Cutaneous Adverse Reaction to Infliximab: Report of Psoriasis Developing in 3 Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Paraneoplastic Syndrome Presenting As Giant Porokeratosis in a Patient with Nasopharyngeal Cancer
Paraneoplastic Syndrome Presenting As Giant Porokeratosis in A Patient with Nasopharyngeal Cancer Fitri Azizah, Sonia Hanifati, Sri Adi Sularsito, Lili Legiawati, Shannaz Nadia Yusharyahya, Rahadi Rihatmadja Department of Dermatology and Venereology, Faculty of Medicine Universitas Indonesia / Dr. Cipto Mangunkusumo National General Hospital Keywords: porokeratosis, giant porokeratosis, paraneoplastic syndrome, nasopharyngeal Abstract: Giant porokeratosis is a rare condition in which the hyperkeratotic plaques of porokeratosis reach up to 20 cm in diameter. Porokeratosis is characterized clinically by hyperkeratotic papules or plaques with a thread-like elevated border. Although rare, porokeratosis has been reported in conjunction with malignancies suggesting a paraneoplastic nature. Associated malignancies reported were hematopoietic, hepatocellular, and cholangiocarcinoma. We report a case of giant porokeratosis in a patient with nasopharyngeal cancer responding to removal of the primary cancer by chemoradiotherapy. 1 INTRODUCTION regress completely after the treatment of malignancy, suggestive of paraneoplastic syndrome. Porokeratosis is a chronic progressive disorder of keratinization, characterized by hyperkeratotic papules or plaques surrounded by a thread-like 2 CASE elevated border corresponds to a typical histologic hallmark, the cornoid lamella . O regan, 2012) There Mr. SS, 68-year-old, was referred for evaluation of are at least six clinical variants of porokeratosis pruritic, slightly erythematous plaques with raised, recognized with known genetic disorder.1 Some hyperpigmented border of one and a half year clinical variant of porokeratosis has been reported in duration on the extensor surface of both legs. The the setting of immunosuppressive conditions, organ lesions shown minimal response to potent topical transplantation, use of systemic corticosteroids, and corticosteroids and phototherapy given during the infections, suggesting that impaired immunity may last 8 months in another hospital. -

Features of Reactive White Lesions of the Oral Mucosa
Head and Neck Pathology (2019) 13:16–24 https://doi.org/10.1007/s12105-018-0986-3 SPECIAL ISSUE: COLORS AND TEXTURES, A REVIEW OF ORAL MUCOSAL ENTITIES Frictional Keratosis, Contact Keratosis and Smokeless Tobacco Keratosis: Features of Reactive White Lesions of the Oral Mucosa Susan Müller1 Received: 21 September 2018 / Accepted: 2 November 2018 / Published online: 22 January 2019 © Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract White lesions of the oral cavity are quite common and can have a variety of etiologies, both benign and malignant. Although the vast majority of publications focus on leukoplakia and other potentially malignant lesions, most oral lesions that appear white are benign. This review will focus exclusively on reactive white oral lesions. Included in the discussion are frictional keratoses, irritant contact stomatitis, and smokeless tobacco keratoses. Leukoedema and hereditary genodermatoses that may enter in the clinical differential diagnoses of frictional keratoses including white sponge nevus and hereditary benign intraepithelial dyskeratosis will be reviewed. Many products can result in contact stomatitis. Dentrifice-related stomatitis, contact reactions to amalgam and cinnamon can cause keratotic lesions. Each of these lesions have microscopic findings that can assist in patient management. Keywords Leukoplakia · Frictional keratosis · Smokeless tobacco keratosis · Stomatitis · Leukoedema · Cinnamon Introduction white lesions including infective and non-infective causes will be discussed -

Review Skin Changes Are One of the Earliest Signs of Venous a R T I C L E Hypertension
pp 11 - 19 ABSTRACT Review Skin changes are one of the earliest signs of venous A R T I C L E hypertension. Some of these changes such as venous eczema are common and easily identified whereas DERMATOLOGICAL other changes such as acroangiodermatitis are less common and more difficult to diagnose. Other vein MANIFESTATIONS OF VENOUS related and vascular disorders can also present with specific skin signs. Correct identification of these DISEASE: PART I skin changes can aid in making the right diagnosis and an appropriate plan of management. Given KUROSH PARSI, MBBS, MSc(Med), FACD, FACP the significant overlap between phlebology and Departments of Dermatology, St. Vincent’s Hospital and dermatology, it is essential for phlebologists to be Sydney Children’s Hospital familiar with skin manifestations of venous disease. Sydney Skin & Vein Clinic, This paper is the first installment in a series of 3 Bondi Junction, NSW, Australia and discusses the dermatological manifestations of venous insufficiency as well as other forms of vascular ectasias that may present in a similar Introduction fashion to venous incompetence. atients with venous disease often exhibit dermatological Pchanges. Sometimes these skin changes are the only clue to an appropriate list of differential diagnoses. Venous ulceration. Less common manifestations include pigmented insufficiency is the most common venous disease which purpuric dermatoses, and acroangiodermatitis. Superficial presents with a range of skin changes. Most people are thrombophlebitis (STP) can also occur in association with familiar with venous eczema, lipodermatosclerosis and venous incompetence but will be discussed in the second venous ulcers as manifestations of long-term venous instalment of this paper (Figure 2). -

Progressive Widespread Warty Skin Growths
DERMATOPATHOLOGY DIAGNOSIS Progressive Widespread Warty Skin Growths Patrick M. Kupiec, BS; Eric W. Hossler, MD Eligible for 1 MOC SA Credit From the ABD This Dermatopathology Diagnosis article in our print edition is eligible for 1 self-assessment credit for Maintenance of Certification from the American Board of Dermatology (ABD). After completing this activity, diplomates can visit the ABD website (http://www.abderm.org) to self-report the credits under the activity title “Cutis Dermatopathology Diagnosis.” You may report the credit after each activity is completed or after accumu- lating multiple credits. A 33-year-old man presented with progres- sive widespread warty skin growths that had been present copysince 6 years of age. Physical examination revealed numerous verrucous papules on the face and neck along with Figure 1. H&E, original magnification ×40. Figure 2. H&E, original magnification ×40. verrucous, tan-pink papules and plaques diffuselynot scattered on the trunk, arms, and legs. A biopsy of a lesion on the neck Dowas performed. H&E, original magnification ×200. The best diagnosisCUTIS is: a. condyloma acuminatum b. epidermodysplasia verruciformis c. herpesvirus infection d. molluscum contagiosum e. verruca vulgaris PLEASE TURN TO PAGE 99 FOR DERMATOPATHOLOGY DIAGNOSIS DISCUSSION Mr. Kupiec is from the State University of New York (SUNY) Upstate Medical University, Syracuse. Dr. Hossler is from the Departments of Dermatology and Pathology, Geisinger Medical Center, Danville, Pennsylvania. The authors report no conflict of interest. Correspondence: Patrick M. Kupiec, BS, 50 Presidential Plaza, Syracuse, NY 13202 ([email protected]). 82 CUTIS® WWW.CUTIS.COM Copyright Cutis 2017. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. -

Vulvar Disease: Overview of Diagnosis and Management for College Aged Women
Vulvar Disease: Overview of Diagnosis and Management for College Aged Women Lynette J. Margesson MD FRCPC ACHA 2013 Annual Meeting, May 30, 2013 No Conflicts of interest Lynette Margesson MD Little evidence based treatment Most information is from small open trials and clinical experience. Most treatment discussed is “off-label” Why Do Vulvar Disease ? Not taught Not a priority Takes Time Still an area if taboo VULVAR CARE IS COMMONLY UNAVAILABLE For women this is devastating Results of Poor Vulvar Care Women : - suffer with undiagnosed symptoms - waste millions of dollars on anti-yeasts - hide and scratch - endure vulvar pain and dyspareunia - are desperate for help VULVA ! What is that? Down there? Vulvar Education Lets eliminate the “Down there” generation Use diagrams and handouts See www.issvd.org - patient education Recognize Normal Anatomy Normal vulvar anatomy Age Race Hormones determine structure - Size & shape - Pigmentation -Hair growth History A good,detailed,accurate history All previous treatment Response to treatment All medications, prescribed and over-the-counter TAKE TIME TO LISTEN Genital History in Women Limited by: embarrassment lack of knowledge social taboos Examination Tips Proper visualization - light + magnification Proper lighting – bright, but no glare Erythema can be normal Examine rest of skin, e.g. mouth, scalp and nails Many vulvar diseases scar, not just lichen sclerosus Special Anatomic Variations Sebaceous hyperplasia ectopic sebaceous glands Vulvar papillomatosis Pre-anesthesia – BIOPSY use a topical -

Brown Papules and a Plaque on the Calf
PHOTO CHALLENGE CLOSE ENCOUNTERS WITH THE ENVIRONMENT Brown Papules and a Plaque on the Calf Jin A. Kim, MD; Ji Hyun Lee, MD, PhD; Jun Young Lee, MD, PhD; Young Min Park, MD, PhD copy not Do A 61-year-old man presented with a cluster of asymptomatic brown papules and a plaque on the left calf of several years’ duration. The lesion consisted of multiple, dark brown, hyperkeratotic papules on a well-demarcated light brown flat plaque. The patient reported no increase in the size or number of lesions. He did not have a history of trauma or a per- sonal or family history of skin cancer. CUTIS What’s the diagnosis? a. agminated lentiginosis b. irritated seborrheic keratosis c. lentigo maligna melanoma d. speckled lentiginous nevus e. verruca plana From the Department of Dermatology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul. The authors report no conflict of interest. Correspondence: Young Min Park, MD, PhD, Department of Dermatology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, 222 Banpo-daero, Seocho-Gu, Seoul, South Korea ([email protected]). WWW.CUTIS.COM VOLUME 97, JUNE 2016 E17 Copyright Cutis 2016. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. Photo Challenge Discussion The Diagnosis: Irritated Seborrheic Keratosis iopsies of one of the protruding papules and the The histology of SK shows monotonous basaloid underlying plaque were performed. The speci- tumor cells without atypia. It generally is com- Bmen from the papule showed hyperkeratosis, prised of focal acanthosis and papillomatosis with acanthosis, papillomatosis, and a flattened dermoepi- a sharp flat base. -

Incidental Focal Acantholytic Dyskeratosis in the Setting of Rosacea
Letter to the Editor http://dx.doi.org/10.5021/ad.2013.25.4.518 Incidental Focal Acantholytic Dyskeratosis in the Setting of Rosacea Sang-Yeon Park, Hae Jin Lee, Jae Yong Shin, Sung Ku Ahn Department of Dermatology, Yonsei University Wonju College of Medicine, Wonju, Korea Dear Editor: direct immunofluorescence (Fig. 2). In the serial sections, Focal acantholytic dyskeratosis (FAD) was first described we observe the same findings. Differential diagnosis for by Ackerman1 in 1972 as a distinct histopathological pat- the possibility of polymorphous light eruption, systemic tern associated with various cutaneous conditions, and lupus erythematosus, contact dermatitis, and dermatitis with classic histopathological findings including supra- artefacta should be considered. But given these clinical basal clefting, hyperkeratosis and parakeratosis, and the and histopathological features, a diagnosis of rosacea with presence of acantholytic and dyskeratotic cells at the FAD was reached. The patient was then admitted to epidermis. While FAD can be observed in many various hospital for treatment with doxycycline 100 mg and cutaneous lesions including benign and/or malignant antihistamines. After one week, the lesions had remarka- epithelial lesions, fibrohistiocytic lesions, inflammatory bly improved. The patient was then discharged, and lesions, melanocytic and/or follicular lesions2-4. These continued on the same therapeutic regimen for an histopathological findings may also extend into the additional month, bythe time all lesions were nearly surrounding tissues, which often appear to be clinically resolved. normal. A 42-year-old woman was presented to our To date, the etiology of FAD has been attributed to department with multiple erythematous pruritic papules numerous sources including hormones, viral infection, and tiny vesicles on her face. -

UC Davis Dermatology Online Journal
UC Davis Dermatology Online Journal Title Multiple acantholytic dyskeratotic acanthomas in a liver-transplant recipient Permalink https://escholarship.org/uc/item/24v5t78z Journal Dermatology Online Journal, 25(4) Authors Kanitakis, Jean Gouillon, Laurie Jullien, Denis et al. Publication Date 2019 DOI 10.5070/D3254043575 License https://creativecommons.org/licenses/by-nc-nd/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Volume 25 Number 4| April 2019| Dermatology Online Journal || Case Presentation 25(4):6 Multiple acantholytic dyskeratotic acanthomas in a liver- transplant recipient Jean Kanitakis1,2, Laurie Gouillon1, Denis Jullien1, Emilie Ducroux1 Affiliations: 1Department of Dermatology, Edouard Herriot Hospital Group, Lyon, France, 2Department of Pathology, Centre Hospitalier Lyon Sud, Pierre Bénite, France Corresponding Author: Jean Kanitakis, Department of Dermatology, Edouard Herriot Hospital Group (Pavillion R), 69437 Lyon cedex 03, France, Tel: 33-472110301, Email: [email protected] (0.5mg/d) and prednisolone (5mg/d). He had Abstract recently developed end-stage renal disease and was Acantholytic dyskeratotic acanthoma is a rare variant undergoing hemodialysis. His post-transplant of epidermal acanthoma characterized pathologically medical history was significant for two melanomas by the presence of acantholysis and dyskeratosis. (one in situ on the abdomen diagnosed at the age of Few cases have been reported until now, one of them 61 years and a superficial spreading melanoma in a heart-transplant patient. We present here a new 2.4mm Breslow thickness of the dorsum of the foot case of this rare lesion that developed in a liver- diagnosed ten years later), a squamous cell transplant patient and review the salient features of this uncommon condition. -
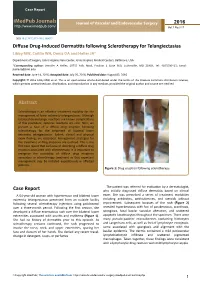
Diffuse Drug-Induced Dermatitis Following Sclerotherapy for Telangiectasias Libby MW, Caitlin WH, Deniz OA and Heller JA*
Case Report iMedPub Journals Journal of Vascular and Endovascular Surgery 2016 http://www.imedpub.com/ Vol.1 No.3:17 DOI: 10.21767/2573-4482.100017 Diffuse Drug-Induced Dermatitis following Sclerotherapy for Telangiectasias Libby MW, Caitlin WH, Deniz OA and Heller JA* Department of Surgery, Johns Hopkins Vein Center, Johns Hopkins Medical Centers, Baltimore, USA *Corresponding author: Jennifer A Heller, 10755 Falls Road, Pavilion 1 Suite 360, Lutherville, MD 21903, Tel: 4105500415; Email: [email protected] Received date: June 14, 2016; Accepted date: July 26, 2016; Published date: August 02, 2016 Copyright: © 2016 Libby MW, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Sclerotherapy is an effective treatment modality for the management of lower extremity telangiectasias. Although localized dermatologic reactions are known complications of this procedure, systemic reactions are rare. Here, we present a case of a diffuse drug eruption following sclerotherapy for the treatment of bilateral lower extremity telangiectasias. Salient clinical and physical exam findings are described. Management strategies for the treatment of drug eruptions are outlined. This is the first case report that we know of describing a diffuse drug eruption associated with sclerotherapy. It is important to recognize the possibility of diffuse drug eruptions secondary to sclerotherapy treatment so that expectant management may be initiated expeditiously in affected patients. Figure 1: Drug eruption following sclerotherapy. The patient was referred for evaluation by a dermatologist, Case Report who initially diagnosed diffuse dermatitis based on clinical A 64-year-old woman with hypertension and bilateral lower exam. -

Trichoscopic Findings in Various Scalp Alopecias Unilateral Truncal Acne A�Er Laminectomy Armoured Keloid Werner's Syndrome: a Rare En�Ty
JDA IJCD Indian Journal of Clinical Dermatology ` 800 - Jaipur Volume 2 | Issue 1 | May 2019 Four Monthly HIGHLIGHTS Sunscreens: The Current Scenario Trichoscopic Findings in Various Scalp Alopecias Unilateral Truncal Acne Aer Laminectomy Armoured Keloid Werner's Syndrome: A Rare Enty Clin of ica al l D rn e u r o m J a t n o a l i o d g n y I A Publication of Jaipur Dermatology Association Clin of ica JDA al l D rn e u r o m J a t n o INDIAN JOURNAL OF a l i o d g n y I CLINICAL DERMATOLOGY A Publication of Jaipur Dermatology Association EDITORIAL BOARD EDITORS DR. DINESH MATHUR DR. U S AGARWAL Prof & Head, Dept. of Skin, JNU Medical College Senior Professor, Ex. Sr. Prof & Head, Dept. of Skin, Dept. of Skin, STD & Leprosy STD & Leprosy, SMS Medical College Ex. Principal & Controller, Ex. Pro VC, RUHS SMS Medical College & Hospital, Jaipur Email: [email protected] Email: [email protected] EXECUTIVE EDITOR Dr. Puneet Agarwal Assistant Professor, Dept. of Skin, STD & Leprosy, SMS Medical College & Hospital, Jaipur Email: [email protected] ASSISTANT EDITORS Dr. Naushin Aara Assistant Professor Dept. of Skin, STD & Leprosy, SMS Medical College & Hospital, Jaipur Email: [email protected] Dr. Taniya Mehta Ex. Senior Resident Dept. of Skin, STD & Leprosy, SMS Medical College & Hospital, Jaipur Email: [email protected] JDA Indian Journal of Clinical Dermatology | Volume 02 | Issue 01 | May 2019 i Clin of ica JDA al l D rn e u r o m J a t n o INDIAN JOURNAL OF a l i o d g n y I CLINICAL DERMATOLOGY A Publication of Jaipur Dermatology Association Volume 02 | Issue 01 | August 2019 COPYRIGHT The entire contents of the Indian Journal of Clinical Dermatology are protected under Indian and International copyrights. -

Actinic Keratosis Squamous Cell Carcinoma in Situ
Prepared by Kurt Schaberg Keratinocyte tumors Actinic Keratosis Precancerous , risk of malignancy ~8-20% per year (progresses to SCC); Due to chronic sun exposure Rough scaly plaque; typically due to sun exposure Tx : liquid nitrogen, 5-FU, shave, curettage • Atypical keratinocytes in lower third of epidermis • Alternating orthokeratosis and parakeratosis • Sparing of cutaneous adnexa • Solar elastosis in dermis Squamous cell carcinoma in situ (aka Bowen’s disease) • No epidermal maturation • Atypical cells at all levels of the epidermis Loss of granular layer • Epidermis appears disorganized Squamous Cell Carcinoma Second most common form of skin cancer (20% of cutaneous malignancies) Locally destructive; metastatic potential Tx: Depends on size, location and depth of invasion: Excision, Mohs micrographic surgery, Radiation • Nests of atypical squamous cells arise from the epidermis and invade the dermis • Evidence of squamous differentiation (keratinization and intercellular bridges) • Dyskeratotic cells = squamous differentiation Risk factors for metastasis (high risk): • Often associated with AK or SCCIS - location (ear, lip) • Findings that suggest invasion - size (>2 cm) • Jagged interface with dermis - depth • Aberrant deep keratinization - evidence of perineural invasion - evidence of desmoplastic • Single cells invasion features Variants: Keratoacanthoma - well-differentiated variant of SCC that spontaneously regresses in most cases. Typically composed of large, crateriform (cup-like) lesion filled with abundant keratin debris -

Oral Cavity 3 J.W
Chapter 3 Oral Cavity 3 J.W. Eveson Contents 3.1 Embryonic Rests and Heterotopias . 72 3.5.4 Addison Disease . 88 3.1.1 Fordyce Granules/Spots . 72 3.5.5 Peutz Jeghers Syndrome . 89 3.1.2 Juxtaoral Organ of Chievitz . 72 3.5.6 Racial Pigmentation . 89 3.5.7 Laugier Hunziker Syndrome . 89 3.2. Vesiculo-Bullous Diseases . 72 3.5.8 Smoker’s Melanosis . 89 3.2.1 Herpes Simplex Infections . 72 3.5.9 Drug-Associated Oral Pigmentation . 90 3.2.2 Chickenpox and Herpes Zoster . 73 3.2.3 Hand-Foot-and-Mouth Disease . 73 3.6 Hyperplastic Lesions . 90 3.2.4 Herpangina . 74 3.6.1 Fibrous Hyperplasias . 90 3.2.5 Pemphigus Vulgaris . 74 3.6.2 Papillary Hyperplasia . 90 3.2.6 Pemphigus Vegetans . 74 3.6.3 Generalised Gingival Fibrous Hyperplasia . 91 3.2.7 Paraneoplastic Pemphigus . 75 3.6.4 Crohn’s Disease . 91 3.2.8 Mucous Membrane Pemphigoid . 75 3.6.5 Orofacial Granulomatosis . 92 3.2.9 Dermatitis Herpetiformis . 76 3.6.6 Chronic Marginal Gingivitis 3.2.10 Linear IgA Disease . 76 and Localised Gingival Fibrous Hyperplasia . 92 3.2.11 Erythema Multiforme . 77 3.6.7 Peripheral Giant Cell Granuloma (Giant Cell Epulis) . 93 3.3 Ulcerative Lesions . 77 3.6.8 Pyogenic Granuloma . 93 3.3.1 Aphthous Stomatitis 3.6.9 Pulse (Vegetable) Granuloma . 93 (Recurrent Aphthous Ulceration) . 77 3.3.2 Behçet Disease . 78 3.7 Benign Tumours and Pseudotumours . 94 3.3.3 Reiter Disease . 78 3.7.1 Giant Cell Fibroma .