Idiopathic Rhabdomyolysis D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Ketones, Urine
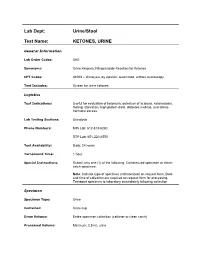
Lab Dept: Urine/Stool Test Name: KETONES, URINE General Information Lab Order Codes: UKE Synonyms: Urine Ketones; Nitroprusside Reaction for Ketones CPT Codes: 81003 – Urinalysis, by dipstick; automated, without microscopy Test Includes: Screen for urine ketones. Logistics Test Indications: Useful for evaluation of ketonuria, detection of acidosis, ketoacidosis, fasting, starvation, high protein diets, diabetes mellitus, and stress- hormone excess. Lab Testing Sections: Urinalysis Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6550 Test Availability: Daily, 24 hours Turnaround Time: 1 hour Special Instructions: Submit only one (1) of the following: Catheterized specimen or clean- catch specimen. Note: Indicate type of specimen (catheterized) on request form. Date and time of collection are required on request form for processing. Transport specimen to laboratory immediately following collection Specimen Specimen Type: Urine Container: Urine cup Draw Volume: Entire specimen collection (catheter or clean catch) Processed Volume: Minimum: 0.5 mL urine Collection: A specimen collected by catheterization is optimal; however, a clean- catch or mid-stream specimen is also acceptable. Random, voided specimens will be accepted, but are the least desirable and are not recommended if a urine culture is also being requested. Special Processing: N/A Patient Preparation: None Sample Rejection: Less than 0.5 mL urine submitted; mislabeled or unlabeled specimen Interpretive Reference Range: Negative Critical Values: N/A Limitations: Specimens containing -

Gluteal Muscle Contracture: Diagnosis and Management Options
SICOT J 2017, 3,1 Ó The Authors, published by EDP Sciences, 2017 DOI: 10.1051/sicotj/2016036 Available online at: www.sicot-j.org REVIEW ARTICLE OPEN ACCESS Gluteal muscle contracture: diagnosis and management options Saroj Rai1, Chunqing Meng1,*, Xiaohong Wang1, Nabin Chaudhary2, Shengyang Jin1, Shuhua Yang1, and Hong Wang1 1 Department of Orthopedics, Wuhan Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, #1277 Jiefang Avenue, 430022 Wuhan, P.R. China 2 Department of Radiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, #1095 Jiefang Avenue, 430030 Wuhan, P.R. China Received 14 April 2016, Accepted 29 October 2016, Published online 6 January 2017 Abstract – Gluteal muscle contracture (GMC), a debilitating disease, exists all over the globe but it is much more prevalent in China. Patients typically present with abduction and external rotation of the hip and are unable to bring both the knees together while squatting. Multiple etiologies have been postulated, the commonest being repeated intramuscular injection into the buttocks. The disease is diagnosed primarily by clinical features but radiological features are necessary for the exclusion of other pathological conditions. Non-operative treatment with physiotherapy can be tried before surgery is considered but it usually fails. Different surgical techniques have been described and claimed to have a better outcome of one over another but controversy still exists. Based on published literatures, the clinical outcome is exceptionally good in all established methods of surgery. However, endoscopic surgery is superior to conventional open surgery in terms of cosmetic outcome with fewer complications. Nevertheless, its use has been limited by lack of adequate knowledge, instrumentations, and some inherent limitations. -

Cancer Cachexia Decreases Specific Force and Accelerates Fatigue in Limb Muscle
Biochemical and Biophysical Research Communications 435 (2013) 488–492 Contents lists available at SciVerse ScienceDirect Biochemical and Biophysical Research Communications journal homepage: www.elsevier.com/locate/ybbrc Cancer cachexia decreases specific force and accelerates fatigue in limb muscle ⇑ B.M. Roberts a, G.S. Frye b, B. Ahn b, L.F. Ferreira b,1, A.R. Judge a,1, a 1225 Center Drive, HPNP Building Room 1142, Department of Physical Therapy, University of Florida, Gainesville, FL 32610, USA b 1864 Stadium Road, Department of Applied Physiology & Kinesiology, University of Florida, Gainesville, FL 32610, USA article info abstract Article history: Cancer cachexia is a complex metabolic syndrome that is characterized by the loss of skeletal muscle Received 30 April 2013 mass and weakness, which compromises physical function, reduces quality of life, and ultimately can Available online 11 May 2013 lead to mortality. Experimental models of cancer cachexia have recapitulated this skeletal muscle atro- phy and consequent decline in muscle force generating capacity. However, more recently, we provided Keywords: evidence that during severe cancer cachexia muscle weakness in the diaphragm muscle cannot be Muscle weakness entirely accounted for by the muscle atrophy. This indicates that muscle weakness is not just a conse- Muscle atrophy quence of muscle atrophy but that there is also significant contractile dysfunction. The current study C-26 aimed to determine whether contractile dysfunction is also present in limb muscles during severe Contractile dysfunction Colon-26 (C26) carcinoma cachexia by studying the glycolytic extensor digitorum longus (EDL) muscle and the oxidative soleus muscle, which has an activity pattern that more closely resembles the dia- phragm. -

Surgeons, Columbia University, New York City) (Received for Publication August 9, 1932)
THE ADDIS SEDIMENT COUNT IN NORMAL CHILDREN By JOHN D. LYTTLE (From the Babies Hospit and the Department of Pediatrics, Colege of Physicians and Surgeons, Columbia University, New York City) (Received for publication August 9, 1932) THE METHOD In 1925 Addis (1) described a method by which, in a concentrated acid urine, the rate of excretion of protein, casts and red and white cells could be determined. His method, with certain modifications, has been followed here. All of the counts were made on the 12 hour night specimen from 7 or 8 P.M. to 7 or 8 A.M. Addis recommended that fluids be restricted during, and for 12 hours preceding the collection, since in dilute and alkaline urine hyaline casts dissolve and red cells may be completely lysed. With children this rigid restriction of fluid proved impossible. Withholding fluid during the afternoon and night except for 200 cc. at the evening meal, gave urines of such concentration and acidity that they were suitable for a count. Most children had an early supper and col- lections were started at 7 or 8 P.M. Under these conditions, the urinary pH was between 5.0 and 6.0 and the specific gravity usually well above 1.020. The specimens were treated as described by Addis: "the con- centrated night urine is thoroughly mixed by repeated inversion of the rubber-stoppered bottle and a 10 cc. sample is transferred to a special graduated tube, and centrifugalized for five minutes at 1,800 revolutions per minute. The supernatant urine is decanted and pipetted down to a known volume which varies with the amount of sediment as judged by direct observation. -

Different Response of Body Weight Change According to Ketonuria After Fasting in the Healthy Obese
ORIGINAL ARTICLE Endocrinology, Nutrition & Metabolism http://dx.doi.org/10.3346/jkms.2012.27.3.250 • J Korean Med Sci 2012; 27: 250-254 Different Response of Body Weight Change According to Ketonuria after Fasting in the Healthy Obese Hyeon-Jeong Kim1, Nam-Seok Joo1, The relationship between obesity and ketonuria is not well-established. We conducted a Kwang-Min Kim1, Duck-Joo Lee1, retrospective observational study to evaluate whether their body weight reduction response and Sang-Man Kim2 differed by the presence of ketonuria after fasting in the healthy obese. We used the data of 42 subjects, who had medical records of initial urinalysis at routine health check-up and 1Department of Family Practice and Community Health, Ajou University School of Medicine, Suwon; follow-up urinalysis in the out-patient clinic, one week later. All subjects in the initial 2Department of Family Medicine, CHA Biomedical urinalysis showed no ketonuria. However, according to the follow-up urinalysis after three Center, CHA University College of Medicine, Seoul, subsequent meals fasts, the patients were divided into a non-ketonuria group and Korea ketonuria group. We compared the data of conventional low-calorie diet programs for ± Received: 20 August 2011 3 months for both groups. Significantly greater reduction of body weight (-8.6 3.6 kg vs 2 2 Accepted: 17 January 2012 -1.1 ± 2.2 kg, P < 0.001), body mass index (-3.16 ± 1.25 kg/m vs -0.43 ± 0.86 kg/m , P < 0.001) and waist circumference (-6.92 ± 1.22 vs -2.32 ± 1.01, P < 0.001) was Address for Correspondence: observed in the ketonuria group compared to the non-ketonuria group. -

Deficient Diabetic Mice
Diminished Loss of Proteoglycans and Lack of Albuminuria in Protein Kinase C-␣–Deficient Diabetic Mice Jan Menne,1,2 Joon-Keun Park,2 Martin Boehne,2 Marlies Elger,2 Carsten Lindschau,2 Torsten Kirsch,2 Matthias Meier,2 Faikah Gueler,2 Annette Fiebeler,3 Ferdinand H. Bahlmann,2 Michael Leitges,4 and Hermann Haller2 Activation of protein kinase C (PKC) isoforms has been implicated in the pathogenesis of diabetic nephropathy. We showed earlier that PKC-␣ is activated in the kid- iabetes affects Ͼ300 million people worldwide; -neys of hyperglycemic animals. We now used PKC-␣؊/؊ 20–40% will develop overt nephropathy. Diabe mice to test the hypothesis that this PKC isoform tes is the most common cause of end-stage mediates streptozotocin-induced diabetic nephropathy. Drenal disease. The earliest clinical sign of ne- We observed that renal and glomerular hypertrophy was phropathy is microalbuminuria. Microalbuminuria also ؊ ؊ similar in diabetic wild-type and PKC-␣ / mice. How- heralds impending cardiovascular morbidity and mortality ever, the development of albuminuria was almost absent (1–4). Microalbuminuria predicts overt proteinuria, which ؊/؊␣ in the diabetic PKC- mice. The hyperglycemia-in- is now believed to actively promote renal insufficiency (5). duced downregulation of the negatively charged base- Therefore, successful treatment of diabetic patients ment membrane heparan sulfate proteoglycan perlecan -؊ ؊ should aim for the prevention or regression of albumin was completely prevented in the PKC-␣ / mice, com- pared with controls. We then asked whether transform- uria. Hyperglycemia seems to cause microalbuminuria in   diabetic patients (6,7). However, how the metabolic dis- ing growth factor- 1 (TGF- 1) and/or vascular endothelial growth factor (VEGF) is implicated in the turbance causes cellular effects is incompletely under- PKC-␣–mediated changes in the basement membrane. -

Ideal Conditions for Urine Sample Handling, and Potential in Vitro Artifacts Associated with Urine Storage
Urinalysis Made Easy: The Complete Urinalysis with Images from a Fully Automated Analyzer A. Rick Alleman, DVM, PhD, DABVP, DACVP Lighthouse Veterinary Consultants, LLC Gainesville, FL Ideal conditions for urine sample handling, and potential in vitro artifacts associated with urine storage 1) Potential artifacts associated with refrigeration: a) In vitro crystal formation (especially, calcium oxalate dihydrate) that increases with the duration of storage i) When clinically significant crystalluria is suspected, it is best to confirm the finding with a freshly collected urine sample that has not been refrigerated and which is analyzed within 60 minutes of collection b) A cold urine sample may inhibit enzymatic reactions in the dipstick (e.g. glucose), leading to falsely decreased results. c) The specific gravity of cold urine may be falsely increased, because cold urine is denser than room temperature urine. 2) Potential artifacts associated with prolonged storage at room temperature, and their effects: a) Bacterial overgrowth can cause: i) Increased urine turbidity ii) Altered pH (1) Increased pH, if urease-producing bacteria are present (2) Decreased pH, if bacteria use glucose to form acidic metabolites iii) Decreased concentration of chemicals that may be metabolized by bacteria (e.g. glucose, ketones) iv) Increased number of bacteria in urine sediment v) Altered urine culture results b) Increased urine pH, which may occur due to loss of carbon dioxide or bacterial overgrowth, can cause: i) False positive dipstick protein reaction ii) Degeneration of cells and casts iii) Alter the type and amount of crystals present 3) Other potential artifacts: a) Evaporative loss of volatile substances (e.g. -

Spinal Muscular Atrophy
FACT SHEET SPINAL MUSCULAR ATROPHY Spinal Muscular Atrophy (SMA) is a Motor Neuron Disease. It is caused by the mutation of the Survival of SYMPTOMS IN INFANTS • Muscle weakness. Motor Neuron (SMN) gene. It occurs due to the loss of • Muscle atrophy (wasting). motor neurons within the spinal cord and brain. It results • Poor muscle tone. in the progressive wasting away of muscles (atrophy) and • Areflexia (delayed reflexes). muscle weakness. SMA can affect people of all ages, races • Weak cry. or genders; however, the majority of cases occur in infancy • Difficulty sucking or swallowing. or childhood. There are four types of SMA. • Feeding difficulties. FORMS OF SMA • Weak cough. • Lack of developmental milestones (inability to lift head TYPE I (ACUTE INFANTILE) or sit up). • Also called Wernig-Hoffman Disease. • Limpness or a tendency to flop. • Most severe form of SMA. • Accumulations of secretions in the lungs or throat. • Usually diagnosed before six months of age. • Those affected cannot sit without support, lungs may SYMPTOMS IN ADULTS not fully develop, swallowing and breathing may be • Muscle weakness. difficult and there is weakness of the intercostal muscles • Muscle atrophy (wasting). (muscles between the ribs). • Weak tongue. • 95 per cent fatal by 18 • Stiffness. • Cramps. TYPE II (CHRONIC INFANTILE) • Fasciculation (twitching). • Usually diagnosed before the age of two, with the • Clumsiness. majority of cases diagnosed by 15 months. • Dyspnea (shortness of breath). • May be able to sit without assistance or even stand with support. DIAGNOSIS • Increased risk for complications from respiratory • A diagnosis can be made by an SMN gene test which infections. -

Skeletal Muscle Damage in COVID-19: a Call for Action
medicina Review Skeletal Muscle Damage in COVID-19: A Call for Action Amira Mohammed Ali 1,2,* and Hiroshi Kunugi 3,4 1 Department of Psychiatric Nursing and Mental Health, Faculty of Nursing, Alexandria University, Alexandria 21527, Egypt 2 Department of Behavioral Medicine, National Institute of Mental Health, National Center of Neurology and Psychiatry, Tokyo 187-8553, Japan 3 Department of Psychiatry, School of Medicine, Teikyo University, Tokyo 173-8605, Japan; [email protected] 4 Department of Mental Disorder Research, National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo 187-8551, Japan * Correspondence: [email protected]; Tel.: +81-042-346-1986 Abstract: Both laboratory investigations and body composition quantification measures (e.g., com- puted tomography, CT) portray muscle loss in symptomatic Coronavirus disease 2019 (COVID-19) patients. Muscle loss is associated with a poor prognosis of the disease. The exact mechanism of muscle damage in COVID-19 patients, as well as the long-term consequences of muscle injury in disease survivors, are unclear. The current review briefly summarizes the literature for mechanisms, assessment measures, and interventions relevant to skeletal muscle insult in COVID-19 patients. Muscle injury is likely to be attributed to the cytokine storm, disease severity, malnutrition, prolonged physical inactivity during intensive care unit (ICU) stays, mechanical ventilation, and myotoxic drugs (e.g., dexamethasone). It has been assessed by imaging and non-imaging techniques (e.g., CT and electromyography), physical performance tests (e.g., six-minute walk test), anthropometric measures (e.g., calf circumference), and biomarkers of muscle dystrophy (e.g., creatine kinase). Interventions Citation: Ali, A.M.; Kunugi, H. -

Albuminuria Versus Egfr
Albuminuria versus GFR as markers of diabetic CKD progression KDIGO Controversies Conference: “Diabetic Kidney Disease” New Delhi, March 2012 Richard J MacIsaac PhD FRACP Director of Endocrinology & Diabetes, St Vincent's Hospital Professorial Fellow, University of Melbourne Evolution of Diabetic CKD Incipient Overt Nephropathy Nephropathy GFR 100 Log AER (ml/min) GFR 10 15 20 yrs Normoalbuminuria Microalbuminuria Macroalbuminuria (AER < 20 µµµg/min) (AER 20-200 µµµg/min) (AER > 200 µµµg/min) Stages of CKD Stage eGFR Description Predominant (ml/min/1.73 m2) AER status 1 > 90 Kidney damage with normal/high GFR Normo- Micro- 2 60-89 Kidney damage with mild reduction in GFR Micro- 3 30-59 Kidney damage with moderate reduction in Micro/Macro- GFR 4 15-29 Kidney damage with severe reduction in Macro- GFR 5 < 15 Kidney failure Albuminuria versus GFR as markers of diabetic CKD progression 1. Albuminuria as a predictor of diabetic CKD 2. GFR as a predictor of diabetic CKD 3. Albuminuria & GFR uncoupling/coupling 4. Summary Albuminuria as a marker of diabetic CKD progression • High Variability M N • Low Specificity • Spontaneous Regression µ • Δ AER ≠ Δ GFR Higher levels of urinary albumin excretion within the normal range predict faster decline in glomerular filtration rate in diabetic patients Babazono T et al. Diabetes Care 2009;32:1518-1520 Albuminuria versus GFR as markers of diabetic CKD progression 1. Albuminuria as a predictor of diabetic CKD 2. GFR as a predictor of diabetic CKD 3. ALbuminuria & GFR uncoupling/coupling 4. Summary GFR as -

Biochemical Profiling of Renal Diseases
INTRODUCTION TO LABORATORY PROFILING Alan H. Rebar, DVM, Ph.D., Diplomate ACVP Purdue University, Discovery Park 610 Purdue Mall, West Lafayette, IN 47907-2040 Biochemical profiling may be defined as the use of multiple blood chemistry determinations to assess the health status of various organ systems simultaneously. Biochemical profiling rapidly has become a major diagnostic aid for the practicing veterinarian for several reasons. First, a more educated clientele has come to expect increased diagnostic sophistication. Secondly, the advent of high-volume clinical pathology laboratories has resulted in low prices that make profiling in veterinary practice feasible and convenient. In addition, improved technology has resulted in the development of procedures that can be used to obtain accurate analyses on microsamples of serum. Such procedures offer obvious advantages to veterinarians, who in the past were hindered by requirements for large sample size. Although biochemical profiling offers exciting potential, it is not a panacea. Since standard chemical screens provide 12 to 30 test results, interpretation of data may be extremely complex. Interpretation is often clouded by the fact that perfectly normal animals may have, indeed, are expected to have, an occasional abnormal test result. It is estimated that in a panel of 12 chemistry tests, approximately 46% of all normal subjects will have at least one abnormal test result. Such abnormalities do not reflect inaccuracies in laboratory test procedures but rather the way in which reference (or normal) values are determined. In order to establish the "normal range" for a given test, the procedure is performed on samples from a large population of clinically normal individuals. -

KETON.Zemia and KETONURIA in CHILDHOOD. by MURIEL J
Arch Dis Child: first published as 10.1136/adc.1.5.302 on 1 January 1926. Downloaded from KETON.zEMIA AND KETONURIA IN CHILDHOOD. BY MURIEL J. BROWN, M.B., Ch.B., D.P.H., AND GRACE GRAHAMI, AM.D. From the Medical Department, The Royal Hospital for Sick Children, Glasgow. The formation of ketone bodies and their excretion in the urine in albnormall amounts have for many years been problems of much interest to both physiologist and clinician. Much of our present knowledge of the subject has been gained from the study of carbohydrate metabolism in diabetes, where ketonuria in its classical formi is frequently observed. From this it has been established that an excess of ketone bodies occurs in the blood when the fats are incompletely ' combusted ' as a result of abnormal carbohydrate metabolism, and ample justification has been provided for the well-known sta.tement myiade by Rosenfeld(l) in 1895 ' that fat burns only in the fire of carbohydrate.' A good review of our present knowledge of ketone production and its prevention is to be found in Shaffer's recent lecture entitled ' Antiketo- genesis, its Mechanism and Signifiecance. '(2) A fu-ll discussion of the stubject in all its aspects is not within the scope of the present communication, but we may quote that ' there no Shaffer's statement is to-day question that http://adc.bmj.com/ ketosis is due to carbohydrate starvation,' and make special reference also to his remninder that the inhibitory effect of carbohydrate on ketone formation depends, not on the mnere existence of sufficient glucose, as glucose, in the blood (cf.