PHHPC June 10, 2011 Exhibits
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Foreign Service Journal, February 1958
FEBRUARY 1958 The AMERICAN FOREIQN SERVICE PROTECTIVE ASSOCIATION Copies of the Protective Association booklet “Croup Insurance Program—June, 1957” are available at: Protective Association office, 1908 C Street, N.W., Washington, D.C. Foreign Service Lounge, 513, 801 - 19.h Street, N.W., Washington, D.C. Foreign Service Institute, Jefferson-Tyler Bldg., 1018 Wilson Blvd., Arlington, Va. Administrative Offices at foreign posts. This group insurance program may meet your needs. It is worth your study. The Protec¬ tive Association plan is one of the most liberal of such plans in the United States. Members are receiving benefits in various claims at a present rate of more than two hundred thousand dollars annually. The plan: Provides a valuable estate for your dependents in the event of your death. Protects you and your eligible dependents against medical and surgical expenses that might be a serious drain on your finances. Includes accidental death and dismemberment insurance. Entitles members and their eligible dependents to over-age-65 insurance, under the pertinent rules and regulations of the Protective Association. Personnel eligible to participate in the plan are: Foreign Service Officers, Department of State. Foreign Service Staff, Department of State. Foreign Service Reserve Officers, Department of State, when on active service. Permanent American employees of the Foreign Service of the Department of State. ICA (Department of State) Officers, when on active service abroad. ♦ Address applications and inquiries to: THE AMERICAN FOREIGN SERVICE PROTECTIVE ASSOCIATION c/o Department of State, Washington 25, D.C., or 1908 G Street, N.W., Washington 6, D.C. Whew—Fait Accompli! WE'VE MOVED TO OUR NEW BUILDING (WITH PARKING LOT) 600 S. -
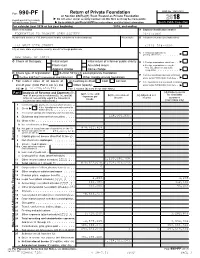
FPOS-2018-Form-990.Pdf
OMB No. 1545-0052 Form 990-PF Return of Private Foundation I or Section 4947(a)(1) Trust Treated as Private Foundation À¾µ¼ Do not enter social security numbers on this form as it may be made public. Department of the Treasury I Internal Revenue Service Go to www.irs.gov/Form990PF for instructions and the latest information. Open to Public Inspection For calendar year 2018 or tax year beginning , 2018, and ending , 20 Name of foundation A Employer identification number FOUNDATION TO PROMOTE OPEN SOCIETY 26-3753801 Number and street (or P.O. box number if mail is not delivered to street address) Room/suite B Telephone number (see instructions) 224 WEST 57TH STREET (212) 548-0600 City or town, state or province, country, and ZIP or foreign postal code C If exemption applicatmionm ism m m m m m I pending, check here NEW YORK, NY 10019 m m I G Check all that apply: Initial return Initial return of a former public charity D 1. Foreign organizations, check here Final return Amended return 2. Foreign organizations meeting the 85% test, checkm hem rem anmd am ttamchm m m I Address change Name change computation H Check type of organization: X Section 501(c)(3) exempt private foundation E If private foundation status was terminamtedI Section 4947(a)(1) nonexempt charitable trust Other taxable private foundation under section 507(b)(1)(A), check here I Fair market value of all assets at J Accounting method: Cash X Accrual F If the foundation is in a 60-month terminmatIion end of year (from Part II, col. -

New York Citytm
The Internationalist ® The Top 10 Guide to New York The Top 10 Guide to New York CityTM The Internationalist 96 Walter Street/Suite 200 Boston, MA 02131 USA The Internationalist • www.internationalist.com • 617-354-7755 1 The Internationalist ® The Top 10 Guide to New York The Internationalist® International Business, Investment and Travel Published by: The Internationalist Publishing Company 96 Walter Street/Suite 200 Boston, MA 02131, USA Tel: 617-354-7722 [email protected] Author: Patrick W. Nee Copyright © 2001 by PWN The Internationalist is a Registered Trademark. The Top 10 Guide to New York City, The Top 10 Travel Guides, The Top 10 Guides are Trademarks of the Internationalist Publishing Company. All right are reserved under International, Pan-American and Pan-Asian Conventions. No part of this book, no lists, no maps or illustration may be reproduced in any form without the written permission of the publisher. All rights vigorously enforced. ISBN: 1-891382-21-7 Special Sales: Books of the Internationalist Publishing Company are available for bulk purchases at special discounts for sales promotions, corporate identity programs or premiums. The Internationalist Publishing Company publishes books on international business, investment and travel. For further information contact the Special Sales department at: Special Sales, The Internationalist, 96 Walter Street/Suite 200, Boston, MA 02131. The Internationalist Publishing Company 96 Walter Street/Suite 200 Boston, MA 02131 USA Tel: 617-354-7722 [email protected] e-mail: [email protected] web site: http://www.internationalist.com The Internationalist • www.internationalist.com • 617-354-7755 2 The Internationalist ® The Top 10 Guide to New York Welcome to New York City. -

HANDPICKED July 30-August 4 • Blue Note
WWW.JAZZINSIDEMAGAZINE.COM AUGUST 2013 Interviews Andrew Cyrille David Chesky Satoko Fujii Francisco Mela Dizzy’s Club, August 19 Roy Hargrove Big Band Blue Note, August 20-25 Marcus Strickland EARL Jazz Standard, August 13-14 Comprehensive Directory of NY Club Concert KLUGH & Event Listings HANDPICKED E view Section! July 30-August 4 • Blue Note xpanded CD Re The Jazz Music Dashboard — Smart Listening Experiences www.ConcordMusicGroup.com www.Chesky.com www.WhalingCitySound.com www.SatokoFujii.com The Stone August 20-25 Like Us facebook.com/JazzInsideMedia Follow Us twitter.com/JazzInsideMag Watch Us youtube.com/JazzInsideMedia TJC14_Ad_Jazz Inside.pdf 1 4/26/13 5:31 PM 13TH ANNUAL SAILING OF THE JAZZ CRUISE WHERE EVERY PERFORMANCE IS SPECIAL Ernie Adams Tony Kadleck John Allred Tom Kennedy Shelly Berg Joe LaBarbera MUSIC DIRECTOR Christoph Luty Alonzo Bodden COMEDIAN Dennis Mackrel Randy Brecker Manhattan Transfer Ann Hampton Callaway Marcus Miller Quartet Quartet Bill Charlap Trio Bob Mintzer Clayton Brothers Lewis Nash Trio Quintet Dick Oatts C Freddy Cole Trio M Ken Peplowski Kurt Elling Quartet SHOW HOST Y Robin Eubanks Houston Person CM Quartet John Fedchock MY BIG BAND DIRECTOR John Pizzarelli CY Quartet JAN. 26-FEB. 2 David Finck Gregory Porter Quartet CMY Chuck Findley 2014 K Poncho Sanchez Bruce Forman Arturo Sandoval Nnenna Freelon Trio Gary Smulyan Wycliffe Gordon GOSPEL SHOW HOST Cedar Walton Trio Jimmy Greene Jennifer Wharton Jeff Hamilton Niki Haris Antonio Hart Tamir Hendelman Dick Hyman Tommy Igoe Sextet Sean Jones TO L L -FREE US & C ANADA FT LAUDERDALE • TURKS & CAICOS • SAN JUAN 888.852.9987 ST. -

229 Hot Places to Run Your Classified Ad Classified Advertising Is a Proven Method
THE FPA GUIDE AND 229 HOT PLACES TO RUN YOUR CLASSIFIED AD CLASSIFIED ADVERTISING IS A PROVEN METHOD The FPA Guide is book of companies that have products or services for sale to the federal government. Classified advertising has always been, and will continue to be the favorite method for Mail Order "Pros" to advertise. Almost all Mail Order Pros started with these tiny inexpensive ads since they represent the best cost effective way to reach millions of people. But, smart small business owners that selling to the federal government is one of the most profitable ways to get business coming in the door. It can be difficult to learn how to get contracts with the federal government, but the FPA Guide is the answer to all that messy paperwork. It's s common misconception that all government jobs have to go to the lowest bidder, but that's not entirely accurate. You see, when a government agency needs to procure a product or service under a certain amount of money, their procurement specialists turn to the FPA Guide, a handbook of companies that advertise their products in services within. It's much easier than trying to find and fill out all the paperwork. TWO BASIC METHODS Two basic methods are used with classified advertising. (1) Place an ad offering FREE literature, and then send your literature to all inquiries. A "free" offer will always out pull an ad that requests money, but your overall profits may be larger since you will generate more inquiries. This method is excellent when you are also collecting "Opportunity Seeker" names that you can rent. -

Fuel Oils (Fourth Edition)
CS12-38 Oils, Fuel UNITED STATES DEPARTMENT OF COMMERCE DANIEL C. ROPER, Secretary NATIONAL BUREAU OF STANDARDS LYMAN J. BRIGGS, Director Bureau of Standards AUG 2 9 1933 FUEL OILS (FOURTH EDITION) COMMERCIAL STANDARD CS12-38 (Supersedes CS12-35) Effective Date for New Production, May 31, 1938 A RECORDED STANDARD OF THE INDUSTRY UNITED STATES GOVERNMENT PRINTING OFFICE WASHINGTON : 1938 For sale by the Superintendent of Documents, Washington, D. C. Price 5 cents U. S. Department of Commerce National Bureau of Standards PROMULGATION of COMMERCIAL STANDARD CS12-38 for FUEL OILS (Foufth Edition) On January 9, 1929, a joint conference of representative refiners, distributors, and consumers of fuel oil, manufacturers of oil burners, and general interests adopted a recommended standard for domestic and industrial fuel oils, which was accepted in writing by the industry and published as Commercial Standard CS12-29. In 1933, and again in 1934, upon recommendation of the standing committee to keep the standard abreast of progress, revisions were adopted and issued as CS 12-33 and CS 12-35, respectively. On February 25, 1938, at the recommendation of the standing com- mittee, a revision of CS12-35, drafted by Technical Committee E of American Society for Testing Materials Committee D-2, was cir- culated for acceptance. The industry has since accepted and ap- proved for promulgation by the United States Department of Com- merce, through the National Bureau of Standards, the revised standard as shown herein. The standard became effective for new production on May 31, 1938, subject to the expiration of the then existing contracts. -
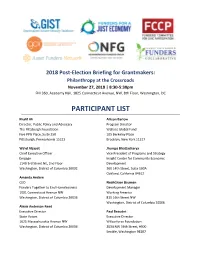
Participant List
2018 Post-Election Briefing for Grantmakers: Philanthropy at the Crossroads November 27, 2018 | 8:30-5:30pm FHI 360, Academy Hall, 1825 Connecticut Avenue, NW, 8th Floor, Washington, DC PARTICIPANT LIST Khalif Ali Allison Barlow Director, Public Policy and Advocacy Program Director The Pittsburgh Foundation Wallace Global Fund Five PPG Place, Suite 250 105 Berkeley Place Pittsburgh, Pennsylvania 15222 Brooklyn, New York 11217 Wa'el Alzayat Jhumpa Bhattacharya Chief Executive Officer Vice President of Programs and Strategy Emgage Insight Center for Community Economic 1140 3rd Street NE, 2nd Floor Development Washington, District of Columbia 20002 360 14th Street, Suite 500A Oakland, California 94612 Amanda Andere CEO NoahGrace Bauman Funders Together to End Homelessness Development Manager 1001 Connecticut Avenue NW Working America Washington, District of Columbia 20036 815 16th Street NW Washington, District of Columbia 20006 Alexis Anderson-Reed Executive Director Paul Beaudet State Voices Executive Director 1625 Massachusetts Avenue NW Wilburforce Foundation Washington, District of Columbia 20036 2034 NW 56th Street, #300 Seattle, Washington 98107 Noah Berger Shona Chakravartty Director, Policy Reform and Advocacy Senior Program Officer The Annie E. Casey Foundation Hill-Snowdon Foundation 503 N. Charles Street 1250 Connecticut Avenue NW Baltimore, Maryland 21201 Washington, District of Columbia 20036 Sayu Bhojwani Peggy Chang Founder and President Program Associate New American Leaders Heising-Simons Foundation 25 West 39th Street, 14th Floor 400 Main Street, Suite 200 New York, New York 10018 Los Altos, California 94022 Jocelyn Bissonnette Heather Lane Chauny Director, Funders Census Initiative Strategy Advisor Funders' Committee for Civic Participation FHI Foundation 1524 S. IH-35, Suite 330 1825 Connecticut Avenue NW Austin, Texas 78704 Washington, District of Columbia 20009 Shelley Waters Boots George Cheung Senior Consultant Program Director The Annie E. -

21 -27, 1942 SUPERVISING EDITOR: Carl A
E7 MOVIE-RADIO FIFTEEN CENTS PROGRAMS FOR ilfiriair 0rt 1 l.l 1 7 390 I a8W`fa IS Pd I 7 r`! 3 0! ?:311S j 1H-91NO r 51 f.Hb7Z/.SO FANNY ( "Snooks' ') BRICE and i HANLEY ( "Daddy ") STAFFORD Thanxgivin' Letter to Daddy GV E See page 1 U9urtbN C eaf Looks at 111 photo -Story: "My Friend Flicka" Winners of Name Lum and Abner's Baby Contest Thanksgiving Litany- 1942 IN THIS momentous year of 1942, we morning when a smile is needed most I must, as individuals and as a nation, -I THANK THEE, GOD! search deep within our souls and the For the firm belief that. America's great heart of America to know and homes are America's future family truly realize the blessings -a that are still of my work when ours in a world torn by war. own to for -so that We cannot bring back those brave victory comes they may reap the har- men who have given their lives in the vest of freedom -1 THANK THEE, cause of freedom for all peoples. Nor GOD! ' can we lessen the grief of their loved For men of vision to lead us -for the ones as they gather round their Thanks- butcher boy, the druggist, the lawyer, giving tables this the clerk, who are year and bravely try now Uncle Sam's sol- to carry on in the diers, sailors, marines face of heartbreak. and pilots -for the 1111k But on this one truly American holi- production workers, GLAMOROUS GUN -MAKERS greet the OI' Maestro at a Toronto day-Thanksgiving- the nurses, the Waves plant turning out arms for the allies. -

American Federation of Musicians: Survey Results
Changing the Beat A Study of the Worklife of Jazz Musicians VOLUME II: AMERICAN FEDERATION OF MUSICIANS: SURVEY RESULTS A Study by Joan Jeffri NATIONAL ENDOWMENT FOR THE ARTS NEA Research Division Report #43 ADVISORY COMMITTEE SPONSORS AND FUNDERS Dr. Billy Taylor, Chairman The National Endowment for the Arts The David and Lucile Packard Foundation David Baker Alvin Batiste The Grammy Foundation Jessie Bermudez Tom Carter American Federation of Musicians Geraldine DeHass Jon Faddis American Federation of Musicians Local 802 Delfayeo Marsalis Dan Morgenstern New Orleans Jazz & Heritage Foundation Jimmy Owens Patrice Rushen The Nathan Cummings Foundation i Project Director: Joan Jeffri, Director, Research Center for Arts and Culture Teachers College Columbia University Consultants: Dr. Douglas Heckathorn, Cornell University Dr. Robert Greenblatt Project coordinators: Adina Williams Phillip Harvey Project researchers: Judith Hellman Janine Okmin Data consultants: Oscar Torres Judith Rosenstein City Coordinators: Detroit Dr. Bernard Brock Dr. David Magidson Center for the Study of Art and Public Policy Wayne State University New Orleans Philip Dobard, Director Graduate Program in Arts Administration University of New Orleans New York Dr. Martin Mueller, Director Jazz and Contemporary Music Program New School University San Francisco Dr. Dee Spencer, Director of Education SF Jazz Organization San Francisco State University Library of Congress info here from Executive Summary Cover: Copyright of Photo ii Table of Contents Introduction 1 Purpose 1 Findings 2 Survey Background and Method 2 Organization of Report 3 Chapter I. Demographics 4 Chapter II. Employment and Income 6 Chapter III. Other Issues 14 Chapter IV. Summary and Conclusions 32 Appendices A. Metropolitan Areas Used in the Study 34 B. -
Judge Rules Against Captiva Convention Hotel
|—INDEX- furis & Leisure 5B At Larqe 5A Calendar 4B Classifieds 7Q Cfty&ide 11A Commentary SA Panther power Mother's Day Crossword 7<? Environment 3G Islanders shine Youngsters Pollrie Beat 2A Recreation SB on successful make plans for Remember When 4A Cypress Lake unit mom's holiday 5A 1961-1990 Still first on Sanibel and Captiva VOL. 29, NO. 19 TUESDAY, MAY 8, 1990 THREE SECTIONS, 44 PAGES 50 CENTS Captiva deputy's house dedicated By Steve Ruediger Islander staff writer A large number of Captiva residents, Lee County officials and sheriffs department officials were on hand Monday for the dedication of the sheriffs deputy's residence on Captiva. "I wish to thank everybody for giving me the opportunity to do this job up here," said Deputy Rory VanDeusen at the dedication ceremony. He and his wife, Joyce, and their seven-month-old son, Scott, plan to move in this Thursday. Also on hand for the dedication was Miriam Johnson, who had previously lived in the house with her late husband, Belton Johnson. She told the crowd that when she was preparing to move out she had hoped the house would not be destroyed and could be put to a good use. That is why she donated it to the Captiva Civic Association. "All this is in answer to a prayer," said Mrs. Johnson, 'The house meant so much to us." She said she was glad that a fine young couple were moving into it and "I hope they will be as happy and as blessed in this house as Belton and I were." The house was moved last year from its old location on Captiva Drive near 'Tween Waters to its new location Please see HOUSE, page 13A A number of officials participated in the ribbon cutting ceremony at the new deputy's house. -

Manhattan Office Market
Manhattan Offi ce Market 2 ND QUARTER 2015 REPORT A NEWS RECAP AND MARKET SNAPSHOT Pictured: 1001 Avenue of the Americas Looking Ahead Partnership for New York City: New York’s Future as the World Financial Capital The report released in June concluded that while New York City remains the preferred location of global fi nancial companies to establish their headquarters, there is a growing trend to relocate jobs and business operations to lower cost, more business-friendly locations that are beyond the city’s border. A comprehensive survey was conducted in collaboration with Gerson Lehrman Group (GRG), intending to better understand how the fi nancial industry is evolving; and what measures are required to solidify New York’s competitive advantage as a global fi nancial center. Collected data represents an overview of the responses from 50-fi rm respondents that included large banks, insurance companies and asset managers, private equity fi rms, hedge funds, and fi nancial technology (FinTech) startups; and represent about 1/3rd of the total industry employment in the city. Additionally, observations were included from 8-real estate fi rms that were surveyed; along with interviews from other related experts in the fi eld. Financial Industry – an economic snapshot • Contributes 20% of the city’s economic output, representing twice that of the next top-grossing industry. • Accounts for nearly 1/3rd of the city’s private sector payroll, despite accounting for only 8%, or about 310,000 of the city’s private sector jobs in 2013; of which 23,000 jobs are high-technology in the areas of software, data processing and network management. -

Beloved Community Strengthening the Field of Black Male Achievement May 2014
BUILDING A BELOVED COMMUNITY STRENGTHENING THE FIELD OF BLACK MALE ACHIEVEMENT MAY 2014 FOREWORD BY LUCY BERNHOLZ | AFTERWORD BY GEOFFREY CANADA AUTHORS & CONTRIBUTORS AUTHORS Seema Shah Director of Research for Special Projects Grace Sato Research Associate CONTRIBUTORS Anjula Duggal Vice President for Marketing and Communications Christine Innamorato Production Manager Larry McGill Vice President for Research Sarah Reibstein Research Assistant Vanessa Schnaidt Director of Communications ABOUT THE FOUNDATION CENTER ACKNOWLEDGEMENTS Established in 1956, the Foundation Center is the The authors acknowledge the generous support leading source of information about philanthropy of the Open Society Foundations’ Campaign worldwide. Through data, analysis, and training, for Black Male Achievement for funding for it connects people who want to change the this work. Special thanks to Shawn Dove, world to the resources they need to succeed. rashid shabazz, Anand Dholakia, Marcus Littles, The Center maintains the most comprehensive Marc Philpart, and Andrew Wolk, who reviewed database on U.S. and, increasingly, global drafts and provided thoughtful and constructive grantmakers and their grants—a robust, feedback. We also thank Robert Wood Johnson accessible knowledge bank for the sector. Foundation and Frontline Solutions for use of It also operates research, education, and training photos from the Under Construction project, programs designed to advance knowledge of as well as Eagle Academy Foundation and Urban philanthropy at every level. Thousands of people Prep Academies for their photo contributions. visit the Center’s web site each day and are served in its five library/learning centers and at more than 470 Funding Information Network locations nationwide and around the world.