What's Going on Down There?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prioritization of Health Services
PRIORITIZATION OF HEALTH SERVICES A Report to the Governor and the 74th Oregon Legislative Assembly Oregon Health Services Commission Office for Oregon Health Policy and Research Department of Administrative Services 2007 TABLE OF CONTENTS List of Figures . iii Health Services Commission and Staff . .v Acknowledgments . .vii Executive Summary . ix CHAPTER ONE: A HISTORY OF HEALTH SERVICES PRIORITIZATION UNDER THE OREGON HEALTH PLAN Enabling Legislatiion . 3 Early Prioritization Efforts . 3 Gaining Waiver Approval . 5 Impact . 6 CHAPTER TWO: PRIORITIZATION OF HEALTH SERVICES FOR 2008-09 Charge to the Health Services Commission . .. 25 Biennial Review of the Prioritized List . 26 A New Prioritization Methodology . 26 Public Input . 36 Next Steps . 36 Interim Modifications to the Prioritized List . 37 Technical Changes . 38 Advancements in Medical Technology . .42 CHAPTER THREE: CLARIFICATIONS TO THE PRIORITIZED LIST OF HEALTH SERVICES Practice Guidelines . 47 Age-Related Macular Degeneration (AMD) . 47 Chronic Anal Fissure . 48 Comfort Care . 48 Complicated Hernias . 49 Diagnostic Services Not Appearing on the Prioritized List . 49 Non-Prenatal Genetic Testing . 49 Tuberculosis Blood Test . 51 Early Childhood Mental Health . 52 Adjustment Reactions In Early Childhood . 52 Attention Deficit and Hyperactivity Disorders in Early Childhood . 53 Disruptive Behavior Disorders In Early Childhood . 54 Mental Health Problems In Early Childhood Related To Neglect Or Abuse . 54 Mood Disorders in Early Childhood . 55 Erythropoietin . 55 Mastocytosis . 56 Obesity . 56 Bariatric Surgery . 56 Non-Surgical Management of Obesity . 58 PET Scans . 58 Prenatal Screening for Down Syndrome . 59 Prophylactic Breast Removal . 59 Psoriasis . 59 Reabilitative Therapies . 60 i TABLE OF CONTENTS (Cont’d) CHAPTER THREE: CLARIFICATIONS TO THE PRIORITIZED LIST OF HEALTH SERVICES (CONT’D) Practice Guidelines (Cont’d) Sinus Surgery . -

Pruritus Vulvae
628 BRITISH MEDICAL JOURNAL 17 MARCH 1973 may wronglly lead to the diagnosis of primary hyperaldo- 13 Mitchell, J. D., Baxter, T. J., Blair-West, J. R., and McCredie, D. A., Archives of Disease in Childhood, 1970, 45, 376. steronism and even to the excision of the wrong endocrine 14 Voute, P. A., Meer, J. van der, and Staugaard-Kloosterziel, W., Acta Endocrinologica, 1971, 67, 197. Br Med J: first published as 10.1136/bmj.1.5854.628 on 17 March 1973. Downloaded from gland. 15 Hudson, J. B., Chobanian, A. V., and Relman, A. S., New England The opposite clinical syndrome-primary lack of renin or J'ournal of Medicine, 1957, 257, 529. 16 Jacobs, D. R., and Posner, J. B., Metabolism, 1964, 13, 522. hyporeninism-has also been recognized recently. In this 17 Vagnucci, A. H., Journal of Clinical Endocrinology and Metabolism, 1969, disease primary lack of renin (and hence of its active pro- 29, 279. 18 Perez, G., Siegel, L., and Schreiner, G. E., Annals of Internal Medicine, duct angiotension II) apparently leads to selective deficiency 1972, 76, 757. of aldosterone associated with normal cortisol production. 19 Ferrara, E., Werk, E., Hanenson, I., Privirera, P., and Kenyon, C., Clinical Research, 1970, 18, 602. The literature contains reference to some 20 cases of isolated 20 Schambelan, M., Stockigt, J. R., and Biglieri, E. G., New England J ournal of Medicine, 1972, 287, 573. analdosteronism, the first a report by J. B. Hudson and his 21 Weidman, P., et Clinical Research, 1972, 20, 249. colleagues15 in 1957. Only recently however has the primary al., deficiency been recognized as renin lack in at least some of these patients. -

Some Aspects of Œstrogenic Therapy
Edinburgh Medical Journal February 1942 SOME ASPECTS OF (ESTROGENIC THERAPY * By W. F. T. HAULTAIN, O.B.E., M.C., B.A., M.B., F.R.C.S.Ed., F.R.C.O.G. I HAVE chosen the subject of cestrogenic therapy for this lectui e for several reasons. The first is that the discovery of the female sex hormones is of comparatively recent origin and, though no doubt there is still much to be discovered with regard to sexual physiology, the work on the natural and synthetic oestrogens has advanced rapidly, with the result that various preparations are even now of the greatest use to the clinician. Secondly, cestrogenic therapy has always been of particular interest to me, even long before I had heard of such a name, and in 1928 I 1 wrote a paper on the administration of ovarian extract for the artificial menopause, gleaned from work which I had been carrying out clinically for five years previously. Since that time I have continued my clinical observations with the various natural and synthetic oestrogenic products which have been introduced, and in this lecture I intend to include my further observations in their appropriate place. Thirdly, special work in the clinical use of has oestrogens been carried out during the last three years in my obstetrical and gynaecological wards. That being so, I intend to deal chiefly in this lecture with conditions with which I have had some clinical experience in regard to the value of oestrogens, and will do no more than refer to other conditions for which have oestrogens been recommended, of which I have no personal experience. -

Is There Any Reason of Irritating Vulvar Itching?
Mini Review ISSN: 2574 -1241 DOI: 10.26717/BJSTR.2021.33.005347 Is there Any Reason of Irritating Vulvar Itching? Magdalena Bizoń Szpernalowska* and Włodzimierz Sawicki Chair and Department of Obstetrics, Medical University of Warsaw, Poland *Corresponding author: Magdalena Bizoń Szpernalowska, Chair and Department of Obstetrics, Gynecology and Gynecological Oncology, ul. Kondratowicza 8, 03-242 Warsaw, Poland ARTICLE INFO ABSTRACT Received: Published: December 27, 2020 Vulvar complains like itching, burning and pain are reported mainly by women in peri- and postmenopuasal age. Severity of symptoms influence on well-being. The most January 11, 2021 frequent reason of vulvar symptoms is lichen sclerosus. Diagnose is given after vulvar Citation: biopsy, which is crucial in exact diagnosis. Sometimes histological result can also reveal hypertrophy of epithelium, acanthosis, lichen planus, vulvar intraepithalial neoplasia or Magdalena Bizoń S, Włodzimierz even vulvar cancer. Lichen sclerosus cause leucoplacia, vulvar atrophy and narrowing of S. Is there Any Reason of Irritating Vulvar the vagina. Delay of diagnosis cause quicker progression of disease and intensification Itching?. Biomed J Sci & Tech Res 33(1)- of vulvar symptoms. The first line of treatment is based on ointments according to 2021.Abbreviations: BJSTR. MS.ID.005347. glicocorticosteroids. If there is no response on this method, the alternative way is photodynamic therapy (PDT). The aim of the treatment is to protect against progression LS: Lichen Sclerosus; PDT: ofKeywords: lichen sclerosus and decrease vulvar symptoms. Photodynamic Therapy; VIN: Vulvar In- traepithelial Neoplasia lichen sclerosus; itching; photodynamic therapy Mini Review weissflechen dermatose and white spot disease [5]. Nomenclature Clinical vulvar symptoms like itching, burning and pain are include also term of lichen sclerosus and atrophicus [6]. -

Vulvar Lichen Sclerosus Et Atrophicus Pragya Ashok Nair
[Downloaded free from http://www.jmidlifehealth.org on Friday, June 16, 2017, IP: 201.13.5.108] Review Article Vulvar Lichen Sclerosus et Atrophicus Pragya Ashok Nair Department of Dermatology Vulvar lichen sclerosus (VLS) is a chronic inflammatory dermatosis characterized and Venereology, by ivory‑white plaques or patches with glistening surface commonly affecting the Pramukshwami Medical College, Karamsad, Gujarat, vulva and anus. Common symptoms are irritation, soreness, dyspareunia, dysuria, and India urinary or fecal incontinence. Anogenital lichen sclerosus (LS) is characterized by Abstract porcelain‑white atrophic plaques, which may become confluent extending around the vulval and perianal skin in a figure of eight configuration. Thinning and shrinkage of the genital area make coitus, urination, and defecation painful. LS is not uncommon in India and present as an itchy vulvar dermatosis which a gynecologist may mistake for candidal vulvovaginitis. There is often a delay in diagnosis of VLS due to its asymptomatic nature and lack of awareness in patients as well as physicians. Embarrassment of patients due to private nature of the disease and failure to examine the genital skin properly are the other reasons for delay in diagnosis. There is no curative treatment for LS. Various medications available only relieve the symptoms. Chronic nature of the disease affects the quality of life. Proper and regular follow‑up is required as there are chances of the development of squamous cell carcinoma. Keywords: Dermatosis, lichen sclerosus et atrophicus, vulva Introduction old.[3] Women are more commonly affected than men ulva is the most visible female genital structure, with 10:1 ratio, particularly during menopausal age V but it has received the least attention in the medical group, but younger women or girls may also be affected. -

What's Going on Down There?
What’s Going on Down There? Denise Rizzolo, PhD, PA-C Introduction • Vulvovaginitis is inflammation of the vulva and vaginal tissues. • Characterized by vaginal discharge and/or vulvar itching and irritation as well as possible vaginal odor. • Accounts for 10 million visits yearly in the US and is the most common gynecologic complaint in prepubertal girls. History- What should you ask? • Pruritus -General or just one spot • Soreness: stinging / burning / pain • Difficulty with sex • Lumps • Discharge • Partner’s have any symptoms • History of similar symptoms Physical Examination • Careful gynecologic exam • Inspection of discharge • Close examination of vulvovaginal area • Careful inspection of cervix • Look at perineum as well Physiologic Discharge • Responsible for 10 percent of cases of vaginal discharge. • Composed of vaginal squamous cells suspended in fluid medium. • Clinical characteristics: • clear to slightly cloudy • non-homogeneous • highly viscous • Changes throughout the month Normal Vaginal Discharge • Not associated with: • itching • burning • malodor • Normal increase in volume • ovulation • following coitus • after menses • during pregnancy The Big 3 •Three most common causes of vulvovaginitis include: • Bacterial Vaginosis • Vaginal candidiasis • Trichomonas Vaginalis •Others include: atrophic vaginitis, irritant vaginitis, and other STIs. Vaginal Candidiasis- Overview • Less common in postmenopausal women, unless taking estrogen. • 90% of yeast infections are secondary to Candida Albican (Most common). • Risk Factors -

The Use of the Hormones in Dermatology'
THE USE OF THE HORMONES IN DERMATOLOGY' MILTON M. IIAIITMAN, M.D., F.A.C.A. San Francisco, California T he endocrine glands exert far reaching effects that we are only now beginning to understand. Aside from the direct specific effects of the various endo- crinopathies on the skin, there may be effects mediated through the autonomic nervous system. Endocrine dysfunction may affect the emotional state and aggravate or initiate psycho-somatic disorders. Allergic disturbances, in eluding those of the skin, comprise an important group of ailments. That specific sensitivities arc not the complete answer to the etiology of allergic disorders, and that the approach by many of them is not the invariable answer to their treatment has long been known. Why a given allergen can at one time provoke a clinical manifestation of allergy and at other times not, is determined by factors which modify the allergic status. Endocrine dysfunctions are among the important factors modifying this status. It is obvious that some knowledge of endocrinology is a necessity to the dermatologist wishing to arm himself \vith the maximum in effective therapeutic weapons. A summary of the clinical and experimental uses of hormones in dermatology is herein presented under three logical headings: A. 5KIN DISORDERS DUE TO THR DEFIC1RNCY OR ABSENCR OF A SPRCIFIC ENDOCRINE PRODUCT RRSPONDING TO SUBSTITUTIVE THERAPY rihe following phenomena should be matters of common knowledge: 1) The brownish pigmentation of adreno-cortieal deficiency (Addison's disease) being arrested and even reversed by adrenal cortex extracts and the synthetic desoxy- corticosterone acetate. 2) The myxedema of hypothyroidism being fully cor- rected by dessicated thyroid or thyroxin. -

A Clinico-Pathological Study of Vulval Dermatoses
J Clin Pathol: first published as 10.1136/jcp.28.5.394 on 1 May 1975. Downloaded from J. clin. Path., 1975, 28, 394-402 A clinico-pathological study of vulval dermatoses P. C. LEIGHTON AND F. A. LANGLEY From the Departments ofObstetrics and Gynaecology and ofPathology, University ofManchester SYNOPSIS A long-term review of 108 women suffering from various forms of vulval dermatosis is described and a detailed analysis of those with chronic hypertrophic vulvitis, lichen sclerosus et atrophicus, and neurodermatitis is made. One case of neurodermatitis and two cases of lichen sclerosus progressed to carcinoma but no case of chronic hypertrophic vulvitis became malignant. It is possible that vulval dermatoses occur more commonly in the nulliparous than in the parous women and there is a slight preponderance of women who are blood group A. It is suggested that the term 'leukoplakia' should be abandoned and that vulval lesions should be described in precise and meaningful histological terms. Although the vulva may be regarded as part of the vulva were recorded in the laboratory diagnostic genital tract it is also part of one of the largest file in the 19 years, 1949 to 1968, but after 1968 organs of the body, namely, the skin. For this reason very few cases of leukoplakia were recorded because most of its disorders are those of the skin modified of uncertainty about the diagnostic criteria and only by site. However, when well defined derma- these have not been investigated further. All the tological conditions such as psoriasis and candida available histological material from the 108 cases infections are excluded, a residue ofill-defined derma- was reviewed. -
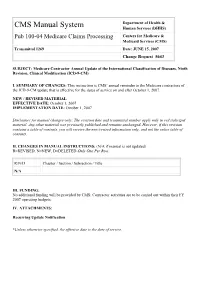
Transmittal 1269 Date: JUNE 15, 2007 Change Request 5643
Department of Health & CMS Manual System Human Services (DHHS) Pub 100-04 Medicare Claims Processing Centers for Medicare & Medicaid Services (CMS) Transmittal 1269 Date: JUNE 15, 2007 Change Request 5643 SUBJECT: Medicare Contractor Annual Update of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) I. SUMMARY OF CHANGES: This instruction is CMS’ annual reminder to the Medicare contractors of the ICD-9-CM update that is effective for the dates of service on and after October 1, 2007. NEW / REVISED MATERIAL EFFECTIVE DATE: October 1, 2007 IMPLEMENTATION DATE: October 1, 2007 Disclaimer for manual changes only: The revision date and transmittal number apply only to red italicized material. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents. II. CHANGES IN MANUAL INSTRUCTIONS: (N/A if manual is not updated) R=REVISED, N=NEW, D=DELETED-Only One Per Row. R/N/D Chapter / Section / Subsection / Title N/A III. FUNDING: No additional funding will be provided by CMS; Contractor activities are to be carried out within their FY 2007 operating budgets. IV. ATTACHMENTS: Recurring Update Notification *Unless otherwise specified, the effective date is the date of service. Attachment – Recurring Update Notification Pub. 100-04 Transmittal: 1269 Date: June 15, 2007 Change Request: 5643 SUBJECT: Medicare Contractor Annual Update of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) Effective Date: October 1, 2007 Implementation Date: October 1, 2007 I. -

Effects Different in Women
8 Gynecology O B .GYN. NEWS • April 1, 2005 ultimate genetic effect,” he continued. risk ofcoronary heart disease in the en- Effects Different in Women, Men For example, in 2002, American suing 10 years, 12% had a 5%-9.9% risk, Aspirin from page 1 women had 373,000 new strokes and and 4% had a risk that was 10% or 345,000 new MIs, said Dr. Buring, a pro- greater for developing coronary heart lighted intrinsic differences in the way “The results show the danger ofgener-fessor of epidemiology at Harvard School disease during the 10 years after they en- that CVD plays out in women, compared alization,” said Paul M. Ridker, M.D., di- ofPublic Health, Boston. In contrast,tered the study. The women were ran- with men. In this study ofwomen,rector ofthe Center for Cardiovascular men had 520,000 new MIs and 323,000 domized to the aspirin regimen or place- strokes were more common than MIs, Disease Prevention at Brigham and new strokes. bo, which they continued during an and aspirin’s benefit was largely in stroke Women’s Hospital in Boston and co–prin- The study enrolled 39,876 healthy, fe- average follow-up of 10.1 years. During prevention. In contrast, results from pri- cipal investigator for the study along with male health professionals during the ear- follow-up, 999 participants had a first, or studies in healthy men, including the Dr. Buring. ly 1990s who reported their baseline major cardiovascular event: nonfatal MI, very similarly designed Physicians’ “The finding that women behave dif- health data by returning a questionnaire. -

Studies in Human Sterility with Special Reference To
STUDIES IN HUMAN STERILITY WITH SPECIAL REFERENCE TO THE INVEST IGAT ION OP THE PATENCY AND FUNCTION OP THE FALLOPIAN TUBES AND OP THE CONDITION OP THE ENLOMETRIUM. ProQuest Number: 13849840 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a com plete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest ProQuest 13849840 Published by ProQuest LLC(2019). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States C ode Microform Edition © ProQuest LLC. ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106- 1346 PREFACE. The thesis which is presented here, consists of two parts &nd an appendix. Part I concerns the pathogenesis, diagnosis and treatment of Human Sterility and is an endeavour to give a comprehensive account of this subject, incorporating a study of much new knowledge and of recent advances which mainly concern technical refinements in the investigation of tubal patency and function, the endometrial cycle and the tfsex hormones.” Only slight reference is made to the male aspect of the problem. In effect, this part of the thesis is almost entirely my contribution to the book ”Sterility and Impaired Fertility” (1959), Hamish Hamilton Medical Books, London, (jointly with C. Lane-Roberts, K. Walker and B.P. Wiesner). The few pages which are included here and which were not written by me are indicated in the text. -

A Clinical Study of Non Venereal Genital Dermatoses
A CLINICAL STUDY OF NON VENEREAL GENITAL DERMATOSES Dissertation submitted to THE TAMILNADU DR. M.G.R. MEDICAL UNIVERSITY CHENNAI – 600 032 APRIL - 2015. In partial fulfillment of the regulations required for the award of M.D. DEGREE IN DERMATOLOGY, VENEREOLOGY AND LEPROLOGY BRANCH XII DEPARTMENT OF DERMATOLOGY Coimbatore Medical College Hospital, Coimbatore. DECLARATION I Dr.A.N.M.Maalik babu solemnly declare that the dissertation entitled “A clinical study of non venereal genital dermatoses” was done by me in the Department of Dermatology and Venereology at Coimbatore Medical College Hospital during the period from August 2013 to July 2014 under the guidance & supervision of Dr.P.P.Ramasamy M.D.,D.D., Professor & Head of Department, Department of Dermatology and Venereology ,Coimbatore Medical College Hospital ,Coimbatore. The dissertation is submitted to Tamil nadu Dr.MGR Medical University,Chennai towards the partial fulfillment of the requirement for the award of M.D., degree in Dermatology, Venereology and Leprology. I have not submitted this dissertion on any previous occasion to any university for the award of any degree. PLACE: Dr. A.N.M.Maalik babu DATE: CERTIFICATE This is to certify that the dissertation entitled “A clinical study of non venereal genital dermatoses ” is a record of bonafide work done by Dr.A.N.M.Maalik babu , Post graduate student in the Department of Dermatology , Venereology and Leprology , Coimbatore Medical College Hospital,Coimbatore under the guidance of Dr.P.P.Ramasamy M.D.,D.D., Professor & Head of Department, Department of Dermatology, Coimbatore Medical College Hospital ,Coimbatore in partial fulfillment of the regulations of the Tamilnadu DR.M.G.R Medical University, Chennai towards the award of M.D., degree (Branch XII) in Dermatology, Venereology and Leprology.