NFPRHA---FP-UPDATES---Tuesday-AM---FINAL.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ANNOVERA™ (Segesterone Acetate and Ethinyl Estradiol Vaginal System) • Risk of Liver Enzyme Elevations with Concomitant Hepatitis C Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION ANNOVERA™ no earlier than 4 weeks after delivery, in females who These highlights do not include all the information needed to use are not breastfeeding. Consider cardiovascular risk factors before ANNOVERA™ safely and effectively. initiating in all females, particularly those over 35 years. (5.1, 5.5) See Full Prescribing Information for ANNOVERA™. • Liver Disease: Discontinue if jaundice occurs. (5.2) ANNOVERA™ (segesterone acetate and ethinyl estradiol vaginal system) • Risk of Liver Enzyme Elevations with Concomitant Hepatitis C Initial U.S. Approval: 2018 Treatment: Stop ANNOVERA™ prior to starting therapy with the combination drug regimen ombitasvir/paritaprevir/ritonavir. ANNOVERA™ can be restarted 2 weeks following completion of this WARNING: CIGARETTE SMOKING AND regimen. (5.3) SERIOUS CARDIOVASCULAR EVENTS • Hypertension: Do not prescribe ANNOVERA™ for females with See full prescribing information for complete boxed warning. uncontrolled hypertension or hypertension with vascular disease. If • Females over 35 years old who smoke should not use used in females with well-controlled hypertension, monitor blood ANNOVERA™. (4) pressure and stop use if blood pressure rises significantly. (5.4) • Cigarette smoking increases the risk of serious cardiovascular • Carbohydrate and lipid metabolic effects: Monitor glucose in pre events from combination hormonal contraceptive (CHC) use. (4) diabetic and diabetic females taking ANNOVERA™. Consider an alternate contraceptive method for females with uncontrolled ----------------------------INDICATIONS AND USAGE-------------------------- dyslipidemias. (5.7) ANNOVERA™ is a progestin/estrogen CHC indicated for use by females of • Headache: Evaluate significant change in headaches and discontinue reproductive potential to prevent pregnancy. (1) ANNOVERA™ if indicated. (5.8) Limitation of use: Not adequately evaluated in females with a body mass index • Bleeding Irregularities and Amenorrhea: May cause irregular bleeding of >29 kg/m2. -

209627Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 209627Orig1s000 MULTI-DISCIPLINE REVIEW Summary Review Office Director Cross Discipline Team Leader Review Clinical Review Non-Clinical Review Statistical Review Clinical Pharmacology Review Reviewers of Multi-Disciplinary Review and Evaluation SECTIONS OFFICE/ AUTHORED/ ACKNOWLEDGED/ DISCIPLINE REVIEWER DIVISION APPROVED Mark Seggel, Ph.D. OPQ/ONDP/DNDP2 Authored: Section 4.2 Digitally signed by Mark R. Seggel -S CMC Lead DN: c=US, o=U.S. Government, ou=HHS, ou=FDA, ou=People, cn=Mark R. Signature: Mark R. Seggel -S Seggel -S, 0.9.2342.19200300.100.1.1=1300071539 Date: 2018.08.08 16:29:15 -04'00' Frederic Moulin, DVM, PhD OND/ODE3/DBRUP Authored: Section 5 Pharmacology/ Digitally signed by Frederic Moulin -S Toxicology DN: c=US, o=U.S. Government, ou=HHS, ou=FDA, ou=People, Reviewer Signature: Frederic Moulin -S 0.9.2342.19200300.100.1.1=2001708658, cn=Frederic Moulin -S Date: 2018.08.08 15:26:57 -04'00' Kimberly Hatfield, PhD OND/ODE3/DBRUP Approved: Section 5 Pharmacology/ Toxicology Digitally signed by Kimberly P. Hatfield -S DN: c=US, o=U.S. Government, ou=HHS, ou=FDA, ou=People, Team Leader Signature: Kimberly P. Hatfield -S 0.9.2342.19200300.100.1.1=1300387215, cn=Kimberly P. Hatfield -S Date: 2018.08.08 14:56:10 -04'00' Li Li, Ph.D. OCP/DCP3 Authored: Sections 6 and 17.3 Clinical Pharmacology Dig ta ly signed by Li Li S DN c=US o=U S Government ou=HHS ou=FDA ou=People Reviewer cn=Li Li S Signature: Li Li -S 0 9 2342 19200300 100 1 1=20005 08577 Date 2018 08 08 15 39 23 04'00' Doanh Tran, Ph.D. -

Health Care Reform
Health Care Reform Preventative Drug list At Magellan Rx Management, we are driven to helping our clients most effectively manage changes in the prescription drug environment. As part of the Patient Protection and Affordable Care Act (PPACA), effective on or after August 1, 2012 non-grandfathered plans are required to cover select FDA-approved drug products related to preventive health services for Adults, Children and Women without a member having to pay a copayment, co-insurance, or meet a deductible. As your pharmacy benefits manager, we will support coverage of specific products at $0 copay as prescription benefit plans become subject to the law. Magellan Rx Management will also routinely update FDA-approved product lists to comply with the Preventive Health mandates and require prescriptions for product coverage. MRx has created ten specific lists that address the preventive health requirements above. A plan is required to cover all the drug lists below, either through the pharmacy or medical benefits. If the plan needs advice regarding coverage, MRx recommends the plan connect with their respective legal counsel. The content of the list will be maintained by Magellan Rx Management and will be continually reviewed and updated to ensure compliance with healthcare reform mandates. UPDATE: For plan years beginning on or after September 24, 2014 (January 1, 2015 for calendar year plans), non-grandfathered health plans are required to cover prescription medications designed to reduce the risk of breast cancer in women, without cost-sharing, subject to reasonable medical management. These required drugs have been added to the “Preventive Health for Adults, Children and Women: Prescription and OTC Products” list below. -

Vaginal Administration of Contraceptives
Scientia Pharmaceutica Review Vaginal Administration of Contraceptives Esmat Jalalvandi 1,*, Hafez Jafari 2 , Christiani A. Amorim 3 , Denise Freitas Siqueira Petri 4 , Lei Nie 5,* and Amin Shavandi 2,* 1 School of Engineering and Physical Sciences, Heriot-Watt University, Edinburgh EH14 4AS, UK 2 BioMatter Unit, École Polytechnique de Bruxelles, Université Libre de Bruxelles, Avenue F.D. Roosevelt, 50-CP 165/61, 1050 Brussels, Belgium; [email protected] 3 Pôle de Recherche en Gynécologie, Institut de Recherche Expérimentale et Clinique, Université Catholique de Louvain, 1200 Brussels, Belgium; [email protected] 4 Fundamental Chemistry Department, Institute of Chemistry, University of São Paulo, Av. Prof. Lineu Prestes 748, São Paulo 05508-000, Brazil; [email protected] 5 College of Life Sciences, Xinyang Normal University, Xinyang 464000, China * Correspondence: [email protected] (E.J.); [email protected] (L.N.); [email protected] (A.S.); Tel.: +32-2-650-3681 (A.S.) Abstract: While contraceptive drugs have enabled many people to decide when they want to have a baby, more than 100 million unintended pregnancies each year in the world may indicate the contraceptive requirement of many people has not been well addressed yet. The vagina is a well- established and practical route for the delivery of various pharmacological molecules, including contraceptives. This review aims to present an overview of different contraceptive methods focusing on the vaginal route of delivery for contraceptives, including current developments, discussing the potentials and limitations of the modern methods, designs, and how well each method performs for delivering the contraceptives and preventing pregnancy. -

Patent Application Publication ( 10 ) Pub . No . : US 2019 / 0192440 A1
US 20190192440A1 (19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2019 /0192440 A1 LI (43 ) Pub . Date : Jun . 27 , 2019 ( 54 ) ORAL DRUG DOSAGE FORM COMPRISING Publication Classification DRUG IN THE FORM OF NANOPARTICLES (51 ) Int . CI. A61K 9 / 20 (2006 .01 ) ( 71 ) Applicant: Triastek , Inc. , Nanjing ( CN ) A61K 9 /00 ( 2006 . 01) A61K 31/ 192 ( 2006 .01 ) (72 ) Inventor : Xiaoling LI , Dublin , CA (US ) A61K 9 / 24 ( 2006 .01 ) ( 52 ) U . S . CI. ( 21 ) Appl. No. : 16 /289 ,499 CPC . .. .. A61K 9 /2031 (2013 . 01 ) ; A61K 9 /0065 ( 22 ) Filed : Feb . 28 , 2019 (2013 .01 ) ; A61K 9 / 209 ( 2013 .01 ) ; A61K 9 /2027 ( 2013 .01 ) ; A61K 31/ 192 ( 2013. 01 ) ; Related U . S . Application Data A61K 9 /2072 ( 2013 .01 ) (63 ) Continuation of application No. 16 /028 ,305 , filed on Jul. 5 , 2018 , now Pat . No . 10 , 258 ,575 , which is a (57 ) ABSTRACT continuation of application No . 15 / 173 ,596 , filed on The present disclosure provides a stable solid pharmaceuti Jun . 3 , 2016 . cal dosage form for oral administration . The dosage form (60 ) Provisional application No . 62 /313 ,092 , filed on Mar. includes a substrate that forms at least one compartment and 24 , 2016 , provisional application No . 62 / 296 , 087 , a drug content loaded into the compartment. The dosage filed on Feb . 17 , 2016 , provisional application No . form is so designed that the active pharmaceutical ingredient 62 / 170, 645 , filed on Jun . 3 , 2015 . of the drug content is released in a controlled manner. Patent Application Publication Jun . 27 , 2019 Sheet 1 of 20 US 2019 /0192440 A1 FIG . -

2021 Formulary List of Covered Prescription Drugs
2021 Formulary List of covered prescription drugs This drug list applies to all Individual HMO products and the following Small Group HMO products: Sharp Platinum 90 Performance HMO, Sharp Platinum 90 Performance HMO AI-AN, Sharp Platinum 90 Premier HMO, Sharp Platinum 90 Premier HMO AI-AN, Sharp Gold 80 Performance HMO, Sharp Gold 80 Performance HMO AI-AN, Sharp Gold 80 Premier HMO, Sharp Gold 80 Premier HMO AI-AN, Sharp Silver 70 Performance HMO, Sharp Silver 70 Performance HMO AI-AN, Sharp Silver 70 Premier HMO, Sharp Silver 70 Premier HMO AI-AN, Sharp Silver 73 Performance HMO, Sharp Silver 73 Premier HMO, Sharp Silver 87 Performance HMO, Sharp Silver 87 Premier HMO, Sharp Silver 94 Performance HMO, Sharp Silver 94 Premier HMO, Sharp Bronze 60 Performance HMO, Sharp Bronze 60 Performance HMO AI-AN, Sharp Bronze 60 Premier HDHP HMO, Sharp Bronze 60 Premier HDHP HMO AI-AN, Sharp Minimum Coverage Performance HMO, Sharp $0 Cost Share Performance HMO AI-AN, Sharp $0 Cost Share Premier HMO AI-AN, Sharp Silver 70 Off Exchange Performance HMO, Sharp Silver 70 Off Exchange Premier HMO, Sharp Performance Platinum 90 HMO 0/15 + Child Dental, Sharp Premier Platinum 90 HMO 0/20 + Child Dental, Sharp Performance Gold 80 HMO 350 /25 + Child Dental, Sharp Premier Gold 80 HMO 250/35 + Child Dental, Sharp Performance Silver 70 HMO 2250/50 + Child Dental, Sharp Premier Silver 70 HMO 2250/55 + Child Dental, Sharp Premier Silver 70 HDHP HMO 2500/20% + Child Dental, Sharp Performance Bronze 60 HMO 6300/65 + Child Dental, Sharp Premier Bronze 60 HDHP HMO -

Contraceptive Update: New Methods, New Guidelines
UCSF Essentials of Primary Care Conference Squaw Creek, CA August 8, 2019 Contraceptive Update: New Methods, New Guidelines Michael S. Policar, MD, MPH Professor Emeritus of Ob, Gyn, and Repro Sci UCSF School of Medicine [email protected] A. Every day (or moreDo You often) Use the US Medical Eligibility B. Occasionally (a few times a week) C. Rarely (a few times a month)Criteria (MEC) in Your Practice? D. Never…they don’t apply to my E. I’ve neverpractice heard of them! • Bayer: litigation consultant • Disclosures relevant to this talk Sebela Pharmaceuticals: – Investigator trainer and proctor in phase III trial of a copper IUD (VeraCept) 6% 50% 10% 17% Every day (or more often) 17% Occasionally (a few times a ... Rarely (a few times a month) Never…they don’t apply to .. I’ve never heard of them! MMWR. July 29, 2016 65 (3):1-103 On-line at: https://www.cdc.gov/mmwr/volumes/65/rr/pdfs/rr6503.pdf US Medical Eligibility Criteria Cat Definition Recommendation 1 No restriction in use Use the method 2 Advantages generally More than usual follow-up outweigh theoretical or needed proven risks 3 Theoretical or proven risks Clinical judgment that the outweigh advantages patient can use safely 4 Unacceptable health risk if the Do not use the method method is used • U.S. Selected Practice Recommendations for Contraceptive Use, 2016. MMWR July 29, 2016. 65(4);1–66 2016 Updates to the US MEC and SPR • New recommendations for women with – Cystic fibrosis – Multiple sclerosis • Interactions with SSRIs and St. -

Preventive Care Services: Contraception
Preventive Care Services: Contraception Preventive Care Coverage at No Cost to You Effective Jan. 1, 2021 Your health plan may provide certain contraceptive coverage as a benefit of membership, at no cost to you when you use a pharmacy or doctor in your health plan's network. There is no copay, deductible or coinsurance, even if your deductible or out-of-pocket maximum has not been met. Coverage for contraceptives can vary depending on the type of plan you are enrolled in, as well as your prescription drug list. If you are using a contraceptive not listed under the Contraceptive Product Coverage, then copays, coinsurance or deductible may apply. Check your drug list or call the number listed on your member ID card to find out what products are covered at no cost share under your plan. Contraception* The following contraceptive items and services may be covered under the medical or pharmacy benefit without cost-sharing when provided by a pharmacy or doctor in your health plan's network. This list is not all inclusive. Additional products may be covered at no additional cost. • One or more prescribed products within each of the categories approved by the FDA for use as a method of contraception • FDA-approved contraceptives available over the counter (i.e. foam, sponge, female condoms), when prescribed by a physician • The morning after pill • Injections such as IM DEPO-PROVERA and DEPO-SUBQ PROVERA 104 may be covered under the medical or pharmacy benefit • Medical devices such as diaphragms, cervical caps and contraceptive implants may -
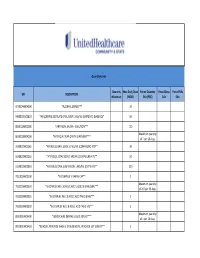
UHC PA Community and State Quantity Limit List
Quantity Limits Quantity Max Daily Dose Period Quantity Period Days Period Fills GPI DESCRIPTION Maximum (MDD) Edit (PQE) Edit Edit 97703040004300 *ALCOHOL SWABS*** 10 34000003101810 *AMLODIPINE BESYLATE ORAL SUSP 1 MG/ML (CMPD KIT) (BASE EQ)* 10 88501000002000 *ARTIFICIAL SALIVA - SOLUTION*** 120 Maximum quantity 86202000004200 *ARTIFICIAL TEAR OPHTH OINTMENT*** of 7 per 26 days. 33200020002065 *ATENOLOL ORAL SOLN 10 MG/ML (COMPOUND KIT)** 20 33200020002055 *ATENOLOL ORAL SOLN 2 MG/ML (COMPOUND KIT)** 50 33200020001810 *ATENOLOL ORAL SUSPENSION 1 MG/ML (CMPD KIT)** 200 78110000000100 *B-COMPLEX VITAMIN CAP** 1 Maximum quantity 78133000000920 *B-COMPLEX W/ C & FOLIC ACID LIQUID 0.9 MG/5ML*** of 237 per 26 days. 78133000000325 *B-COMPLEX W/ C & FOLIC ACID TAB 0.8 MG*** 1 78133000000330 *B-COMPLEX W/ C & FOLIC ACID TAB 1 MG*** 1 Maximum quantity 88350010006400 *BENZOCAINE DENTAL LIQUID 20% KIT*** of 1 per 26 days. 90050010006410 *BENZOYL PEROXIDE WASH 2.5% & BENZOYL PEROXIDE LOT 10% KIT** 1 47300005100100 *BIFIDOBACTERIUM BIFIDUM CAP** 2 97202007100900 *BLOOD GLUCOSE CALIBRATION - LIQUID*** 0.04 Maximum quantity 97202011006200 *BLOOD GLUCOSE METER DISPOSABLE DEVICE WITH TEST STRIPS*** of 1 per 999 days. Maximum quantity 97202010006200 *BLOOD GLUCOSE MONITORING DEVICES*** of 1 per 365 days. Maximum quantity 97202010006410 *BLOOD GLUCOSE MONITORING KIT W/ DEVICE*** of 1 per 365 days. Maximum quantity 97202010006400 *BLOOD GLUCOSE MONITORING KIT*** of 1 per 365 days. Maximum quantity 97750010006200 *BLOOD PRESSURE MONITORING - DEVICE*** of 1 per 999 days. Maximum quantity 9025990212B120 *CALCIPOTRIENE CR 0.005% & DIMETHICONE CR 5% THERAPY PACK*** of 1 per 26 days. 79109903450340 *CALCIUM CARB-VIT D W/ MINERALS TABS 600 MG-200 UNIT*** 5 79109903450355 *CALCIUM CARB-VIT D W/ MINERALS TABS 600 MG-800 UNIT*** 2 Maximum quantity 6610990420B120 *CELECOXIB CAP 200 MG & METH SAL-MEN-CAPSAICIN LIQD THER PK* of 1 per 26 days. -

Orange Book Cumulative Supplement 08 August 2019
CUMULATIVE SUPPLEMENT 8 AUGUST 2019 APPROVED DRUG PRODUCTS WITH THERAPEUTIC EQUIVALENCE EVALUATIONS 39th EDITION Department of Health and Human Services Food and Drug Administration Office of Medical Products and Tobacco Center for Drug Evaluation and Research Office of Generic Drugs Office of Generic Drug Policy 2019 Prepared By Food and Drug Administration Office of Medical Products and Tobacco Center for Drug Evaluation and Research Office of Generic Drugs Office of Generic Drug Policy APPROVED DRUG PRODUCTS with THERAPEUTIC EQUIVALENCE EVALUATIONS 39th EDITION Cumulative Supplement 8 August 2019 CONTENTS PAGE 1.0 INTRODUCTION ......................................................................................................................................... v 1.1 How to use the Cumulative Supplement ............................................................................................ v 1.2 Cumulative Supplement Content ...................................................................................................... vi 1.3 Applicant Name Changes ................................................................................................................ vii 1.4 Levothyroxine Sodium....................................................................................................................... ix 1.5 Availability of the Edition .................................................................................................................... x 1.6 Report of Counts for the Prescription Drug Product List .................................................................. -

(12) United States Patent (10) Patent No.: US 8,158,152 B2 Palepu (45) Date of Patent: Apr
US008158152B2 (12) United States Patent (10) Patent No.: US 8,158,152 B2 Palepu (45) Date of Patent: Apr. 17, 2012 (54) LYOPHILIZATION PROCESS AND 6,884,422 B1 4/2005 Liu et al. PRODUCTS OBTANED THEREBY 6,900, 184 B2 5/2005 Cohen et al. 2002fOO 10357 A1 1/2002 Stogniew etal. 2002/009 1270 A1 7, 2002 Wu et al. (75) Inventor: Nageswara R. Palepu. Mill Creek, WA 2002/0143038 A1 10/2002 Bandyopadhyay et al. (US) 2002fO155097 A1 10, 2002 Te 2003, OO68416 A1 4/2003 Burgess et al. 2003/0077321 A1 4/2003 Kiel et al. (73) Assignee: SciDose LLC, Amherst, MA (US) 2003, OO82236 A1 5/2003 Mathiowitz et al. 2003/0096378 A1 5/2003 Qiu et al. (*) Notice: Subject to any disclaimer, the term of this 2003/OO96797 A1 5/2003 Stogniew et al. patent is extended or adjusted under 35 2003.01.1331.6 A1 6/2003 Kaisheva et al. U.S.C. 154(b) by 1560 days. 2003. O191157 A1 10, 2003 Doen 2003/0202978 A1 10, 2003 Maa et al. 2003/0211042 A1 11/2003 Evans (21) Appl. No.: 11/282,507 2003/0229027 A1 12/2003 Eissens et al. 2004.0005351 A1 1/2004 Kwon (22) Filed: Nov. 18, 2005 2004/0042971 A1 3/2004 Truong-Le et al. 2004/0042972 A1 3/2004 Truong-Le et al. (65) Prior Publication Data 2004.0043042 A1 3/2004 Johnson et al. 2004/OO57927 A1 3/2004 Warne et al. US 2007/O116729 A1 May 24, 2007 2004, OO63792 A1 4/2004 Khera et al. -

UNITED STATES SECURITIES and EXCHANGE COMMISSION Washington, D.C
UNITED STATES SECURITIES AND EXCHANGE COMMISSION Washington, D.C. 20549 FORM 8-K CURRENT REPORT Pursuant to Section 13 or 15(d) of the Securities Exchange Act of 1934 Date of Report (date of earliest event reported): January 13, 2021 TherapeuticsMD, Inc. (Exact Name of Registrant as Specified in Its Charter) Nevada 001-00100 87-0233535 (State or Other Jurisdiction (Commission (IRS Employer of Incorporation) File Number) Identification No.) 951 Yamato Road, Suite 220 Boca Raton, FL 33431 (Address of principal executive office) (zip code) Registrant’s telephone number,including area code: (561) 961-1900 Not Applicable (Former name or former address, if changed since last report.) Check the appropriate box below if the Form 8-K filing is intended to simultaneously satisfy the filing obligation of the registrant under any of the following provisions: ☐ Written communications pursuant to Rule 425 under the Securities Act (17 CFR 230.425) ☐ Soliciting material pursuant to Rule 14a-12 under the Exchange Act (17 CFR 240.14a-12) ☐ Pre-commencement communications pursuant to Rule 14d-2(b) under the Exchange Act (17 CFR 240.14d-2(b)) ☐ Pre-commencement communications pursuant to Rule 13e-4(c) under the Exchange Act (17 CFR 240.13e-4(c)) Securities registered pursuant to Section 12(b) of the Act: Trading Name of each exchange Title of each class Symbol(s) on which registered Common Stock, par value $0.001 per share TXMD The Nasdaq Stock Market LLC Indicate by check mark whether the registrant is an emerging growth company as defined in Rule 405 of the Securities Act of 1933 (§230.405 of this chapter) or Rule 12b-2 of the Securities Exchange Act of 1934 (§240.12b-2 of this chapter).