Emerging Drug List — Valdecoxib
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Emerging Drug List PARECOXIB SODIUM
Emerging Drug List PARECOXIB SODIUM NO. 10 MAY 2001 Generic (Trade Name): Parecoxib sodium Manufacturer: Pharmacia & Upjohn Inc. Indication: For peri-operative pain relief Current Regulatory Parecoxib is currently under review at Health Canada and the Food and Drug Status: Administration in the U.S. They are expecting approval in the fourth quarter of 2001. It is not marketed in any country at this time Description: Parecoxib is the first parenteral cyclooxygenase-2 (COX-2) selective inhibitor to be developed. It is a water-soluble prodrug that is rapidly hydrolyzed to valdecoxib (the active COX-2 inhibitor). Valdecoxib's affinity for COX-2 versus COX-1 is 90 times greater than celecoxib and 34,000 times greater than ketorolac. Once injected, peak concentrations of valdecoxib are attained in 10 to 20 minutes. Valdecoxib has a half-life of eight to 10 hours. Current Treatment: Currently, the only other nonsteroidal anti-inflammatory agent that is available as an injection is ketorolac. Ketorolac is used in some centres for peri-operative pain management, however opioids are the main class of agents used for this indication. Ketorolac has been associated with a relatively high incidence of gastrointestinal (GI) side effects, including severe cases of hemorrhage. Cost: There is no information available on the cost of parecoxib. Evidence: Parecoxib has been compared to ketorolac and morphine in clinical trials. Parecoxib at a dose of 20 and 40 mg/day IV, were compared to ketorolac, 30 mg/day IV and morphine, 4 mg/day or placebo in 202 women undergoing hysterectomy. Both doses of parecoxib were comparable to ketorolac for relieving postoperative pain. -

Development and Validation of an Ultra Performance Liquid
DOI: 10.4274/tjps.76588 Turk J Pharm Sci 2017;14(1):1-8 ORIGINAL ARTICLE Development and Validation of an Ultra Performance Liquid Chromatography Method for the Determination of Dexketoprofen Trometamol, Salicylic Acid and Diclofenac Sodium Deksketoprofen Trometamol, Salisilik Asit ve Diklofenak Sodyum Etkin Maddeleri için Ultra Performanslı Sıvı Kromatografisi Yönteminin Geliştirilmesi ve Validasyonu Sibel İLBASMIŞ TAMER Gazi University, Faculty of Pharmacy, Department of Pharmaceutical Technology, Ankara, Turkey ABSTRACT Objectives: A simple, fast, accurate and precise method has been developed for the determination of dexketoprofen trometamol (DKP), salicylic acid (SA) and diclofenac sodium (DIC) in the drug solutions using ultra high performance liquid chromatography (UPLC). Materials and Methods: UPLC method is highly reliable and sensitive method to quantify the amount of the active ingredient and the method is validated according to ICH guidelines. Results: The developed method is found to be precise, accurate, specific and selective. The method was also found to be linear and reproducible. The value of limit of dedection (LOD) of DKP, SA, DIC were found 0.00325 µg/mL, 0.0027 µg/mL and 0.0304 µg/mL, respectively. The limit of quantitation (LOQ) of DKP, SA and DIC were found 0.00985 µg/mL, 0.0081 µg/mL and 0.0920 µg/mL, respectively. Conclusion: Proposed methods can be successfully applicable to the pharmaceutical preparation containing the above mentioned drugs (dexketoprofen trometamol, salicylic acid and diclofenac sodium). Even very small amounts of active substance can be analyzed and validations can be performed easily. Key words: Dexketoprofen trometamol, salicylic acid, diclofenac sodium, UPLC, validation ÖZ Amaç: Deksketoprofen trometamol (DKP), salisilik asit (SA) ve diklofenak sodyumun (DIC) ilaç çözeltisindeki analizi için ultra yüksek basınçlı sıvı kromatografisi (UPLC) kullanılarak basit, hızlı, doğru ve kesin bir yöntem geliştirilmiştir. -

New Restrictions on Celecoxib (Celebrex) Use and the Withdrawal of Valdecoxib (Bextra)
Early release, published at www.cmaj.ca on April 15, 2005. Subject to revision. HEALTH AND DRUG ALERTS P RACTICE New restrictions on celecoxib (Celebrex) use and the withdrawal of valdecoxib (Bextra) Early release, published at www.cmaj.ca on Apr. 15, 2005. Subject to revision. Reason for posting: Coxibs, v. 0.5%; risk ratio 3.7, 95% CI the class of NSAIDs that selec- 1.0–13.5).2 Amid concerns about Table 1: The degree of inhibition of COX-2 relative tively inhibit cyclooxygenase 2 reports of severe cutaneous reac- to COX-1 for various NSAIDs (COX-2), were designed to re- tions (Stevens–Johnson syn- NSAID type COX-2 selectivity* duce joint pain and inflamma- drome, erythema multiforme, tion without causing the gastric toxic epidermal necrolysis) COX-2 selective inhibitors epithelial adverse effects typical among patients taking valde- Rofecoxib 80 of nonselective NSAIDs. Rofe- coxib,5 the drug was removed Etodolac 23 coxib (Vioxx) was withdrawn from the market. Meloxicam 11 from the market in September Celecoxib 9 2004 over concerns about car- What to do: COX-2 inhibitors Nonselective NSAIDs diovascular adverse effects, and appear to increase the risk of car- Diclofenac 4 key safety trials involving cele- diovascular adverse events in a Sulindac 3 coxib (Celebrex)1 and valdecoxib dose-related fashion, and all pa- Piroxicam 2 (Bextra)2 have recently been tients should be informed of this. Ibuprofen 0.4 published. Health Canada now Calculating the patient’s baseline Naproxen 0.3 recommends new restrictions on risk of cardiovascular disease Indomethacin 0.2 celecoxib use, and valdecoxib (e.g., with Framingham risk cal- Ketorolac 0.003 has been taken off the market.3 culators) may be wise, and cele- Note: COX = cyclooxygenase. -

Non Steroidal Anti-Inflammatory Drugs
Non Steroidal Anti‐inflammatory Drugs (NSAIDs) 4 signs of inflammation • Redness ‐ due to local vessel dilatation • Heat ‐ due to local vessel dilatation • Swelling – due to influx of plasma proteins and phagocytic cells into the tissue spaces • Pain – due to local release of enzymes and increased tissue pressure NSAIDs • Cause relief of pain ‐. analgesic • Suppress the signs and symptoms of inflammation. • Exert antipyretic action. • Useful in pain related to inflammation. Esp for superficial/integumental pain . Classification of NSAIDs • Salicylates: aspirin, Sodium salicylate & diflunisal. • Propionic acid derivatives: ibuprofen, ketoprofen, naproxen. • Aryl acetic acid derivatives: diclofenac, ketorolac • Indole derivatives: indomethacin, sulindac • Alkanones: Nabumetone. • Oxicams: piroxicam, tenoxicam Classification of NSAIDs ….. • Anthranilic acid derivatives (fenamates): mefenamic acid and flufenamic acid. • Pyrazolone derivatives: phenylbutazone, oxyphenbutazone, azapropazone (apazone) & dipyrone (novalgine). • Aniline derivatives (analgesic only): paracetamol. Clinical Classif. • Non selective Irreversible COX inhibitors • Non slective Reversible COX inhibitors • Preferential COX 2 inhibitors • 10‐20 fold cox 2 selective • meloxicam, etodolac, nabumetone • Selective COX 2 inhibitors • > 50 fold COX ‐2 selective • Celecoxib, Etoricoxib, Rofecoxib, Valdecoxib • COX 3 Inhibitor? PCM Cyclooxygenase‐1 (COX‐1): -constitutively expressed in wide variety of cells all over the body. -"housekeeping enzyme" -ex. gastric cytoprotection, hemostasis Cyclooxygenase‐2 (COX‐2): -inducible enzyme -dramatically up-regulated during inflammation (10-18X) -constitutive : maintains renal blood flow and renal electrolyte homeostasis Salicylates Acetyl salicylic acid (aspirin). Kinetics: • Well absorbed from the stomach, more from upper small intestine. • Distributed all over the body, 50‐80% bound to plasma protein (albumin). • Metabolized to acetic acid and salicylates (active metabolite). • Salicylate is conjugated with glucuronic acid and glycine. • Excreted by the kidney. -

Metabolic Profiling of Murine Plasma Reveals an Unexpected Biomarker In
Metabolic profiling of murine plasma reveals an unexpected biomarker in rofecoxib-mediated cardiovascular events Jun-Yan Liua, Ning Lib, Jun Yanga, Nan Lic, Hong Qiub, Ding Aia,c, Nipavan Chiamvimonvatb, Yi Zhuc, and Bruce D. Hammocka,1 aDepartment of Entomology and University of California-Davis Cancer Center and bDivision of Cardiovascular Medicine, University of California, Davis, CA 95616; and cDepartment of Physiology, Beijing University, Beijing 100083, People’s Republic of China Contributed by Bruce D. Hammock, August 6, 2010 (sent for review June 16, 2010) Chronic administration of high levels of selective COX-2 inhibitors infarction (MI), hypertension, and heart failure has also been ob- (coxibs), particularly rofecoxib, valdecoxib, and parecoxib, increases served to be associated with the administration of the nonaspirin risk for cardiovascular disease. Understanding the possibly multiple conventional NSAIDs, including but not limited to diclofenac, mechanisms underlying these adverse cardiovascular events is critical ibuprofen, naproxen, and indomethacin (8–12). In addition, there for evaluating the risks and benefits of coxibs and for development of could be rofecoxib-specific events such as the facile formation of safer coxibs. The current understanding of these mechanisms is likely a cardiotoxic maleic anhydride derivative from rofecoxib that may incomplete. Using a metabolomics approach, we demonstrate that contribute to its adverse effects (13). This hypothesis fails to ex- oral administration of rofecoxib for 3 mo results in a greater than 120- plain the increased risk in the cardiovascular system from other fold higher blood level of 20-hydroxyeicosatetraenoic acid (20-HETE), nonaspirin NSAIDs. Thus, current mechanisms provide an in- fi which correlates with a signi cantly shorter tail bleeding time in complete explanation for cardiovascular problems associated with a murine model. -

Bextra, INN-Valdecoxib
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Bextra 10 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each film-coated tablet contains 10 mg valdecoxib. For excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablets White, capsule-shaped, debossed ‘10’ on one side and ‘7815’ on the other. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Symptomatic relief in the treatment of osteoarthritis or rheumatoid arthritis. Treatment of primary dysmenorrhoea. 4.2 Posology and method of administration Bextra is administered orally. Bextra may be taken with or without food (see section 5.2). Osteoarthritis and rheumatoid arthritis: The recommended dose is 10 mg once daily. Some patients may receive additional benefit from 20 mg once daily. The maximum recommended dose is 20 mg once daily. Treatment of primary dysmenorrhoea: The recommended dose for symptomatic relief is 40 mg once daily as required. On the first day of treatment, an additional 40 mg dose may be taken if needed. Thereafter, the maximum recommended dose is 40 mg once daily. Elderly: For elderly patients (≥ 65 years), in particular those of less than 50 kg body weight, initiate therapy at the lowest recommended dose for osteoarthritis and rheumatoid arthritis (10 mg once daily) (see section 5.2). Hepatic Impairment: No dosage adjustment is generally necessary in patients with mild hepatic impairment (Child-Pugh score 5-6). In patients with moderate hepatic impairment (Child-Pugh score 7- 9 ) treatment should be initiated with caution. The lowest recommended dose should be used for osteoarthritis and rheumatoid arthritis (10 mg once daily) and the dosage should not exceed 20 mg for primary dysmenorrhoea. -

Received July 12, 2005, Accepted October 18, 2005 V. Ciddi University College of Pharmaceutical Sciences, Kakatiya University, W
SHORT COMMUNICATIONS the corresponding parent drug 1. At the LC50 level 1 ex- Faculty of Pharmaceutical Sciences, Kakatiya University, Warangal, hibited an about 1 log unit stronger cytotoxic effect India (MGM Àlog LC50 (1) ¼ 5.25/5.10 vs. MGM–– log LC50 (2) ¼ 4.02) and at the GI50 and TGI level it even led to an Determination of valdecoxib in serum using increase in growth inhibitory effects of about 1.5 log units a HPLC-diode array detector and its application (MGM–– log GI50 (1) ¼ 6.42/6.45 vs. MGM–– log GI50 in a pharmacokinetic study (2) ¼ 4.95 and MGM–– log TGI (1) ¼ 5.88/5.87 vs. MGM–– log TGI (2) 4.31). ¼ S. Keshetty, R. K. Venisetty, V. Molmoori, V. Ciddi Furthermore, formation of the 2-hydroxyl compound 1 was observed upon incubation of prodrug 2 at a concen- tration of 10À5 M with 2 mg/ml enzyme and 5 Â 10À5 M Received July 12, 2005, accepted October 18, 2005 NADH in phosphate buffer at 37 C which is a clear evi- dence that prodrug 2 is a substrate for for E. coli nitrore- V. Ciddi University College of Pharmaceutical Sciences, ductase (data not shown). Kakatiya University, Warangal – 506 009, AP, India [email protected] References Pharmazie 61: 245–246 (2006) Asche C, Frank W, Albert A, Kucklaender U (2005) Synthesis, antitumour activity and structure-activity relationships of 5H-benzo[b]carbazoles. Bioorgan Med Chem 13: 819–837. Carl PL, Chakravarty PK, Katzenellenbogen JA (1981) A novel connector linkage applicable in prodrug design. -

Acute Congestive Heart Failure Induced by Rofecoxib
J Am Board Fam Pract: first published as 10.3122/jabfm.17.2.131 on 13 April 2004. Downloaded from Acute Congestive Heart Failure Induced by Rofecoxib Robert J. Campbell, MD, and Kevin B. Sneed, PharmD Nonsteroidal anti-inflammatory drugs (NSAIDs) COX-1 in the stomach is believed to have protec- are routinely prescribed for the treatment of vari- tive properties of the gastric mucosa.12,13 COX-2 is ous conditions requiring analgesia and anti-inflam- expressed in response to inflammatory stimuli, and matory activity. People also have access to NSAIDs is affected by cytokines and other inflammatory over-the-counter for relief of mild aches, pains, and mediators. Most NSAIDs inhibit both isoforms to headaches. NSAIDs have the potential to produce varying degrees, relative to the activity of the indi- several adverse effects in patients. They are known vidual chemical properties of the NSAID. In recent to have the potential to produce gastrointestinal years, COX-2 specific inhibitors have become toxicities leading to dyspepsia or even ulceration. available [celecoxib, rofecoxib, valdecoxib (in order Gastrointestinal symptoms are the most common of US market release)]. It had been hypothesized adverse effects associated with NSAID use.1 Plate- that by targeting the COX-2 enzyme specifically, let aggregation is known to be inhibited by only the inflammatory prostaglandins would be in- NSAIDs because of their ability to inhibit the ac- hibited while sparing the activity of COX-1. This tion of thromboxane A, a potent platelet aggrega- would allow the medication to produce anti- tor.2–4 This could lead to hemorrhaging in patients inflammatory and analgesia activities without po- with vascular injuries or congenital hematologic tentially decreasing the protective effects of the conditions. -
Parecoxib (As Sodium)
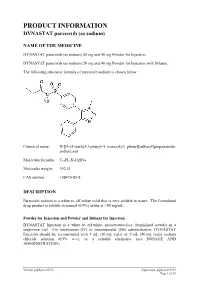
PRODUCT INFORMATION DYNASTAT parecoxib (as sodium) NAME OF THE MEDICINE DYNASTAT parecoxib (as sodium) 20 mg and 40 mg Powder for Injection. DYNASTAT parecoxib (as sodium) 20 mg and 40 mg Powder for Injection with Diluent. The following structural formula of parecoxib sodium is shown below: Chemical name: N-[[4-(5-methyl-3-phenyl-4 isoxazolyl) phenyl]sulfonyl]propanamide, sodium salt Molecular formula: C19H17N2O4SNa Molecular weight: 392.41 CAS number: 198470-85-8 DESCRIPTION Parecoxib sodium is a white to off-white solid that is very soluble in water. The formulated drug product is soluble in normal (0.9%) saline at >50 mg/mL. Powder for Injection and Powder and Diluent for Injection DYNASTAT Injection is a white to off-white, preservative-free, lyophilised powder in a single-use vial. For intravenous (IV) or intramuscular (IM) administration, DYNASTAT Injection should be reconstituted with 1 mL (20 mg vials) or 2 mL (40 mg vials) sodium chloride solution (0.9% w/v), or a suitable alternative (see DOSAGE AND ADMINISTRATION). Version: pfpdynav10213 Supersedes: pfpdynav10912 Page 1 of 25 Diluent for Injection DYNASTAT Injection may be supplied with a 2 mL capacity diluent ampoule with a fill volume of either 1 mL or 2 mL Sodium Chloride Intravenous Infusion (0.9% w/v) BP. Reconstituted Solution The reconstituted solution is clear and colourless. DYNASTAT Injection 20 mg and 40 mg contains parecoxib sodium, sodium phosphate-dibasic anhydrous; phosphoric acid and/or sodium hydroxide may have been added to adjust pH. When reconstituted in sodium chloride solution (0.9% w/v), DYNASTAT Injection contains approximately 0.22 mEq and 0.44 mEq of sodium per 20 mg vial and 40 mg vial, respectively. -

Is Ketorolac Safe for Use After Cardiac Surgery?
Black Box Warning: Is Ketorolac Safe for Use After Cardiac Surgery? Lisa Oliveri, BSc,*† Katie Jerzewski, BSc,*† and Alexander Kulik, MD, MPH*† Objective: In 2005, after the identification of cardiovascu- similar to those expected using Society of Thoracic Surgery lar safety concerns with the use of nonsteroidal anti- database risk-adjusted outcomes. In unadjusted analysis, inflammatory drugs (NSAIDs), the FDA issued a black box patients who received ketorolac had similar or better post- warning recommending against the use of NSAIDs following operative outcomes compared with patients who did not cardiac surgery. The goal of this study was to assess the receive ketorolac, including gastrointestinal bleeding (1.2% v postoperative safety of ketorolac, an intravenously admin- 1.3%; p ¼ 1.0), renal failure requiring dialysis (0.4% v 3.0%; istered NSAID, after cardiac surgery. p ¼ 0.001), perioperative myocardial infarction (1.0% v 0.6%; Design: Retrospective observational study. p ¼ 0.51), stroke or transient ischemic attack (1.0% v 1.7%; Setting: Single center, regional hospital. p ¼ 0.47), and death (0.4% v 5.8%; p o 0.0001). With adjust- Participants: A total of 1,309 cardiac surgical patients ment in a multivariate model, treatment with ketorolac was (78.1% coronary bypass, 28.0% valve) treated between 2006 not a predictor for adverse outcome in this cohort (odds and 2012. ratio: 0.72; p ¼ 0.23). Interventions: A total of 488 of these patients received Conclusions: Ketorolac appears to be well-tolerated for ketorolac for postoperative analgesia within 72 hours of use when administered selectively after cardiac surgery. -

A High Level of Cyclooxygenase-2 Inhibitor Selectivity Is Associated with a Reduced Interference of Platelet Cyclooxygenase-1 Inactivation by Aspirin
A high level of cyclooxygenase-2 inhibitor selectivity is associated with a reduced interference of platelet cyclooxygenase-1 inactivation by aspirin Marc Ouellet, Denis Riendeau, and M. David Percival* Department of Biochemistry and Molecular Biology, Merck Frosst Centre for Therapeutic Research, Kirkland, QC, Canada H9R 4P8 Communicated by Edward M. Scolnick, Merck & Co., Inc., West Point, PA, October 12, 2001 (received for review July 12, 2001) Both nonsteroidal anti-inflammatory drugs, such as ibuprofen, and definitively established, coadministration of low-dose aspirin is the prototypical selective cyclooxygenase (Cox)-2 inhibitors DuP- recommended for high-risk patients taking NSAIDs for the 697 and NS-398 block the inhibition of Cox-1 by aspirin in vitro. treatment of inflammatory disorders (8). However, in vitro However, clinical studies have shown that the Cox-2 selective enzyme and human studies performed in the early 1980s showed drugs (or coxibs) rofecoxib and etoricoxib, at therapeutic doses, do that the NSAIDs ibuprofen and indomethacin can block aspirin not interfere with the antiplatelet effect of aspirin, in contrast to inactivation of Cox-1 (9–12). Very recently, a clinical study ibuprofen. Here, we have evaluated the relative potential of confirmed that ibuprofen does block platelet Cox-1 inhibition by ibuprofen and various coxibs to interfere with the inactivation of low-dose aspirin, suggesting that that the coadministration of the Cox-1 by aspirin by using purified enzyme and calcium ionophore- two drugs may compromise the cardioprotective effect of aspirin activated human platelets. The irreversible inactivation of Cox-1 by (42). The Cox-2 selective inhibitors NS-398 and DuP-697 also aspirin can be antagonized by ibuprofen and coxibs, albeit with have been reported to block the aspirin-mediated inhibition of widely different potencies. -

Plants As Sources of Anti-Inflammatory Agents
molecules Review Plants as Sources of Anti-Inflammatory Agents Clara dos Reis Nunes 1 , Mariana Barreto Arantes 1, Silvia Menezes de Faria Pereira 1, Larissa Leandro da Cruz 1, Michel de Souza Passos 2, Luana Pereira de Moraes 1, Ivo José Curcino Vieira 2 and Daniela Barros de Oliveira 1,* 1 Laboratório de Tecnologia de Alimentos, Centro de Ciências e Tecnologias Agropecuárias, Universidade Estadual do Norte Fluminense Darcy Ribeiro, Campos dos Goytacazes, RJ 28013-602, Brazil; [email protected] (C.d.R.N.); [email protected] (M.B.A.); [email protected] (S.M.d.F.P.); [email protected] (L.L.d.C.); [email protected] (L.P.d.M.) 2 Laboratório de Ciências Químicas, Centro de Ciências e Tecnologia, UniversidadeEstadual do Norte Fluminense Darcy Ribeiro, Campos dos Goytacazes, RJ 28013-602, Brazil; [email protected] (M.d.S.P.); [email protected] (I.J.C.V.) * Correspondence: [email protected]; Tel.: +55-22-988395160 Academic Editors: Thea Magrone, Rodrigo Valenzuela and Karel Šmejkal Received: 29 June 2020; Accepted: 5 August 2020; Published: 15 August 2020 Abstract: Plants represent the main source of molecules for the development of new drugs, which intensifies the interest of transnational industries in searching for substances obtained from plant sources, especially since the vast majority of species have not yet been studied chemically or biologically, particularly concerning anti-inflammatory action. Anti-inflammatory drugs can interfere in the pathophysiological process of inflammation, to minimize tissue damage and provide greater comfort to the patient. Therefore, it is important to note that due to the existence of a large number of species available for research, the successful development of new naturally occurring anti-inflammatory drugs depends mainly on a multidisciplinary effort to find new molecules.