Ayrshire and Arran NHS Board
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
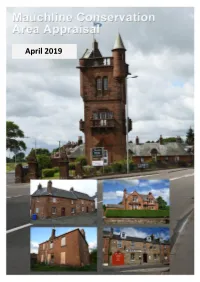
Mauchline Conservation Area Appraisal
April 2019 0 Contents 1. Introduction Context and Purpose of the Appraisal What Does Conservation Area Status mean? What Does a Conservation Area Appraisal do? 2. Statutory Designations Conservation Area Listed Buildings 3. Location and Setting 4. History and Development Early Development Eleventh to Sixteenth Century The Seventeenth Century The Eighteenth Century The Nineteenth and Twentieth Centuries Loudoun Spout Mauchline Cooperative Society 5. Conservation Area Appraisal Character and Land Use Topography Street Pattern and Access Routes Townscape Public and Private Open Space Boundary features Street Surfaces Trees and Landscaping Archaeological Assessments Building Scale and Form Landmarks Architectural Style Conservation Area Styles and Characteristics Building Types and Material Roofing and High Level Features Windows Doors and Shop Fronts Key Buildings Appraisal Recent Constructions within the Conservation Area Vacant Properties 6. Negative Factors 1 7. Assessment of Significance 8. Opportunities for Action and Enhancement Review of the Conservation Area Boundary Development Sites and Regeneration Managing Change Opportunities for Enhancement Environmental Initiatives APPENDICES Schedule of listed buildings Extract from East Ayrshire Local Development Plan Permitted development rights omitted from conservation areas 2 1. Introduction Context and Purpose of the Appraisal 1.1 Scottish Planning Policy (SPP) recognises the contribution cultural heritage makes to economy, identity and quality -

Winter Service Plan
1 INTRODUCTION The Ayrshire Roads Alliance within the Department of Neighbourhood Services is responsible for providing the winter service for East Ayrshire including:- Establishing standards Establishing treatment priorities Day to day direction of operations Monitoring performance Liaison with adjoining Councils and Emergency Services The Winter Service Plan was revised during the summer of 2011 to introduce the concepts and to follow the format provided in the code of practice 'Well Maintained Highways’, which was updated in May 2011. There is additional and more detailed information available (within the Ayrshire Roads Alliance Quality Management System) for personnel involved with the management and implementation of this Winter Service Plan. The Winter Service Plan will be reviewed annually and amended and updated before the 1st of October to include any revisions and changes considered necessary and appropriate to the service delivery. 2 CONTENTS Page Page 1.0 Statement of Policies and Responsibilities 04 5.0 Organisational Arrangements and 1.1 Statutory Obligations and Policy 04 Personnel 09 1.2 Responsibilities 04 5.1 Organisation chart and employee 1.3 Decision Making Process 05 responsibilities 09 1.4 Liaison arrangements with other authorities 05 5.2 Employee duty schedules, rotas and standby arrangements 10 1.5 Resilience Levels 06 5.3 Additional Resources 10 2.0 Quality 06 5.4 Training 10 2.1 Quality management regime 06 5.5 Health and safety procedures 10 2.2 Document control procedures 06 6.0 Plant, Vehicles and Equipment -
6. Supplementary Guidance
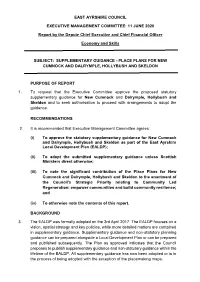
EAST AYRSHIRE COUNCIL EXECUTIVE MANAGEMENT COMMITTEE: 11 JUNE 2020 Report by the Depute Chief Executive and Chief Financial Officer Economy and Skills SUBJECT: SUPPLEMENTARY GUIDANCE - PLACE PLANS FOR NEW CUMNOCK AND DALRYMPLE, HOLLYBUSH AND SKELDON PURPOSE OF REPORT 1. To request that the Executive Committee approve the proposed statutory supplementary guidance for New Cumnock and Dalrymple, Hollybush and Skeldon and to seek authorisation to proceed with arrangements to adopt the guidance. RECOMMENDATIONS 2. It is recommended that Executive Management Committee agrees: (i) To approve the statutory supplementary guidance for New Cumnock and Dalrymple, Hollybush and Skeldon as part of the East Ayrshire Local Development Plan (EALDP); (ii) To adopt the submitted supplementary guidance unless Scottish Ministers direct otherwise; (iii) To note the significant contribution of the Place Plans for New Cumnock and Dalrymple, Hollybush and Skeldon to the enactment of the Council’s Strategic Priority relating to Community Led Regeneration: empower communities and build community resilience; and (iv) To otherwise note the contents of this report. BACKGROUND 3. The EALDP was formally adopted on the 3rd April 2017. The EALDP focuses on a vision, spatial strategy and key policies, while more detailed matters are contained in supplementary guidance. Supplementary guidance and non-statutory planning guidance can be prepared alongside a Local Development Plan or can be prepared and published subsequently. The Plan as approved indicates that the Council proposes to publish supplementary guidance and non-statutory guidance within the lifetime of the EALDP. All supplementary guidance has now been adopted or is in the process of being adopted with the exception of the placemaking maps. -

Kilmarnock Living
@^abVgcdX`A^k^c\ 6 H E : 8 > 6 A E A 6 8 : I D A > K : ! L D G @ ! A : 6 G C 6 C 9 : C ? D N ilZcineaVXZhndj]VkZid`cdlVWdji ^c@^abVgcdX`VcY:Vhi6ngh]^gZ The Dean Castle and Country Park, Kilmarnock River Ayr Way, from Glenbuck A phenomenal medieval experience. The Dean Castle is a A unique opportunity for walkers to experience the most glorious wonderfully well-preserved keep and surrounding buildings set in Ayrshire countryside on Scotland’s first source to sea walk. Starting beautifully manicured gardens and Country Park extending to more at Glenbuck, the birthplace of legendary football manager Bill than 480 acres. Shankley, the path travels 44 miles to the sea at Ayr. The Historic Old Town, Kilmarnock Burns House Museum, Mauchline Narrow lanes and unique little boutique shops. There are plenty of Situated in the heart of picturesque Mauchline, the museum was supermarkets and big stores elsewhere in Kilmarnock, but check the first marital home of Robert Burns and Jean Armour. As well as out Bank Street for something really different. being devoted to the life of Scotland’s national poet, the museum The Palace Theatre and Grand Hall, Kilmarnock has exhibits on the village’s other claims to fame – curling stones The creative hub of East Ayrshire. This is where everything from and Mauchline Box Ware. opera companies to pantomimes come to perform. And the hall is a great venue for private events. Kay Park, Kilmarnock Soon to be home to the Burns Monument Centre, this is one of Rugby Park, Kilmarnock the best of Kilmarnock’s public parks. -

East Ayrshire Local Development Plan Action Programme August 2019
East Ayrshire Local Development Plan Action Programme August 2019 update 1 Kilmarnock settlement wide placemaking map 2 Kilmarnock town centre placemaking map 3 Action Policy/Proposal Action Required Persons Responsible Timescales Progress as at August 2019 No (2017) 1 Development of Consideration of new Hallam Land Management/house 2017-2022 Renewal of Planning Permission in Principle Northcraig site 319H & planning application builders for Proposed Change of Use from Agricultural site 362M (Southcraig and implementation to Residential Use incorporating means of Drive) by Hallam Land access, open space, landscaping and Management. associated works was approved in 2015 Further application (17/0355/AMCPPP) was approved in February 2018. Development is now underway on site. The 1st phase of the development will involve the erection of 136 residential units by Barratt Homes. A further 2 phases will be developed in the future. No timescales are available for the 2 remaining phases at present. Discussions are ongoing with respect to the future development of site 262M. 2 Development of site A partnership Land owners/developer(s) 2020-2025 Small part of the site has been granted 152B at Meiklewood, between all owners approval for vehicle storage and office North Kilmarnock is required. accommodation associated with existing Alternatively, a single business on the site developer to take ownership of whole Development proposals expected to come site and develop forwards now that site 319H (Northcraigs) has primarily for commenced development and access through business/industrial site 153B (Rowallan Business Park) has been use. High resolved. infrastructure costs may mean the site is The long term strategy for the north of a longer term Kilmarnock, including this site, will be a key prospect and may issue to be explored through the preparation require a of LDP2. -

1943 the Digital Conversion of This Burns Chronicle Was Sponsored by Southern Scottish Counties Burns Association
Robert BurnsLimited World Federation Limited www.rbwf.org.uk 1943 The digital conversion of this Burns Chronicle was sponsored by Southern Scottish Counties Burns Association The digital conversion service was provided by DDSR Document Scanning by permission of the Robert Burns World Federation Limited to whom all Copyright title belongs. www.DDSR.com THE ROBER T BURNS ANNUAL AND CHRONICLE 1943 THE BURNS FEDERATION KILMARNOCK 1943 Price Three Shillings and Nine Pence "BURNS CHRONICLE" ADVERTISER CRAIG'S RESTAURANTS for MORNING COFFEE SNACKS · LUNCHEONS AFTERNOON TEA The Rhul The Gordon 123 7-19 Sauchiehall Gordon Street Street Branches throughout the CIty JAMES CRAIG (GLASGOW). LTO •• Woodlands Road. GLASGOW "BURNS CHRONICLE" ADVERTISER JEAN ARMOUR BURNS HOUSES CASTLE STREET, MAUCHLlNE AYRSH I RE Established in 1915 by the Glasgow and District Burns Association These Houses were purchased, repaired, and gifted to the Association by the late Mr. Charles R. Cowie, J.P., of Glasgow. They comprise the Burns House (in which the poet and Jean Armour began housekeeping in 1788), Dr. John M'Kenzie's House, and "Auld Nanse Tinnock's" (the "change-house" of Burns's poem "The Holy Fair"); and provide comfortable acco~modation for nine old ladies, who live rent and rate free and receive a small pension. A portion of the Burns House has been arranged as a Museum, which now contains numerous authentic relics of Jean Armour and the poet: these include the Armour Family Bible and several manuscripts of Burns. An Endowment Fund' for the maintenance of the Houses and the provision of the pensions is being formed. -

Table 1: Mid-2008 Population Estimates - Localities in Alphabetical Order
Table 1: Mid-2008 Population Estimates - Localities in alphabetical order 2008 Population Locality Settlement Council Area Estimate Aberchirder Aberchirder Aberdeenshire 1,230 Aberdeen Aberdeen, Settlement of Aberdeen City 183,030 Aberdour Aberdour Fife 1,700 Aberfeldy Aberfeldy Perth & Kinross 1,930 Aberfoyle Aberfoyle Stirling 830 Aberlady Aberlady East Lothian 1,120 Aberlour Aberlour Moray 890 Abernethy Abernethy Perth & Kinross 1,430 Aboyne Aboyne Aberdeenshire 2,270 Addiebrownhill Stoneyburn, Settlement of West Lothian 1,460 Airdrie Glasgow, Settlement of North Lanarkshire 35,500 Airth Airth Falkirk 1,660 Alexandria Dumbarton, Settlement of West Dunbartonshire 13,210 Alford Alford Aberdeenshire 2,190 Allanton Allanton North Lanarkshire 1,260 Alloa Alloa, Settlement of Clackmannanshire 20,040 Almondbank Almondbank Perth & Kinross 1,270 Alness Alness Highland 5,340 Alva Alva Clackmannanshire 4,890 Alyth Alyth Perth & Kinross 2,390 Annan Annan Dumfries & Galloway 8,450 Annbank Annbank South Ayrshire 870 Anstruther Anstruther, Settlement of Fife 3,630 Arbroath Arbroath Angus 22,110 Ardersier Ardersier Highland 1,020 Ardrishaig Ardrishaig Argyll & Bute 1,310 Ardrossan Ardrossan, Settlement of North Ayrshire 10,620 Armadale Armadale West Lothian 11,410 Ashgill Larkhall, Settlement of South Lanarkshire 1,360 Auchinleck Auchinleck East Ayrshire 3,720 Auchinloch Kirkintilloch, Settlement of North Lanarkshire 770 Auchterarder Auchterarder Perth & Kinross 4,610 Auchtermuchty Auchtermuchty Fife 2,100 Auldearn Auldearn Highland 550 Aviemore Aviemore -

East Ayrshire Local Development Plan Non-Statutory Planning Guidance
East Ayrshire Council East Ayrshire Local Development Plan Non-statutory Planning Guidance Bank Street and John Finnie Street Conservation Area Appraisal and Management Plan 2007 Austin-Smith:Lord LLP East Ayrshire Council 5th December 2007 Kilmarnock John Finnie Street and Page 1 of 135 207068 Bank Street Conservation Area Conservation Area Appraisal and Management Plan CONTENTS 1.0 Introduction 2.0 Statutory Designations 3.0 Planning and Other Policies 4.0 History and Context 5.0 Architectural Appraisal 6.0 Townscape and Urban Realm Appraisal 7.0 Archaeological Assessment 8.0 Assessment of Significance 9.0 Vulnerability and Related issues 10.0 Conservation and Management Guidelines 11.0 Implementation and Review APPENDICES Appendix One - Outstanding Conservation Area Boundaries and Properties Appendix Two - Statutory Designations Appendix Three - Buildings Gazetteer Appendix Four - Archaeological Gazetteer Appendix Five - Definitions Austin-Smith: Lord LLP 296 St. Vincent Street, Glasgow. G2 5RU t. 0141 223 8500 f. 0141 223 8501 e: [email protected] June 2007 Austin-Smith:Lord LLP is a limited liability partnership registered in England and Wales with registered number OC315362. Austin-Smith:Lord LLP East Ayrshire Council 5th December 2007 Kilmarnock John Finnie Street and Page 2 of 135 207068 Bank Street Conservation Area Conservation Area Appraisal and Management Plan Austin-Smith:Lord LLP East Ayrshire Council 5th December 2007 Kilmarnock John Finnie Street and Page 3 of 135 207068 Bank Street Conservation Area Conservation Area Appraisal and Management Plan 1.0 INTRODUCTION th Figure 1: John Finnie Street from Station Brae and the North, Early 20 Century (author’s collection) 1.1 The character of Kilmarnock is shaped by the quality and diversity of its historic buildings and streetscape. -

Thecommunityplan
EAST AYRSHIRE the community plan planning together working together achieving together Contents Introduction 3 Our Vision 3 Our Guiding Principles 4 The Challenges 8 Our Main Themes 13 Promoting Community Learning 14 Improving Opportunities 16 Improving Community Safety 18 Improving Health 20 Eliminating Poverty 22 Improving the Environment 24 Making the Vision a Reality 26 Our Plans for the next 12 years 28 Our Aspirations 28 2 Introduction Community planning is about a range of partners in the public and voluntary sectors working together to better plan, resource and deliver quality services that meet the needs of people who live and work in East Ayrshire. Community planning puts local people at the heart of delivering services. It is not just about creating a plan or a vision but about jointly tackling major issues such as health, transport, employment, housing, education and community safety. These issues need a shared response from, and the full involvement of, not only public sector agencies but also local businesses, voluntary organisations and especially local people. The community planning partners in East Ayrshire are committed to working together to make a real difference to the lives of all people in the area. We have already achieved a lot through joint working, but we still need to do a lot more to make sure that everybody has a good quality of life. Together, those who deliver services and those who live in our communities will build on our early success and on existing partnerships and strategies to create a shared understanding of the future for East Ayrshire. -

Stewarton Road
The Avenue Street / Graham Terrace portion of the town centre is a designated Conservation Area and it is proposed that the conservation area should be extended to cover the High Street area of the town. It is recognised that the needs of the community, in so far as leisure activities are concerned, are likely to change in the future and that this warrants a greater channelling of resources into the area. The most pressing priorities are the expansion of secondary education facilities in the town, the provision of new leisure facilities at an appropriate location to serve the Glasgow Link Corridor and the upgrading of the B778 Fenwick / Stewarton road. It is intended that developer contributions will be specifically directed towards funding these particular initiatives. Stewarton 2017 which reflects anticipated demand and is commensurate with the designation of the town as a Stewarton is a thriving small commuter town with a Service Centre and as a strategic expansion location. population of 6,582 in 2001 which has undergone Care has been taken, however, to ensure that future rapid expansion in recent years. The town is within development is in keeping with and respects the easy reach of both Kilmarnock and Irvine and is also character of the community and the capability of the strategically located on the main Glasgow to Dumfries landscape to accommodate the size and scale of railway line. development proposed. In this regard, potential The settlement is identified as a Service Centre in the developers of the strategic expansion locations Ayrshire Joint Structure Plan and this designation is identified in the plan will be required to prepare also reflected in the local plan. -

East Ayrshire Council
EAST AYRSHIRE COUNCIL GOVERNANCE AND SCRUTINY COMMITTEE: 24 SEPTEMBER 2010 DERELICT BUILDINGS REPORT Report by Depute Chief Executive / Executive Director of Neighbourhood Services 1. PURPOSE OF REPORT 1.1 Further to the Governance and Scrutiny Committee of 19 March 2010, the purpose of this report is to present to Committee a report that identifies and provides relevant information on those derelict buildings within East Ayrshire which are known to the Council and which present cause for concern. 1.2 Details have been included of cases that officers have been involved with over the last 5 years as well as those that remain of concern. Details are also included within appendix 2 of those properties within the Buildings at Risk Register, (BARR). 2. DERELICT BUILDINGS 2.1 Those properties detailed within appendix 1 to this report include specifically buildings that are in a derelict condition, and not buildings which are merely untidy in their appearance or land which is similarly untidy. For the purposes of this exercise, “derelict” has been taken to comprise properties where there is a significant deterioration in the physical fabric of the building; for example by way of damage to doors, windows, elevations or roof such as to allow ingress by the weather or to encourage vandalism. 2.2 The properties referred to in this report do not necessarily represent the entirety of derelict buildings within the district. They are those properties in respect of which the Planning and Economic Development Service has received complaints or which are subject of enforcement investigation. The buildings lie within the following settlements: Catrine, Cumnock, Dalmellington, Darvel, Galston, Hurlford, Kilmarnock, Kilmaurs, Mauchline, Muirkirk, New Cumnock, Newmilns, Patna, Rankinston and Waterside (Patna). -
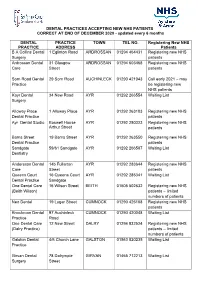
DENTAL PRACTICES ACCEPTING NEW NHS PATIENTS CORRECT at END of DECEMBER 2020 - Updated Every 6 Months
DENTAL PRACTICES ACCEPTING NEW NHS PATIENTS CORRECT AT END OF DECEMBER 2020 - updated every 6 months DENTAL PRACTICE TOWN TEL NO. Registering New NHS PRACTICE ADDRESS Patients B A Collins Dental 1 Eglinton Road ARDROSSAN 01294 464431 Registering new NHS Surgery patients Ardrossan Dental 31 Glasgow ARDROSSAN 01294 603468 Registering new NHS Care Street patients Sorn Road Dental 29 Sorn Road AUCHINLECK 01290 421043 Call early 2021 – may Practice be registering new NHS patients Kayr Dental 34 New Road AYR 01292 266554 Waiting List Surgery Alloway Place 1 Alloway Place AYR 01292 263103 Registering new NHS Dental Practice patients Ayr Dental Studio Boswell House AYR 01292 280323 Registering new NHS Arthur Street patients Barns Street 19 Barns Street AYR 01292 263550 Registering new NHS Dental Practice patients Sandgate 59/61 Sandgate AYR 01292 266587 Waiting List Dentistry Andersson Dental 14b Fullarton AYR 01292 283644 Registering new NHS Care Street patients Queens Court 16 Queens Court AYR 01292 285341 Waiting List Dental Practice Sandgate One Dental Care 16 Wilson Street BEITH 01505 502632 Registering new NHS (Beith Wilson) patients – limited numbers of patients Neo Dental 19 Lugar Street CUMNOCK 01290 425108 Registering new NHS patients Knockroon Dental 97 Auchinleck CUMNOCK 01290 420048 Waiting List Practice Road One Dental Care 12 New Street DALRY 01294 832524 Registering new NHS (Dalry Practice) patients – limited numbers of patients Galston Dental 4/6 Church Lane GALSTON 01563 820235 Waiting List Practice Girvan Dental 78 Dalrymple