwmitl} of fHasimrljiiHrtls Francis W. Sargent, Governor DIRECTORY OF LABOR ORGANIZATIONS 1974 Executive Office of Manpower Affairs Mary B. ISetvman, Secretary GOV DOC 9331 0744 1974 Published by the Massachusetts Department of Labor anil Industries Rocco Alberto, Commissioner •• Publication of this Document Approved by Alfred C. Holland, State Purchasing Agent. 2300-6-74-092048 Estimated cost per copy: $.78 DIRECTORY OF LABOR ORGANIZATIONS IN MASSACHUSETTS 19 7 4 (With Statistics of Membership, 1972-73-74) Compiled by the DIVISION OF STATISTICS Thomas M. Raftery, Director MASSACHUSETTS DEPARTMENT OF LABOR AND INDUSTRIES Rocco Alberto, Commissioner INTRODUCTION The Material here presented constitutes the Sixty-Ninth Directory of Labor Organizations in Massachusetts. The first Directory of this kind was published in August, 1902. The term "Labor Organizations" as used in this Directory is a group of employees or wage earners organized for the purpose of improving their status through negotiations with employers. The organization is usually a party to either a written or verbal agreement concerning wages and conditions of employment. Since the last Directory was issued many new unions have been organized, others have become inactive or disbanded. The Department has records of unions in existence by reason of "statements" required by Chapter 618, Acts of 1946 (Revised by Chapter 394, Acts of 1949). This edition consists of four divisions, as follows: I. " National and International Organizations " having one or more affil- iated local unions in the United States, (pages 3-13). II. " Delegate Organizations " consisting of organizations composed of delegates from local unions whose members are in trades or industries of a like character within a definite district, or of delegates from local unions in the same locality, not necessarily in similar trades (pages 14-21). -

Directory of Labor Organizations in Massachusetts
\/ t> \. r- t\ . r\ ^ " •^- BOSTON P UBLIC LIBRARY jj ^ Piihlic Document No. 15 3 9999 06316 184 6 Francis W . Sargent, Governor DIRECTORY OF LABOR ORGANIZATIONS 1969 ANNUAL REPORT ON THE STATISTICS OF LABOR GOV DOC 9331 .0744 1969 Published by the Massachusetts Department of Labor and Industries Rocco Alberto, Commissioner •• Publication of this Document Approved by Alfred C. Holland. State Purchasing Agent. 1800-6-69-949795 Estimated cost per copy: $.59 DIRECTORY OF LABOR ORGANIZATIONS IN MASSACHUSETTS 19 6 9 (With Statistics of Membership, 1967-68-69) Labor Bulletin No. 212 Compiled by the DIVISION OF STATISTICS Thomas M. Raftery, Director MASSACHUSETTS DEPARTMENT OF LABOR AND INDUSTRIES Rocco Alberto, Commissioner INTRODUCTION The material here presented constitutes the Sixty-Fourth Directory of Labor Organizations in Massachusetts. The first Directory of this kind was published in August, 1902, The term "Labor Organizations" as used in this Directory is a group of employees or wage earners organized for the purpose of improving their status through negotiations with employers. The organization is usually a party to either a written or verbal agreement concerning wages and conditions of employment. Since the last Directory was issued many new unions have been organized, others have become inactive or disbanded. The Department has records of unions in existence by reason of "statements" required by Chapter 618, Acts of 1946 (Revised by Chapter 394, Acts of 1949). This edition consists of four divisions, as follows: I. " National and International Organizations " having one or more affil- iated local unions in the United States, (pages 4-14). II. " Delegat e Organizations " consisting of organizations composed of delegates from local unions whose members are in trades or industries of a like character within a definite district, or of delegates from local unions in the same locality, not necessarily in similar trades, (pages 15-24). -

Town of Cohasset
TOWN OF COHASSET ANNUAL REPORT 1952 (3ln jM^martam ROSCOE G. PRATT Born ^ September 18, 1889 Died — March 28, 1952 Served as Field Driver 1934 through 1938 Appointed Deputy, Fire Department, Beechwood District — 1936 Appointed Superintendent of Moth Department 1938, 1940 through 1952 Elected Tree Warden March 9, 1940 Reelected through 1952 AINIVUAL REPORT OF THE Board of Selectmen OF THE FINANCIAL AFFAIRS OF THE TOWN OF COHASSET AND THE Report of Other Town Officers For the Year Ending December 31 1952 Annual Report, Town of Cohasset, 1952 TOWN OFFICERS, 1952 - 1953 TOWN RECORDS Elected by Ballot Moderator ROBERT B. JAMES Term expires March 1954 Town Clerk WILLIAM H. MORtelS Term expires March 1953 Selectmen, Assessors and Board of Public Welfare NORMAN CARD Term expires March 1953 IRA B. P. STOUGHTON Term expires March 1954 HELEN E. SCRIPTURE Term expires March 1955 Treasurer MAURICE R. NOONAN Term expires March 1955 Collector of Taxes GORDON E. FLINT Term expires March 1955 Tree Warden ROSGOE G. PRATT Term expires March 1953 Died on March 28, 1952 Howard Bates, Appointed to fill vacancy on March 31, 1952 Highway Surveyor WILLIAM T. BARNES Term expires March 1954 Constables EDWARD BARROW ROYAL A. BATES H. MONTY LaFLAMME STEPHEN H. ROONEY EDMUND H. MacIVER School Committee JOHN H. DEAN Term expires March 1953 FRANCIS HAGERTY Term expires March 1953 GEORGE STEWART JASON Term expires March 1954 HARRY H. REED, JR Term expires March 1954 WILLIAM E. POLAND Term expires March 1955 RICHARD SULLIVAN Term expires March 1955 Board of Health EDWARD E. TOWER Term expires March 1953 NATHANIEL HURWITZ Term expires March 1954 FRED W. -

Ocm39986872-1943-HB-1276.Pdf (1.927Mb)
HOUSE No. 1276 Cfte Commontoealtf) of 00a$sacJ)u$etts SPECIAL REPORT OF THE DEPARTMENT OF MENTAL HEALTH ON THE ADVISA- BILITY AND EXPENSE OF ESTABLISH- ING A BUREAU FOR THE CARE OF INEBRIATES. [Public Health.] 100 Nashua Street, Boston, November 30, 1942. To the Honorable Senate and House of Representatives. The Department of Mental Health, acting in accord- ance with the authorization which follows, herewith re- spectfully submits its report. I. Authorization for this Report, Chapter 73, Resolves op 1943. Resolve providing foe an Investigation by the Department of Mental Health relative to the Advisability and Ex- pense or Establishing a Bureau for the Care of Inebriates. Resolved, That the department of mental health is hereby author- ized and directed to investigate the advisability of establishing a bureau for the care of inebriates, and in connection therewith to con- sider the subject matter of current house document numbered two thousand and seven, relative to the establishment in the department of public health of a bureau for the care of inebriates. Said department of mental health shall report to the general court the results of its investigation, and its recommendations, if any, together with esti- mates of cost and drafts of legislation necessary to carry such recom- mendations into effect, by filing the same with the clerk of the house of representatives on or before the first Wednesday of December in the year nineteen hundred and forty-two. Approved October 9, 19^1. 2 HOUSE — No. 1276. [Jan. The subject matter of House, No. 2007 follows: An Act relative to the Establishment of a Bureau for the Care of Inebriates under the Department of Public Health, Chapter one hundred and eleven of the General Laws, Tercentenary Edition, is hereby amended by inserting at the end the following new section: Section 190. -

Massachusetts, Department of Public Health
©Ij? (Eommotmitfaltlj of UtasarljitarttB FIFTY- THIRD AINHNIU^IL REIF©RT of the MASSACHUSETTS Department of Public Health. July 1,1966 June 30, 1967 A 53rd ANNUAL REPORT of the DEPARTMENT OF PUBLIC HEALTH July 1, 196b - June 30, 1967 ,._.;2a 1967 gTAIE HOUSE. BOSTON TABLE OF CONTENTS Page Administration < Adult Health kl Alcoholism ^2 Budget m _ _ ^q Civil Defense Section 55 Communicable Diseases j^ Dental Health ^5 Drug Addiction Rehabilitation Board 12 Food and Drugs l^o Health Education 2.6 Health Statistics 13 Hospital Facilities 66 Hospitals, Department Lakeville Hospital .... 71 Lemuel Shattuck Hospital 1+7 Massachusetts Hospital School 72 Pondville Hospital 73 Rutland Heights Hospital 73 Tewksbury Hospital 7^ Western Massachusetts Hospital 75 Laboratories, Institute of 68 Legislation Passed by I966-I967 Legislature ..... 28 Recommendations for 1968 Legislation 37 Local Health Services 5I+ Massachusetts Committee on Children and Youth Ik Massachusetts Health Research Institute, Inc 15 Maternal and Child Health Services 63 Medical Care 18 Nursing Homes and Related Facilities 1+7 Nursing Section 56 Nutrition Section ....... 57 Public Health Council k Regional Health Offices ..... 59 Research, Development, and Professional Training . 20 Regulations Promulgated by Department 22 Sanitary Engineering 51 Social Work Section 58 Training Center for Comprehensive Care 15 Tuberculosis Control 71 Venereal Diseases , . kk MASSACHUSETTS DEPARTMENT OF PUBLIC HEALTH June 30, 1967 Commissioner of Public Health, Alfred L. Frechette, M.D., M.P.H. PUBLIC HEALTH COUNCIL Alfred L. Frechette, M.D., M.P.H. , Chairman Francis B. Carroll, M.D. 196^-1967 John H. Knowles, M.D. 1964-1970 Bernard B. Berger, M.S.