Service Redesign Case Study 1: November 2014
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

BERKSHIRE PROSPECTUS AMBITION, COLLABORATION and GROWTH Thames Valley Berkshire LEP Berkshire Prospectus Local Authorities As Well As Other Key Stakeholders
BERKSHIRE PROSPECTUS AMBITION, COLLABORATION AND GROWTH 02 THE BERKSHIRE Berkshire Prospectus Berkshire PROSPECTUS THE OPPORTUNITIES IN THIS PROSPECTUS It is no coincidence that this prospectus for Berkshire has been released in tandem with the Thames Valley Berkshire Local Enterprise Partnership (LEP) Recovery and REPRESENT A CHANCE Renewal Plan. The two documents sit alongside each other, evidencing the formidable collaborative nature of how TO RESET POST COVID the LEP is working in partnership with the six Berkshire Local Authorities as well as other key stakeholders. AND MAKE BERKSHIRE This prospectus clearly identifies several key schemes and projects which, when delivered, will greatly enhance Berkshire’s appeal as a place to live and EVEN BETTER work in the years ahead. The projects highlighted in this prospectus represent unique opportunities for new investment that will appeal to a wide range of partners, locally, regionally and nationally. The LEP and Local Authorities will work alongside private and public sector colleagues to facilitate the development and successful delivery of these great opportunities. COLLABORATIVE WORKING We should highlight the constructive partnership between the Local Authorities and the LEP, who together have forged a great working relationship with One Public Estate (OPE). Established in 2013, OPE now works nationally with more than 300 councils.These projects are transforming local communities and public services right across the country. They provide technical support and funding to councils to deliver ambitious property and place-focused programmes in collaboration with central government and other public sector partners. Thames Valley Berkshire LEP Berkshire Thames Valley 03 As highlighted in the Recovery and Renewal Plan, Thames Valley Berkshire is more than the sum of its parts. -

VISION Barnstable Berkshire Bristol Dukes Essex Franklin
Massachusetts Division of Insurance Annual Report Membership in VISION Insured Preferred Provider Plans by County as of December 31, 2006 VISION Barnstable Berkshire Bristol Dukes Essex Franklin Hampden Hampshire Middlesex Nantucket Norfolk Plymouth Suffolk Worcester MA 1 Insured Preferred Provider Plan Members Members at Members at Members at Members at Members at Members at Members at Members at Members at Members at Members at Members at Members at Members at Total 2006 By County End of 2006 End of 2006 End of 2006 End of 2006 End of 2006 End of 2006 End of 2006 End of 2006 End of 2006 End of 2006 End of 2006 End of 2006 End of 2006 End of 2006 Members 2 1 AIG Life Insurance Company 000000000000000 2 (The) Chesapeake Life Insurance Company 000000000010001 3 Columbian Life Insurance Company 0 0 0 13 106 0 0 0 216 0 90 16 41 76 558 4 Combined Insurance Company of America 48 20 422 0 1,288 351 290 246 2,964 0 1,498 422 800 1,417 9,766 5 Connecticut General Life Insurance Company 000000000000000 6 Fidelity Security Insurance Company 169 16 907 6 725 405 665 2,234 2,093 0 2,791 1,503 1,332 1,793 14,639 7 (The) Guardian Life Insurance Company of America 117 0 0 0 160 11 0 9 2,221 0 1,026 0 639 353 4,536 8 Massachusetts Vision Service Plan, Inc. 0 2,860 2,240 83 11,308 0 1,109 279 101,555 0 16,472 3,428 45,968 1,931 187,233 9 (The) MEGA Life and Health Insurance Company 298 96 385 30 563 71 223 107 992 45 472 354 329 371 4,336 10 Mid-West Life Insurance Company of Tennessee 618 47 290 27 656 44 131 71 968 30 408 426 188 470 4,374 11 National Union Fire Insurance Co. -

Chanukah Cooking with Chef Michael Solomonov of the World
Non-Profit Org. U.S. POSTAGE PAID Pittsfield, MA Berkshire Permit No. 19 JEWISHA publication of the Jewish Federation of the Berkshires, serving V the Berkshires and surrounding ICE NY, CT and VT Vol. 28, No. 9 Kislev/Tevet 5781 November 23 to December 31, 2020 jewishberkshires.org Chanukah Cooking with Chef The Gifts of Chanukah Michael Solomonov of the May being more in each other’s presence be among World-Famous Restaurant Zahav our holiday presents On Wednesday, December 2 at 8 p.m., join Michael Solomonov, execu- tive chef and co-owner of Zahav – 2019 James Beard Foundation award winner for Outstanding Restaurant – to learn to make Apple Shrub, Abe Fisher’s Potato Latkes, Roman Artichokes with Arugula and Olive Oil, Poached Salmon, and Sfenj with Cinnamon and Sugar. Register for this live virtual event at www.tinyurl.com/FedCooks. The event link, password, recipes, and ingredient list will be sent before the event. Chef Michael Solomonov was born in G’nai Yehuda, Israel, and raised in Pittsburgh. At the age of 18, he returned to Israel with no Hebrew language skills, taking the only job he could get – working in a bakery – and his culinary career was born. Chef Solomonov is a beloved cham- pion of Israel’s extraordinarily diverse and vibrant culinary landscape. Chef Michael Solomonov Along with Zahav in Philadelphia, Solomonov’s village of restaurants include Federal Donuts, Dizengoff, Abe Inside Fisher, and Goldie. In July of 2019, Solomonov brought BJV Voluntary Subscriptions at an another significant slice of Israeli food All-Time High! .............................................2 culture to Philadelphia with K’Far, an Distanced Holidays? Been There, Israeli bakery and café. -
Berkshire Passenger Rail Station Location and Design Analysis, Draft for Public Comment—August 2014
BERKSHIRE PASSENGER RAIL STATION LOCATION AND DESIGN ANALYSIS, DRAFT FOR PUBLIC COMMENT—AUGUST 2014 BERKSHIRE PASSENGER RAIL STATION LOCATION AND DESIGN ANALYSIS, DRAFT FOR PUBLIC COMMENT—AUGUST 2014 ACKNOWLEDGEMENTS Staff, Elected Officials, and Residents of the Berkshire Line Communities Karen Christensen and the Bring Back the Trains Campaign Bill Palmer, MassDOT Dustin Rhue, MassDOT Gary Sheppard, Berkshire Regional Transit Authority Bob Malnati, Berkshire Regional Transit Authority John R. Hanlon Jr., Housatonic Railroad Company Colin Pease, Housatonic Railroad Company Deborah Menette,Housatonic Railroad Company Berkshire Regional Planning Commission Nathaniel Karns, AICP, Executive Director Thomas Matuszko, AICP, Assistant Director Clete Kus, AICP, Transportation Manager Mark Maloy, GIS, Data and IT Manager Brian Domina, Senior Planner Patricia Mullins, Senior Planner Gwen Miller, Planner Jaclyn Pacejo, Planner BERKSHIRE PASSENGER RAIL STATION LOCATION AND DESIGN ANALYSIS Page 1 ACKNOWLEDGEMENTS This page intentionally left blank. BERKSHIRE PASSENGER RAIL STATION LOCATION AND DESIGN ANALYSIS Page 2 EXECUTIVE SUMMARY Executive Summary rail service. In some instances, the nearly significant challenge in locating a passen- Map 1: Locus Map The Housatonic Railroad Company (HRRC) century old historic passenger rail stations ger rail station in a downtown area was has proposed re-establishing passenger rail may meet these needs and in other instances, finding sites with sufficient room for park- service between Danbury, Connecticut and new locations may better serve them. ing. Thus, for the recommended down- Pittsfield, Massachusetts on the former town passenger rail stations a smaller To address this issue, the Berkshire Regional Berkshire Line. The passenger rail service amount of parking, compared to a regional Planning Commission (BRPC) partnered between these two locations last operated passenger rail station, will likely be availa- with HRRC to conduct this passenger rail in 1971 shortly after the Penn Central ble. -

RIVER KENNET Status: Site of Special Scientific Interest (SSSI)
COUNTY: BERKSHIRE/WILTSHIRE SITE NAME: RIVER KENNET Status: Site of Special Scientific Interest (SSSI) notified under Section 28 of the Wildlife and Countryside Act 1981 Local Planning Authorities: Berkshire County Council, Wiltshire County Council, Newbury District Council, Kennet District COuncil National Grid Reference: SU203692 to SU572667 Ordnance Survey Sheet 1:50,000: 174 1:10,000: SU26 NW, SU27 SW, SU27 SE, SU37 SW, SU36 NW, SU36 NE, SU47 NW, SU46 NE, SU56 NW, SU56 NE Date Notified (Under 1981 Act): 1 November 1995 Date of Last Revision: Area: 112.72 ha Other information: The River Lambourn, which is a tributary of the River Kennet, is also an SSSI. There are two existing SSSIs along the River Kennet: Freemans Marsh and Chilton Foliat Meadows. The site boundary is the bank top or, where this is indistinct, the first break of slope. Description and Reasons for Notification The River Kennet has a catchment dominated by chalk with the majority of the river bed being lined by gravels. The Kennet below Newbury traverses Tertiary sands and gravels, London Clay and silt, thus showing a downstream transition from the chalk to a lowland clay river. As well as having a long history of being managed as a chalk stream predominantly for trout, the Kennet has been further modified by the construction of the Kennet and Avon Canal. In some places the canal joins with the river to form a single channel. There are also many carriers and channels formerly associated with water meadow systems. The river flows through substantial undisturbed areas of marshy grassland, wet woodland and reed beds. -

Town & County Coverage Sheet
Town & County Coverage Sheet Massachusetts Counties Brian Forsythe, CWIC | Office Phone: (508) 856-2513 | Email: [email protected] Middlesex County: Acton; Ashby; Ayer; Bedford; Billerica; Boxborough; Burlington; Carlisle; Chelmsford; Concord; Dracut; Dunstable; Groton; Littleton; Lowell; Pepperell; Shirley; Tewksbury; Townsend; Tyngsborough; Westford; Wilmington Worcester County: Ashburnham; Athol; Barre; Berlin; Bolton; Clinton; Fitchburg; Gardner; Hardwick; Harvard; Hubbardston; Lancaster; Leominster; Lunenburg; New Braintree; Oakham; Petersham; Phillipston; Princeton; Royalston; Rutland; Sterling; Templeton; Westminster; Winchendon New York Counties: Albany, Columbia, Greene, Rensselaer, Schenectady, Schoharie, Washington Marjorie Longo, CWIC | Office Phone: (508) 856-8585 | Email: [email protected] Middlesex County: Arlington; Ashland; Belmont; Cambridge; Everett; Framingham; Holliston; Hopkinton; Hudson; Lexington; Lincoln; Malden; Marlborough; Maynard; Medford; Melrose; Natick; Newton; North Reading; Reading; Sherborn; Somerville; Stoneham; Stow; Sudbury; Wakefield; Waltham; Watertown; Wayland; Weston; Winchester; Woburn Worcester County: Auburn; Blackstone; Boylston; Brookfield; Charlton; Douglas; Dudley; East Brookfield; Grafton; Holden; Hopedale; Leicester; Mendon; Milford; Millbury; Millville; North Brookfield; Northborough; Northbridge; Oxford; Paxton; Shrewsbury; Spencer; Southborough; Southbridge; Sturbridge; Sutton; Upton; Uxbridge; Wales; Warren; Webster; West Boylston; West Brookfield; Westborough; -

Name County State Popula on Es Mate 2019 Bourne Town Barnstable
Name County State Popula/on es/mate 2019 Bourne town Barnstable County Massachuse3s 19762 Brewster town Barnstable County Massachuse3s 9775 Chatham town Barnstable County Massachuse3s 5982 Dennis town Barnstable County Massachuse3s 13871 Eastham town Barnstable County Massachuse3s 4906 Falmouth town Barnstable County Massachuse3s 30993 Harwich town Barnstable County Massachuse3s 12142 Mashpee town Barnstable County Massachuse3s 14229 Orleans town Barnstable County Massachuse3s 5788 Provincetown town Barnstable County Massachuse3s 2961 Sandwich town Barnstable County Massachuse3s 20169 Truro town Barnstable County Massachuse3s 2008 Wellfleet town Barnstable County Massachuse3s 2724 Adams town Berkshire County Massachuse3s 8010 Alford town Berkshire County Massachuse3s 488 Becket town Berkshire County Massachuse3s 1716 Cheshire town Berkshire County Massachuse3s 3129 Clarksburg town Berkshire County Massachuse3s 1638 Dalton town Berkshire County Massachuse3s 6525 Egremont town Berkshire County Massachuse3s 1205 Florida town Berkshire County Massachuse3s 715 Great Barrington town Berkshire County Massachuse3s 6945 Hancock town Berkshire County Massachuse3s 696 Hinsdale town Berkshire County Massachuse3s 1911 Lanesborough town Berkshire County Massachuse3s 2940 Lee town Berkshire County Massachuse3s 5664 Lenox town Berkshire County Massachuse3s 4944 Monterey town Berkshire County Massachuse3s 924 Mount Washington town Berkshire County Massachuse3s 157 New Ashford town Berkshire County Massachuse3s 223 New Marlborough town Berkshire County Massachuse3s -

Thames Valley and Surrey Care Records Partnership May 2020 TVS Care Records Partnership Update
Thames Valley and Surrey Care Records Partnership www.thamesvalleysurreycarerecords.net May 2020 TVS Care Records partnership update 1 URGENCY 2 WIDER ACCESS 3 ACCELERATION By the end of June During the COVID 19 pandemic Surrey, clinicians across up‐to‐date patient information Oxfordshire and Berkshire West, becomes even more important Milton Keynes Frimley and across Thames Valley and speeding up work Buckinghamshire Surrey. to get will have access information into to patient the platform as information across soon as possible. those areas. 4 AMBULANCES 5 FURTHER ACCELERATION 6 ACROSS BOUNDARIES We are looking where the Ambulance service SCAS and We are aiming to programme can be accelerated to subsequently SECAMB will share patient data help patients (for example, those access the care record. across ICS boundaries with cancer) ASAP. We will only accelerate if we can do it safely. 5/27/2020 4 TVS Care Records partnership update Given the COVID 19 pandemic the programme will require: • A more flexible approach, as staff may be deployed to support COVID‐19 related activities. • Each local area across Thames Valley & Surrey to take greater ownership of their TVS Care Records activity and our collective opportunities. LEADERSHIP We are delighted that Jane Hogg will be joining the programme as the new SRO for the TVS Partnership. Jane is currently the Integration and Transformation Director for Frimley Integrated Care System (ICS) and will be leading the work of the partnership alongside her Frimley ICS role. 5/27/2020 5 Who?: the Thames -

West Berkshire
West Berkshire Census 2001 and Access to Services Focus on Rural Areas West Berkshire is in the South East Government Office Region 1 Map of the Government Office Region showing Authority boundaries and shaded by Output Area according to the urban / rural definition. - 2 - Population In West Berkshire 42.8% of people live in rural areas, compared with 22.4% in the Government Office Region. Within the rural areas all people live in less sparse areas West Berkshire South East Male Female Total Male Female Total Urban 40,992 41,598 82,590 3,025,510 3,180,658 6,206,168 Rural 30,711 31,182 61,893 879,645 914,832 1,794,477 Less Sparse 30,711 31,182 61,893 878,911 914,059 1,792,970 Town 11,629 12,022 23,651 373,428 398,650 772,078 Village 12,858 12,914 25,772 338,028 346,602 684,630 Dispersed 6,224 6,246 12,470 167,455 168,807 336,262 Sparse - - - 734 773 1,507 Town - - - 137 146 283 Village - - - 597 627 1,224 Dispersed - - - - - - Total 71,703 72,780 144,483 3,905,155 4,095,490 8,000,645 Percentage rural 42.8 42.8 42.8 22.5 22.3 22.4 Source table from the Census: UV03 Gender Proportion of the population of the Authority living in rural towns, villages and dispersed areas compared with the Government Office Region and England. West Berkshire South East England Dispersed Village Rural type Town 0 1020304050 Percentage Source table from the Census: UV03 Gender 3 Age In West Berkshire 5.1% of the population live in rural areas and are under 10 years old. -

Berkshire | Buckinghamshire | Hampshire | Isle of Wight | London | Oxfordshire
News and events for autumn/winter 2019 Berkshire | Buckinghamshire | Hampshire | Isle of Wight | London | Oxfordshire Christmas at Chastleton OXFORDSHIRE Sat 23 – Sun 24, Sat 30 Nov, Sun 1 & Sat 7 – Sun 8 Dec 11am-3pm The Buscot and Coleshill Come and see the house magically Estates transformed for a Victorian Christmas. Near Faringdon. SN6 7PT Tel: 01793 762209 Greys Court Near Henley-on-Thames. RG9 4PG Coleshill Underground WWII event Tel: 01491 628529 Sun 22 Sep 10am-4pm Discover Coleshill’s hidden Second World War Heritage Open Days: Harvest at Greys Court history. Talks, trails, re-enactors, access to Wed 18 & Thu 19 Sep our replica bunker at the home of Churchill’s Ten-minute talks by expert gardeners, fruit British Resistance. tasting and more, with free entry for all for Adults £5 Child £2.50 Heritage Open Days. B 0344 249 1895 or online October half-term: Loads of leaves Coleshill open afternoons Sat 26 Oct - Sun 3 Nov Sun 13 Oct 2-5pm Pick up a trail leaflet and wander the estate in See our restored water mill to find out how search of clues celebrating the autumn colour. flour is produced and explore a Second World £2 War replica bunker. Christmas at Basildon Park Christmas: Gift of giving Introduction to coppicing workshop Sat 23 Nov – Mon 6 Jan Sat 26 Oct & Sat 16 Nov 9am-4pm Celebrate the anniversary of the gift of Greys Court to the nation. It’s set to be really festive. Victorian Decadence: Practical day with our expert ranger in our BERKSHIRE Christmas at Basildon Park woods to learn about the history of coppicing, tool selection and safe use, cutting stools and Christmas dinners in the cowshed Sat 23 Nov – Mon Jan 7 Weekdays in Dec 12noon & 1.30pm Basildon Park Witness Basildon Park dripping in opulent basic processing of wood for products and wildlife benefits. -

Improving Health and Care in Buckinghamshire, Oxfordshire and Berkshire West
Improving health and care in Buckinghamshire, Oxfordshire and Berkshire West Who we are, how we work together and our developing priorities and plans for the next five years Contents 0 Introduction 1 Introduction Our vision About us Welcome to the first of a number of public updates about the development of a five year strategy for the Buckinghamshire, Oxfordshire and Berkshire West Integrated Care System (BOB ICS). Our aim in this update is to provide you with information on: Page 1 Page 5 Page 6 How we work together as a Buckinghamshire, Oxfordshire and Berkshire West Integrated Care System (BOB ICS) Positives Challenges How we work together Our vision and aims Our thoughts about priorities Page 8 Page 9 Page 11 Our work to develop a five year plan by the end of November 2019 How services are Healthy places to live, Our priorities planned for and great places to work - delivered our people strategy The BOB ICS five year, one system plan will set out how all ICS partners will work together locally and together at scale to meet the current and future health and care needs of the communities we serve. It will describe how the BOB ICS will deliver the requirements of NHS Long Term Plan (www.longtermplan.nhs.uk) and address BOB ICS’s specific priorities. We are fully committed to being open and transparent about how the plan is developing over the Page 13 Page 14 Page 15 coming months - this document is the first step in that process. It will be followed by the publication of our draft “technical” submission to NHS England / NHS Improvement in early October and a final version of this technical document, once reviewed and signed off later in the year. -
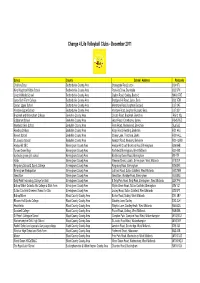
Website List Dec 11
Change 4 Life Volleyball Clubs - December 2011 School County School Address Postcode Challney Boys Bedfordshire County Area Stoneygate Road, Luton LU4 9TJ King Houghton Middle School Bedfordshire County Area Parkside Drive, Dunstable LU5 5PX Lincroft Middle School Bedfordshire County Area Station Road, Oakley, Bedford MK43 7RE Luton Sixth Form College Bedfordshire County Area Bradgers Hill Road, Luton, Beds LU2 7EW Cedars Upper School Bedfordshire County Area Mentmore Road, Leighton Buzzard LU7 2AE Vandyke Upper School Bedfordshire County Area Vandyke Road, Leighton Buzzard, Beds LU7 3DY Bracknell and Wokingham College Berkshire County Area Chruch Road, Bracknell, Berkshire RG12 1DJ Edgbarrow School Berkshire County Area Grant Road, Crowthorne, Surrey RG45 7HZ Newlands Girls School Berkshire County Area Farm Road, Maidenhead, Berkshire SL6 5JB Reading College Berkshire County Area Kings Road, Reading, Berkshire RG1 4HJ Kennet School Berkshire County Area Stoney Lane, Thatcham, Berks RG19 4LL St Josephs School Berkshire County Area Newport Road, Newbury, Berkshire RG14 2AW Hodge Hill SEC Birmingham County Area Hodge Hill Court, Bromford Road, Birmingham B36 8HB Turves Green Boys Birmingham County Area Northfield, Birmingham, West Midlands B31 4BS bordesley green girls school Birmingham County Area Bordesley Green Road, Birmingham B9 4TR Holte Birmingham County Area Wheeler Street, Lozells, Birmingham, West Midlands B19 2EP Kingsbury School & Sports College Birmingham County Area Kingsbury Road, Birmingham B24 8RE Birmingham Metropolitan