Post-Lumbar Puncture Headache—Does Hydration Before Puncture Prevent Headache and Affect Cerebral Blood Flow?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lumbar Puncture (LP)
Lumbar puncture (LP) What is a lumbar puncture (LP)? Who will perform this test? An LP is a common and routine procedure, also A doctor trained in performing this procedure known as a spinal tap, where a very small will do the LP. A trained children’s nurse will hold needle is inserted through the base of the spine your infant in the appropriate position (which to collect a sample of the fluid surrounding the is lying on their side curled up in a tight ball). brain and spinal cord. This fluid is called Another team member may also be present to cerebrospinal fluid (CSF). help. Why do we need to do this? Can you be present during the LP? LP is the only way to confirm a case of Yes, you can tell the team that you would like to meningitis (swelling of the lining of the brain be present. However, many parents find it caused by an infection in the CSF). distressing to see any procedures being done on their baby and would rather not be present. This National guidelines strongly recommended that is perfectly understandable. Please let the team an LP is done alongside other routine know and they will usually agree to whatever investigations, such as blood and urine tests, works best for you but be aware that it is best to look for signs of infection if meningitis is to be quiet so the doctor can concentrate on the suspected. This is a routine and very important procedure. investigation. Is it a painful procedure? Getting a sample of CSF will help Drs to find out An LP is an uncomfortable procedure similar to if your child has meningitis and if what is a blood test or drip being inserted. -

The Clinical Effect of Lumbar Puncture in Normal Pressure Hydrocephalus
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.45.1.64 on 1 January 1982. Downloaded from Journal of Neurology, Neurosurgery, and Psychiatry 1982;45:64-69 The clinical effect of lumbar puncture in normal pressure hydrocephalus C WIKKELS0, H ANDERSSON, C BLOMSTRAND, G LINDQVIST From the Department of Neurology and Neurosurgery, Sahlgren Hospital, University of Goteborg, Sweden SUMMARY Owing to all the difficulties involved in selecting patients with normal pressure hydro- cephalus for shunt-operation, a cerebrospinal fluid-tap-test (CSF-TT) is introduced. Psychometric and motor capacities of the patients are measured before and after lumbar puncture and removal of 40-50 ml CSF. Patients fulfilling criteria for normal pressure hydrocephalus were compared to patients with dementia and atrophy shown by computed tomography. Normal pressure hydro- cephaluspatients showed temporary improvement after lumbar puncture. The extent ofthe temporary improvement appeared to be well correlated with the improvement after shunt operation. Accord- ingly, the CSF-TT seems to be of value when selecting those patients who will probably benefit from a shunt operation. The syndrome of normal pressure hydrocephalus is pressure by lumbar puncture caused both subjective Protected by copyright. characterised by gait disturbance, progressive mental and objective temporary improvement in some deterioration and urinary incontinence.' Particularly patients with normal pressure hydrocephalus.10 16 17 noteworthy is the complex gait disturbance with Such patients also improved after CSF-shunting. spastic-ataxia, extrapyramidal components, and However, no details have been given about the commonly dyspraxia of gait.2 In addition, there is in amount of CSF which was drained or to what degree typical cases mental "slowing up" with lack of the CSF pressure was lowered. -

Ventriculoperitoneal Shunts in the Emergency Department: a Review
Open Access Review Article DOI: 10.7759/cureus.6857 Ventriculoperitoneal Shunts in the Emergency Department: A Review Michael Ferras 1 , Nicholas McCauley 1 , Trilok Stead 2 , Latha Ganti 3, 4, 5 , Bobby Desai 6 1. Emergency Medicine, Ocala Regional Medical Center, University of Central Florida, Ocala, USA 2. Emergency Medicine, Trinity Preparatory School, Winter Park, USA 3. Emergency Medicine, Envision Physician Services, Orlando, USA 4. Emergency Medicine, University of Central Florida College of Medicine/Hospital Corporation of America Graduate Medical Education Consortium of Greater Orlando, Orlando, USA 5. Emergency Medicine, Polk County Fire Rescue, Bartow, USA 6. Emergency Medicine, Ocala Regional Medical Center, University of Central Florida College of Medicine, Ocala, USA Corresponding author: Latha Ganti, [email protected] Abstract In this paper, we review the indications, complications, and pitfalls associated with ventriculoperitoneal (VP) shunts. As most VP shunt problems initially present to the emergency department, it is important for emergency physicians to be well-versed in managing them. In the article, the possible reasons for shunt failure are explored and summarized using an infographic. We also examine potential clinical presentations of VP shunt failure. Categories: Emergency Medicine, Neurosurgery Keywords: ventriculoperitoneal shunts Introduction And Background Emergency department physicians usually see a large number of patients with medical maladies managed by the aid of instrumentation or hardware such as a ventriculoperitoneal (VP) shunt. While patients have shunts placed for multiple reasons, it is important for emergency service providers to know how to evaluate, troubleshoot, and treat those with VP shunt complications. An estimated 30,000 VP shunt procedures are performed yearly in the United States [1]. -

Role of Lumbar Puncture in Traumatic Brain Injury
308 Indian Journal of Public Health Research & Development, April-June 2021, Vol. 12, No. 2 Role of Lumbar Puncture In Traumatic Brain Injury Ranjeet Kumar Jha1, Rachna Gupta2 1Assistant Professor, Department of Neurosurgery, 2Professor, Department of Surgery, Shyam Shah Medical College, Rewa Abstract Background: Cerebrospinal fluid (CSF) drainage via ventricular puncture is an established therapy of elevated intracranial pressure (ICP). In contrast, lumbar CSF removal is believed to be contraindicated with intracranial hypertension. Method: We investigated the safety and efficacy of lumbar CSF drainage to decrease refractory elevated ICP in a small cohort of patients with traumatic brain injury (TBI). A score (0–8 points) was used to assess computed tomography (CT) images for signs of herniation and for patency of the basal cisterns. All patients received lumbar CSF drainage either as a continuous drainage or as a single lumbar puncture (LP). Type and method of CSF drainage, mean ICP 24 h prior and after CSF removal, and adverse events were documented. Outcome was assessed after 3 months (with dichotomized Glasgow outcome scale). Results: Eight patients were evaluated retrospectively. n = 5 suffered a moderate, n = 2 a severe TBI (one Glasgow coma score not documented). The CT score was ≥5 in all patients prior to LP and decreased after puncture without clinical consequences in two patients. The amount of CSF removal did not correlate with score changes (P = 0.45). CSF drainage led to a significant reduction of mean ICP (from 22.3 to 13.9 mmHg, P = 0.002). Continuous drainage was more effective than a single LP. Three of eight patients reached a favorable outcome. -
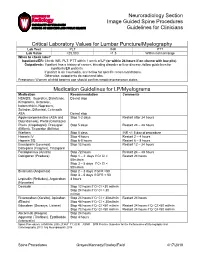
Neuroradiology Section Image Guided Spine Procedures Guidelines for Clinicians
Neuroradiology Section Image Guided Spine Procedures Guidelines for Clinicians Critical Laboratory Values for Lumbar Puncture/Myelography Lab Test PLT INR PTT Lab Value >25,000 <1.5 Within normal range When to check labs? Inpatients/ER: Check INR, PLT, PTT within 1 week of LP (or within 24 hours if on chemo with low plts) Outpatients: If patient has a history of cancer, bleeding disorder or liver disease, follow guidelines for inpatients/ER patients If patient is on Coumadin, see below for specific recommendations. Otherwise, outpatients do not need labs. Pregnancy: Women of child bearing age should confirm negative pregnancy status Medication Guidelines for LP/Myelograms Medication Recommendation Comments NSAIDS: Ibuprofen, Diclofenac, Do not stop Ketoprofen, Ketorolac, Indomethicin, Naproxen, Sulindac, Diflunisal, Celecoxib ASA Do not stop Aggrenox/persantine (ASA and Stop 1-2 days Restart after 24 hours Dipyridamole), Pletal (Cilostazol) Plavix (Clopidogrel), Prasugrel Stop 5 days Restart 24 – 48 hours (Effient), Ticagrelor (Brilinta) Warfarin Stop 5 days INR <1.5 day of procedure Heparin IV Stop 4 hours Restart 2 – 4 hours Heparin SQ Stop 6-8 hours Restart 6 – 8 hours Enoxaparin (Lovenox), Stop 12 hours Restart 12 – 24 hours Dalteparin (Fragmin), Tinzaparin Fondaparinux (Arixtra) Stop 72 hours Restart 24 – 48 hours Dabigatran (Pradaxa) Stop 1 – 2 days if Cr Cl > Restart 24 hours 50ml/min Stop 3 – 5 days if Cr Cl < 50ml/min Bivalrudin (Angiomax) Stop 2 – 3 days if GFR >50 Stop 3 – 5 days if GFR < 50 Lepirudin (Refludan), Argatroban 4 hours (Novastan) Desrudin Stop 12 hours if Cr Cl >30 ml/min Stop 24 hours if Cr Cl < 30 ml/min Rivaroxaban (Xarelto), Apixaban Stop 24 hours if Cr Cl > 30ml/min Restart 24 hours (Eliquis) Stop 48 hours if Cr Cl < 30ml/min Edoxaban (Savasya, Lixiana) Stop 48 hours if Cr Cl >50 ml/min Restart 24 hours if Cr Cl >50 ml/min Stop 72 hours if Cr Cl <50 ml/min Restart 24 hours if Cr Cl <50 ml/min Abciximab (Reopro) Stop 24 hours Aggrastat (Tirofiban), Eptifibatide Stop 4 hours (Intergrelin) Spinal Procedures. -
Ventriculoperitoneal Shunt Occlusion and Cranioplasty. a Case Report
Ventriculoperitoneal shunt occlusion and cranioplasty. A case report Lívio Pereira de Macêdo, Arlindo Ugulino Netto, Juan Pablo Borges R. Maricevich, Nivaldo S. Almeida, Hildo Rocha Cirne Azevedo-Filho DOI: 10.33962/roneuro-2020-063 Romanian Neurosurgery (2020) XXXIV (1): pp. 405-410 DOI: 10.33962/roneuro-2020-063 www.journals.lapub.co.uk/index.php/roneurosurgery Ventriculoperitoneal shunt occlusion and cranioplasty. A case report Lívio Pereira de Macêdo1, Arlindo Ugulino Netto1, Juan Pablo Borges Rodrigues Maricevich2, Nivaldo S. Almeida1, Hildo Rocha Cirne Azevedo-Filho1 1 Department of Neurosurgery, Hospital da Restauração, Recife, Pernambuco, BRAZIL 2 Department of Plastic Surgery, Hospital da Restauração, Recife, Pernambuco, Brazil ABSTRACT Keywords Decompressive craniectomy (DC) is an urgent neurosurgical procedure, effective in cranioplasty, the reduction of intracranial pressure (ICP) in patients with elevated ICP and in VPS, complications of brain infarction that do not respond to clinical treatment; traumatic VPS Occlusion brain injury (TBI); intracerebral haemorrhage (ICH) and aneurysmal intracerebral haemorrhage. Symptomatic hydrocephalus is present in 2 to 29% of patients who undergo craniectomy. They may require a ventriculoperitoneal shunt (VPS). The literature does not yet show standard management of cranioplasty in patients who have previously undergone a shunt, showing evidence of sinking skin flap syndrome. This case shows parenchymal expansion after VPS occlusion and cranioplasty in the Corresponding author: Lívio Pereira de Macêdo patient’s profile. The 23-year-old male patient, right-handed, went to the hospital in January 2017 due to severe traumatic brain injury following multiple traumas. The Department of Neurosurgery, patient underwent urgent DC surgery for the management of elevated ICP. -
Relevant Code and Sample Claim Form Guide
RELEVANT CODE AND SAMPLE CLAIM FORM GUIDE June 2020 Edition INDICATION SPINRAZA® (nusinersen) is indicated for the treatment of spinal muscular atrophy (SMA) in pediatric and adult patients. SELECTED IMPORTANT SAFETY INFORMATION Coagulation abnormalities and thrombocytopenia, including acute severe thrombocytopenia, have been observed after administration of some antisense oligonucleotides. Patients may be at increased risk of bleeding complications. Please see additional Important Safety Information on page 11 and accompanying full Prescribing Information. INTRODUCTION This guide provides an overview of best practices to assist with coding for procedures related to SPINRAZA administration and ancillary services (if needed). It also provides examples of claim forms and guidance on how to complete them. For a more comprehensive presentation of applicable codes and claim forms, refer to the Guide to SPINRAZA Reimbursement, available at SPINRAZA-hcp.com or through your Biogen representative. ALWAYS CHECK YOUR PATIENT’S PLAN FOR COVERAGE AND CODING GUIDANCE Remember, coding and billing recommendations may vary by payer. Your practice or facility should check directly with the patient’s payer(s) for guidance on the appropriate codes to use to facilitate claim processing for SPINRAZA, its administration, and any ancillary services. Biogen field representatives are available to answer questions and further support the reimbursement process. LINKS TO IMPORTANT RESOURCES Regarding Medicare Parts A and B, coverage for SPINRAZA administration is determined through an LCD. For links to LCDs for MACs in your state, visit the CMS website at www.cms.gov/Medicare/Coverage/DeterminationProcess/LCDs. A map of MACs can be found at www.cms.gov/Medicare/Medicare-Contracting/Medicare-Administrative-Contractors/Who-are-the-MACs. -
Public Use Data File Documentation
Public Use Data File Documentation Part III - Medical Coding Manual and Short Index National Health Interview Survey, 1995 From the CENTERSFOR DISEASECONTROL AND PREVENTION/NationalCenter for Health Statistics U.S. DEPARTMENTOF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics CDCCENTERS FOR DlSEASE CONTROL AND PREVENTlON Public Use Data File Documentation Part Ill - Medical Coding Manual and Short Index National Health Interview Survey, 1995 U.S. DEPARTMENT OF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics Hyattsville, Maryland October 1997 TABLE OF CONTENTS Page SECTION I. INTRODUCTION AND ORIENTATION GUIDES A. Brief Description of the Health Interview Survey ............. .............. 1 B. Importance of the Medical Coding ...................... .............. 1 C. Codes Used (described briefly) ......................... .............. 2 D. Appendix III ...................................... .............. 2 E, The Short Index .................................... .............. 2 F. Abbreviations and References ......................... .............. 3 G. Training Preliminary to Coding ......................... .............. 4 SECTION II. CLASSES OF CHRONIC AND ACUTE CONDITIONS A. General Rules ................................................... 6 B. When to Assign “1” (Chronic) ........................................ 6 C. Selected Conditions Coded ” 1” Regardless of Onset ......................... 7 D. When to Assign -

Transcranial Doppler for Monitoring and Evaluation of Idiopathic Intracranial Hypertension
Published online: 2020-05-02 THIEME Original Article 309 Transcranial Doppler for Monitoring and Evaluation of Idiopathic Intracranial Hypertension Pradeep R1 Dhananjay Gupta1 Nikith Shetty2 Anjani Kumar Bhushan1 Krishna Haskar1 Sujana Gogineni1 Anish Mehta1 Mahendra Javali1 Purshottam T. Acharya1 Rangasetty Srinivasa1 1Department of Neurology, Ramaiah Medical College, Bengaluru, Address for correspondence Dhananjay Gupta, MD, Department of Karnataka, India Neurology, Ramaiah Medical College and Hospitals, New BEL Road, 2Department of Neurology, Kasturba Medical College, Manipal, M S Ramaiah Nagar, MSRIT Post,Bengaluru 560054, Karnataka, India Karnataka, India (e-mail: [email protected]). J Neurosci Rural Pract 2020;11:309–314 Abstract Background Idiopathic intracranial hypertension (IIH) is a disorder of unknown origin, characterized by features of raised intracranial pressure (ICP). Existing literature is inconclusive about the role of transcranial Doppler (TCD) in the management of IIH. Objective To study the TCD changes in IIH patients, pre- and post-cerebrospinal fluid (CSF) drainage. Materials and Methods This was a prospective study, conducted between July 2017 and December 2019, in a tertiary care referral center in South India. Sixteen consec- utive patients, suspected to have IIH, underwent magnetic resonance imaging ofthe brain, a baseline TCD, and lumbar puncture with CSF drainage and pressure moni- toring. Post-CSF drainage, TCD was repeated and mean flow velocities, peak systolic velocities, end-diastolic velocities, and pulsatility index (PI), in the middle cerebral artery (MCA), vertebral artery, and basilar artery (BA) were noted. Thirteen patients had elevated CSF pressure, and fulfilled the diagnostic criteria for IIH. These patients were included in the final analysis and pre- and post-CSF drainage TCD blood flow velocities and PI were compared. -

Lumbar Puncture
A fact sheet for patients and carers Lumbar puncture This fact sheet provides information on lumbar punctures. Our fact sheets are designed as general introductions to each subject and are intended to be concise. Each person is affected differently and you should speak with your doctor or specialist for individual advice. What is a lumbar puncture? A lumbar puncture involves extracting some of the fluid that surrounds your brain and spine (known as cerebrospinal fluid or CSF). It is sometimes referred to as a spinal tap. Often, a lumbar puncture is done because doctors need to do some tests on the CSF to help them make a diagnosis. Doctors may look for changes in the fluid that could indicate infection or bleeding, or unusual or uncommon cells that could be a sign of a neurological disorder. They will also check the pressure of the CSF. Less frequently, a lumbar puncture can be done as a means of treatment if a person has too much CSF, and the pressure of the fluid around the brain and spine is too high. What happens before a procedure? A lumbar puncture is likely to take 30 minutes to an hour, so you don’t usually have to stay in hospital overnight. There is no need to stop eating and drinking before the procedu re, and you should continue to take any medication as prescribed, unless you have been told otherwise by your doctor. If you are taking any medication to thin your blood (anticoagulants) it is important that you inform the hospital before your appointment. -

Neurosurgical CSF Diversion in Idiopathic Intracranial Hypertension: a Narrative Review
life Review Neurosurgical CSF Diversion in Idiopathic Intracranial Hypertension: A Narrative Review Geraint J. Sunderland 1,2,*, Michael D. Jenkinson 2,3, Elizabeth J. Conroy 4, Carrol Gamble 4 and Conor L. Mallucci 1,5 1 Department of Paediatric Neurosurgery, Alder Hey Children’s Hospital NHS Foundation Trust, Liverpool L12 2AP, UK; [email protected] 2 Department of Neurosurgery, The Walton Centre NHS Foundation Trust, Liverpool L9 7LJ, UK; [email protected] 3 Institute of Systems, Molecular and Integrative Biology, University of Liverpool, Liverpool L69 7BE, UK 4 Liverpool Clinical Trials Centre, University of Liverpool, Liverpool, L69 3GL, UK; [email protected] (E.J.C.); [email protected] (C.G.) 5 Faculty of Health and Life Sciences, University of Liverpool, Liverpool L69 7TX, UK * Correspondence: [email protected] Abstract: The prevalence of idiopathic intracranial hypertension (IIH), a complex disorder, is in- creasing globally in association with obesity. The IIH syndrome occurs as the result of elevated intracranial pressure, which can cause permanent visual impairment and loss if not adequately managed. CSF diversion via ventriculoperitoneal and lumboperitoneal shunts is a well-established strategy to protect vision in medically refractory cases. Success of CSF diversion is compromised by high rates of complication; including over-drainage, obstruction, and infection. This review outlines currently used techniques and technologies in the management of IIH. Neurosurgical CSF diversion Citation: Sunderland, G.J.; is a vital component of the multidisciplinary management of IIH. Jenkinson, M.D.; Conroy, E.J.; Gamble, C.; Mallucci, C.L. Keywords: idiopathic intracranial hypertension; pseudotumour cerebri; cerebrospinal fluid; ventricu- Neurosurgical CSF Diversion in loperitoneal shunt; lumboperitoneal shunt; programmable valve; anti-siphon device; neurosurgery Idiopathic Intracranial Hypertension: A Narrative Review. -

Multiple Organ Support Introduction to Multiple Organ Support, D
IMANCUAGEMENT & PRACTICE IntensIve care - emergency medIcIne - anaesthesIology VOLUME 18 - ISSUE 1 - SPRING 2018 sPECIAl suPPlEMENTs Hamilton Medical symposium: Optimising patient-ventilator synchronisation Nestlé Nutrition Institute symposium: Nutritional challenges in ICU patients Multiple organ support Introduction to multiple organ support, D. Abrams et al. From multiple organ support therapy (most) to extracorporeal organ support (ecos) in critically ill patients, C. Ronco et al. chronic respiratory dialysis, D. Abrams et al. Understanding LVAD & artificial hearts, N. Aissaoui et al. Plus co2 in the critically ill, L. Morales- emergencies, I. Gonzalez Being an expert witness, Quinteros et al. a novel communication device J. Dale-Skinner Immune dysfunction in sepsis, for tracheostomy IcU patients, role of the chaplain in the IcU, V. Herwanto et al. F. Howroyd K. Jones hypothermia in neurocritical care the critical care resuscitation developing new approaches to patients other than cardiac arrest, Unit, L.I. Losonczy et al. patient safety, J. Welch et al. R. Helbok & R. Beer variation in end-of-life care, how to provide better intensive Intracranial pressure monitoring A. Michalsen care? J. Takala devices, S. Patil & F. Fadhlillah simulate or not to simulate? caring for critically ill immunocom- complications of decompressive M. Poggioli et al. promised patients, E. Azoulay craniectomy in neurological ©For personal and private use only. Reproduction must be permitted by the copyright holder. Email to [email protected]. must be permitted use only. Reproduction and private ©For personal icu-management.org @ICU_Management 52 MATRIX Isabel González Attending Physician Intensive Care Unit Complications of Complejo Hospitalario De León Altos de Nava Spain decompressive craniectomy migonzalezpe@saludcastillay- leon.es in neurological emergencies a brief report There are a number of complications related to the use of decompressive surgery.