Antibacterial and Cellular Behaviors of Novel Zinc-Doped Hydroxyapatite/Graphene Nanocomposite for Bone Tissue Engineering
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
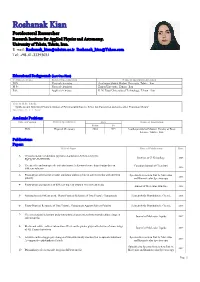
Roshanak Kian Postdoctoral Researcher Research Institute for Applied Physics and Astronomy, University of Tabriz, Tabriz, Iran
Roshanak Kian Postdoctoral Researcher Research Institute for Applied Physics and Astronomy, University of Tabriz, Tabriz, Iran. E-mail: [email protected], [email protected] Tel: +98-41-33393031 Educational Background: (Last One First) Certificate Degree Field of Specialization Name of Institution Attended PhD Physical chemistry Azarbaijan Shahid Madani University, Tabriz - Iran M.Sc. Physical chemistry Zanjan University, Zanjan - Iran B.Sc. Applied chemistry K. N. Toosi University of Technology, Tehran - Iran Title of M.Sc. Thesis: “ Synthesis and Structural Characterization of Pyridinocalix(4)arene Silver Ion Complexes and some other Transition Metals” Supervisors: Dr. A. A. Torabi Academic Positions: Title of Position Field of Specialization Date Name of Institution From To PhD Physical Chemistry 2010 2015 Azarbaijan Shahid Madani- Faculty of Basic Science, Tabriz - Iran. Publications: Papers: Title of Paper Place of Publication Date 1- Crystal structure of dichloro (pyridine-2-aldoxime-N,N)mercury(II): JOURNAL OF Z. Kristallogr 2005 HgCl2(NC5H4CHNOH) 2- The specific and non-specific solvatochromic behavior of some diazo Sudan dyes in Canadian Journal of Chemistry 2015 different solvents 3- Photo-physical behavior of some antitumor anthracycline in solvent media with different Spectrochimica Acta Part A: Molecular 2014 polarity and Biomolecular Spectroscopy 4- Photo-physical properties of different types of vitamin A in solvent media Journal of Molecular Structure 2015 5- Solvatochromic Effects on the Photo-Physical -

Culturetalk Iran Video Transcripts: Azerbaijan Museum
CultureTalk Iran Video Transcripts: http://langmedia.fivecolleges.edu Azerbaijan Museum Persian transcript: نگار: ھَمين کﻻً تو اين قِ َسمت َمرکزی َشھر َوقتی پياده َروی کنی خيلی ساختِ ِمونھای[ساختمان ِھای ] قديمی می بينی که مثﻻً تبديل شدند حاﻻ...حاﻻ يه اِ ِستفاده ای دارند اَ َزش[ َاز آن] می حکنند َولی در ِعين ال موزه است و موزه ِی موزه ِی تبريز موزه ِی َآذربايجانه[ َآذربايجان است] اِ ِسمش. تو ھَمين ميدون[ميدان] َشھرداری تبريز يه کم باﻻتر از اون واقِع شده که ديگه َمثﻻً... محسن: موزه ِی َآذربايجان نگار: آره، ِ ِاسمش موزه ِی آذربايجانه . محسن: َيعنی چه چيزای[ ِچيزھای] ﱢخاصی تو اونجا[آنجا] ِنگه داری می شه[می شود] شما [ که می دانيد]. نگار: من خيلی ساﻻی[سال ھای] پيش رفتم ولی خب ِتوی... دو َ َ طبقه داره توی ََطبقه ِی باﻻش[ ِباﻻی آن] ُکﻻً َمثﻻً َ ّاوﻻً يه ِ سری يه ِسری چيزايی[چيزھايی] که َسنگايی[سنگ ھايی] که نوشته ھايی حاﻻ ھر چی... ُظروفی که از َ ّحفاری َ ِ ِمسجد کبود که... َ ِ ِمسجد کبود َدقيقاً َ َِبغل موزه ِی َآذربايجان ِواقع شده و اونجا ُکﻻً يه ِ َ قسمتی َمثﻻً ُ ِحدود بگم[بگويم] پنج شيش سال پيش يه ِ َقسمتی اونجا کشف کردند که َ َفھميدند که اين ِ َِقدمت خيلی چند ساله داشته زير خاک ُ ّکلی چيز پيدا کردند ُ ّکلی ِ ِ ِاسکلت َآدما[آدم ھا] رو[را] پيدا کردند ُ ّکلی َمثﻻً َھمين َظرفا َ ِانواع چيزا[چيزھا]. ُمحسن: َظرف ھا و ِ ِسکه ھا . نگار: اين ھا را پيدا کردند که َاصﻻً ُ ّکلی ُ َکمک کرد به ِ َ ِشناختن ِتاريخ اون ِ َقسمت. -

A Short Glimpse to the Urban Development of Tabriz During the History * Ph.D Candidate
Journal Of Contemporary Urban Affairs 2019, Volume 3, Number 1, pages 73– 83 A Short Glimpse to the Urban Development of Tabriz During the History * Ph.D Candidate. NARMIN BABAZADEH ASBAGH Faculty of Architecture, Eastern Mediterranean University, Famagusta, Turkey E-mail: [email protected] A B S T R A C T A R T I C L E I N F O: Article history: Locating on North West of Iran, Tabriz, the capital of East Azerbaijan Province, Received 03 September 2018 is one of the important metropolises of the country. The foundation of this Accepted 08 October 2018 Available online 26 October historic city dated back to 1500 B.C. but due to the severe earthquakes, few 2018 historic buildings remained from ancient eras. In 2012, Tabriz was selected as the most beautiful city of Iran, and it is nominated as the tourism capital of Keywords: Islamic countries in 2018. Tabriz used to be the capital of Iran during different Tabriz; dynasties like Ilkhanid, Kara Koyunlu, Ak Koyunlu, and Safavid; it was the Iran; Urban Development; residence of the royal family and crown prince during the Qajar Dynasty Qajar Dynasty; period. Tabriz is famous as “the city of the firsts”; and the Historic Bazaar Rapid Urban Growth. Complex of Tabriz is the biggest roofed bazaar in the world, inscribed as a World Heritage Site in 2010. Tabriz experiences the phenomenon of rapid urban growth causing the formation of slum settlements in the border zones of the city. This paper will briefly discuss the urban development of Tabriz during the history. -

Shahriyar: Shahriyar and “Sahandim”
Khazar Journal of Humanities and Social Sciences Volume 20 № 3 2017, 126-145 © Khazar University Press 2017 DOI: 10.5782/2223-2621.2017.20.3.126 Poetry Customs and Traditions of Shahriyar: Shahriyar and “Sahandim” Esmira Fuad (Shukurova) Institute of Literature named after Nizami Ganjavi, Azerbaijan National Academy of Science Introduction Regardless of any poetry model, in which the poetic thought is expressed, the poet is always his own time and century’s voice, its conscience, friend of his people, the protector of people who live frankly, not enticed of the world blessing and a heart, who speaks only the truth pertaining to his period, its wishes and intentions. One of the bearers of these passionate hearts is Doctor Seyid Mahammadhuseyn Behjat Tebrizi Shahriyar… Who is Shahriyar? Shahriyar is the most powerful representative of Iran and Azerbaijani poetry of 20-th century, the classical poet and art genius estimated as Hafizi-sani and Sadi of his time. He was born in Tabriz city on March 21, 1905, in spring. Haji Miraga Khoshginabi Musavi, the poet’s father was a well-known lawyer in Tabriz and his mother Kovkab khanim was a housewife. Haji Miraga, who has enjoyed universal esteem of his people, known as jack-of-all-trades, holding in high respect amongst the friends, at the same time being a protector of needy families and men was known as a personality taking care of truth. Shahriyar lived in the Southern Azerbaijan, Iran, during some stages of the 20-th century which was characterized by severe class struggles and social-political fights for the national freedom, cultural progress. -

Article a Catalog of Iranian Prostigmatic Mites of Superfamilies
Persian Journal of Acarology, Vol. 2, No. 3, pp. 389–474. Article A catalog of Iranian prostigmatic mites of superfamilies Raphignathoidea & Tetranychoidea (Acari) Gholamreza Beyzavi1*, Edward A. Ueckermann2 & 3, Farid Faraji4 & Hadi Ostovan1 1 Department of Entomology, Science and Research Branch, Islamic Azad University, Fars, Iran; E-mail: [email protected] 2 ARC-Plant Protection Research Institute, Private bag X123, Queenswood, Pretoria, 0121, South Africa; E-mail: [email protected] 3 School of Environmental Sciences and Development, Zoology, North-West University- Potchefstroom Campus, Potchefstroom, 2520, South Africa 4 MITOX Consultants, P. O. Box 92260, 1090 AG Amsterdam, The Netherlands * Corresponding author Abstract This catalog comprises 56 genera and 266 species of mite names of superfamilies Raphignathoidea and Tetranychoidea recorded from Iran at the end of January, 2013. Data on the mite distributions and habitats based on the published information are included. Remarks about the incorrect reports and nomen nudum species are also presented. Key words: Checklist, mite, habitat, distribution, Iran. Introduction Apparently the first checklist about mites of Iran was that of Farahbakhsh in 1961. Subsequently the following lists were published: “The 20 years researches of Acarology in Iran, List of agricultural pests and their natural enemies in Iran, A catalog of mites and ticks (Acari) of Iran and Injurious mites of agricultural crops in Iran” are four main works (Sepasgosarian 1977; Modarres Awal 1997; Kamali et al. 2001; Khanjani & Haddad Irani-Nejad 2006). Prostigmatic mites consist of parasitic, plant feeding and beneficial predatory species and is the major group of Acari in the world. Untill 2011, 26205 species were described in this suborder, of which 4728 species belong to the cohort Raphignathina and tetranychoid and raphignathoid mites include 2211 and 877 species respectively (Zhang et al. -

The Use of the Naturalism Approach in Designing the Tabriz Carpet Museum
21 DOI: https://dx.doi.org/10.51148/jaas.2018.3 THE USE OF THE NATURALISM APPROACH IN DESIGNING THE TABRIZ CARPET MUSEUM Amir Rishi Jegheh and Ardalan Karimi Ilkhchi branch, Islamic Azad University, Ilkhchi, Iran ABSTRACT Culture and art have come from the very beginning of mankind, along with human life, Research Article in order to calm down humankind, and what comes out of mind in different arts and in different ways. With the advancement of mankind in various arenas and sciences, art, PII: S238315531800003-7 in turn, was subject to change and in various parts of the earth's human races, the craftsmanship of buildings and handicrafts was made in caves. Meanwhile, art in the Middle East from ancient times was the cradle of human civilization and the creator Received: 22 Aug. 2018 and developer of human beings in various fields, including art. From ancient times, Revised: 30 Nov. 2018 especially after the arrival of Islam, Iran has witnessed progress in various fields of Published: 15 Dec. 2018 literary culture, especially art and architecture. In addition to the art of building and architecture, the creation of motifs in the tiling of mosaics etc. Handmade carpet art is one of the characteristics of recognizing the art of the land of Iran, especially the territory of Azerbaijan. Tabriz is a Persian carpet garden with the texture and development of a variety of carpets in different designs with a fringe in the range and worldwide name in different parts of the world. It is worth mentioning that this ancient city has an exhibition or museums in which architecture along with art witnesses the display of authentic Iranian and Islamic art and architecture. -

National Army Day Marked Sion-Making, the Top Diplomat Added
WWW.TEHRANTIMES.COM I N T E R N A T I O N A L D A I L Y 8 Pages Price 50,000 Rials 1.00 EURO 4.00 AED 42nd year No.13922 Monday APRIL 19, 2021 Farvardin 30, 1400 Ramadan 6, 1442 Envoy: Creating a ‘candid Iran freestyle wrestling Ayatollah Khamenei Iran–China cultural ties picture’ about lifting sanctions team crowned Asian donates $120,000 to drastically increased after pursued in Vienna Page 2 champions Page 3 free prisoners Page 7 Islamic Revolution Page 8 See page 3 60% enrichment carried important political messages: Ghalibaf TEHRAN— Mohammad Bagher Ghali- enemies that Iran’s nuclear industry has baf, speaker of the Iranian parliament, become indigenous and no one can stop spoke on Sunday about the 60% uranium the progress of Islamic Iran.” enrichment and the sabotage act at Na- Speaking at the parliament, Ghalibaf called tanz, suggesting that the sabotage must enrichment of uranium to 60% “an epoch-mak- be responded “at the right time”. ing” event in terms of science and technology Noting that enriching uranium up to in addition important political messages. 60% purity carried important political The April 11 sabotage attack on the messages to the West, Ghalibaf said, “Iran’s Natanz nuclear plant is an instance of enemies expected Iran’s nuclear activities war crime in terms of international law to be halted or slowed down by terrorist and the UN Charter. acts, but this enrichment proved to our Continued on page 2 Annual aluminum ingot production up 61% MBS TEHRAN - Production of aluminum ingot ovation Organization (IMIDRO) showed. -

Tabriz Historic Bazaar (Iran) No 1346
Rotterdam, 25–28 June 2007. Tabriz Historic Bazaar (Iran) Weiss, W. M., and Westermann, K. M., The Bazaar: Markets and Merchants of the Islamic World, Thames and Hudson No 1346 Publications, London, 1998. Technical Evaluation Mission: 13–16 August 2009 Additional information requested and received from the Official name as proposed by the State Party: State Party: ICOMOS sent a letter to the State Party on 19 October 2009 on the following issues: Tabriz Historic Bazaar Complex • Further justification of the serial approach to the Location: nomination. • Further explanation of how the three chosen sites Province of East Azerbaijan relate to the overall outstanding value of the property and of how they are functionally linked, Brief description: with reference to the Goi Machid and the Sorkhāb Bazārchā areas, in relation to the wider Tabriz Historic Bazaar Complex consists of a series of Bazaar area. interconnected, covered brick structures, buildings, and • enclosed spaces for different functions. Tabriz and its Expansion of the description of the legal th protection measures. Bazaar were already prosperous and famous in the 13 • century, when the town became the capital city of the Expansion of the description of the objectives country. The importance of Tabriz as a commercial hub and the measures of the planning instruments in continued until the end of the 18th century, with the force in relation to the factors threatening the expansion of Ottoman power. Closely interwoven with property. the architectural fabric is the social and professional • Further explanation of the overall framework of organization of the Bazaar, which allows its functioning the management system and of the state of and makes it into a single, integrated entity. -

An Analysison Urbansprawlinthe Tabriz Metropolitan and Its Fringe Cities
AN ANALYSISON URBANSPRAWLINTHE TABRIZ METROPOLITAN AND ITS FRINGE CITIES 1RASOULGHORBANI, 2MINA FAROKHISOMEH 1Professor in Department of Geography and Urban Planning, University of Tabriz , Tabriz, Iran. 2PhD Candidate of Geography and Urban Planning, University of Tabriz, Tabriz, Iran. Email: [email protected], [email protected] Abstract- This paper assessment causes and effects of urban sprawl development pattern in during 1984- 2011 in fringe cities of the Tabriz metropolitan Area. The sprawl is external growth without control and imbalance at around of urban area that caused of destruction green space, increase traffic, loss of agricultural land and changes it’s to built-up area. In order to detect and evaluate to measure the model of urban sprawl, density and Holderness model was employed. We used quantities data of the study area from the period between 1984 and 2011, and Population Censuses Data. The result of this study shows that economic, social and environmental effects of sprawl caused that change in agriculture land to built-up area, density and transportation system from 1984 to 2011 in the around of Tabriz. Density and area analysis show that there has been an increase growth in area during the 27 years with the Percentage growth in population by 1.43% in Basmenj, 1.62% in Sardrud, 2.67% in Sofyan and 1.98% in Tabriz and with the reduction of density from 1984 to 2011. The Holderness Equation indicates in the fringe of the metropolitan city of Tabriz that on average high percent of the city physical growth was due to some factors other than population growth, and some percent was due to population growth. -

Internal Diversity
GLOBAL DIVERSITIES Internal Diversity Iranian Germans Between Local Boundaries and Transnational Capital Sonja Moghaddari mpimmg Global Diversities Series Editors Steven Vertovec Department of Socio-Cultural Diversity Max Planck Institute for the Study of Religious and Ethnic Diversity Göttingen, Germany Peter van der Veer Department of Religious Diversity Max Planck Institute for the Study of Religious and Ethnic Diversity Göttingen, Germany Ayelet Shachar Department of Ethics, Law, and Politics Max Planck Institute for the Study of Religious and Ethnic Diversity Göttingen, Germany Over the past decade, the concept of ‘diversity’ has gained a leading place in academic thought, business practice, politics and public policy across the world. However, local conditions and meanings of ‘diversity’ are highly dissimilar and changing. For these reasons, deeper and more com- parative understandings of pertinent concepts, processes and phenomena are in great demand. This series will examine multiple forms and configu- rations of diversity, how these have been conceived, imagined, and repre- sented, how they have been or could be regulated or governed, how different processes of inter-ethnic or inter-religious encounter unfold, how conflicts arise and how political solutions are negotiated and prac- ticed, and what truly convivial societies might actually look like. By com- paratively examining a range of conditions, processes and cases revealing the contemporary meanings and dynamics of ‘diversity’, this series will be a key resource for students and professional social scientists. It will repre- sent a landmark within a field that has become, and will continue to be, one of the foremost topics of global concern throughout the twenty-first century. -

Long-Period Ground Motion Simulation for NTF Fault Scenario
Long-period Ground Motion Simulation for NTF Fault NearScenario-source in Tabriz energy City released of 2003 Bam earthquake using slip-weakening law Paper Title Line 1 Mohammad Reza Ghayamghamian International institute of earthquake engineering and seismology, Tehran, Iran Afrooz Rajool Islamic Azad University, Tehran, Iran SUMMARY: Tabriz, one of the metropolises of Iran, is a megacity situated at the northwest of the Iran with more than 1.5 million inhabitants. North Tabriz Fault (NTF) is a major seismogenic fault in NW of Iran that crossed north of Tabriz city and directly threaten metropolitan area of Tabriz. The NTF would have been the source of several major historical earthquakes in the past. Therefore, it is na important task to identify the characteristics of long-period strong ground motions for seismic hazard mitigation plan and design of long structures. The kinematic model with non-uniform slip distribution on the fault plane is employed to simulate velocity waveforms at the sites. To this end, the source parameters for the worst rupture scenario of NTF are defined. Then, the long-period velocity motions for this rupture scenario are simulated at 300 points in a grid of 1 km × 1 km covering whole Tabriz region. The simulated motions clearly show near-fault directivity pulse with different peaks and periods depending on the site location to the fault. The peak velocity (PGV) is found to be in the range of 100 to 255 cm/sec. Furthermore, the response spectra for simulated motions are also calculated, which their peak values vary in the range of 200-330 cm/sec for velocity. -

CV of Bakhtiar Feizizadeh
C V & Research output list P a g e | 1 C V & Research output list P a g e | 1 Curriculum Vitae of Bakhtiar Feizizadeh, born September 21rd 1981 in Malekan, Iran - Name: Bakhtiar Feizizadeh - Academic degree: Associated professor - ORCID: 0000-0002-3367-2925 - Number of publication up to 30. 06.2020: > 150 scientific papers - H-index: 14, Citation < 1730; - Phone, +98 09143058630, - E-Mail: [email protected], [email protected] - Languages: Turkish/Azerbaijani, Persian, English, basic skills in German and Arabic Education /Qualifications - 1.10. 2010- 28.5. 2014: PhD study in Applied Geoinformatics, Department of Geoinformatics, University of Salzburg, Austria. Supervised by Prof.Dr. Thomas Blaschke, PhD thesis topic: “Uncertainty, Sensitivity and Fuzzy Sets in GIS Multi- Criteria Decision Analysis” - 1.10.2012- 30.5. 2013: Scholar researcher and visiting PhD student, Center of GIS in Department of Geography, Supervised by Prof. Dr. Piotr Jankowski, San Diego State University (SDSU), California, USA. - 1.10. 2005-30.12. 2007: Master’s Degree in: Remote sensing and GIS, Department of Remote Sensing and GIS, University of Tabriz, Iran - 1.10. 2001-30.01. 2005: Bachelor’s Degree: Physical Geography (with honors), Department of Physical Geography, University of Tabriz, Iran. Awards - 2020. National Prize as top researcher of Iran, Ministry of Science, Research and Technology of Iran - 2019. Alexander Von Humboldt fellowship for experienced researchers. Germany, University of Humboldt Zu Berlin - 2019. National Prize as honored researcher of East Azerbaijan Provinces, Iran, Governance of East Azerbaijan Provinces - 2018. Prize of University of Tabriz as honoured researcher in 2018 - 2015.