The Immune System and Kidney Disease: Basic Concepts and Clinical Implications
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Primer the Complement System
View metadata, citation and similar papers at core.ac.uk brought to you by CORE providedMagazine by ElsevierR259 - Publisher Connector vascular permeability and the infection. The second category Primer extravasation of plasma. This is in which there is persistent accompanied by the adhesion of formation of immune complexes is leukocytes to vascular endothelium autoimmune disease, in which, by The complement and their emigration into definition, the antigen is a system surrounding tissue. Complement permanent feature of the host. plays an important part in An understanding of how immune Philip Taylor, Marina inflammation, in helping to recruit complexes cause tissue injury effector cells and in promoting the developed from study of such Botto and Mark Walport killing and clearance of pathogens. diseases in humans and animals, and But complement can be both from the induction of experimental The system of plasma proteins called friend and foe. In some immune complex disease. In these complement was so-named because circumstances the activation of situations, immune complexes were it complements the activity of complement in response to immune shown to cause tissue injury through antibody in the lysis of bacteria. It complexes may cause harm: acutely activation of complement, as opsonin has a central role in host defence in the context of massive (binding to complement receptors on against many micro-organisms and in complement activation occurring in leukocytes) and as the source of the modulation of inflammatory patients with overwhelming Gram- anaphylatoxins (stimulating leukocyte reactions, an activity that has been negative bacterial sepsis, and chemotaxis and degranulation). But illuminated by the study of humans chronically, when an antibody the development of gene-targeted with naturally occurring deficiencies response develops in the context of mice with deficiencies of complement of complement. -

Donor-Alloantigen-Reactive Regulatory T Cell Therapy in Liver
Confidential Page 1 of 80 Donor-Alloantigen-Reactive Regulatory T Cell Therapy in Liver Transplantation Version 7.0/ August 1, 2018 IND# 15479 Study Sponsor(s): The National Institute of Allergy and Infectious Diseases (NIAID) Grant #: R34AI095135 and U01AI110658-01 Study Drug Manufacturer/Provider: Sanofi US PRINCIPAL INVESTIGATOR CO- PRINCIPAL INVESTIGATOR CO- PRINCIPAL INVESTIGATOR SANDY FENG, MD, PHD JEFFREY BLUESTONE, PHD SANG-MO KANG, MD, FACS Professor of Surgery Executive Vice Chancellor and Provost Associate Professor Director, Abdominal Transplant A.W. Clausen Distinguished Professor University of California, San Surgery Fellowship in Medicine Francisco University of California, San University of California, San Francisco 513 Parnassus Ave. Francisco 513 Parnassus Ave. Box 0780, HSE-520 505 Parnassus Ave. Box 0400, HSW-1128 San Francisco, CA 94143-0780 Box 0780, M-896 San Francisco, CA 94143-0780 Phone: (415) 353-1888 San Francisco, CA 94143-0780 Phone: (415) 476-4451 E-mail: Sang- Phone: (415) 353-8725 Fax: (415) 476-9634 [email protected] Fax: (415) 353-8709 E-mail: [email protected] E-mail: [email protected] CO- PRINCIPAL INVESTIGATOR BIOSTATISTICIAN MEDICAL OFFICER QIZHI TANG, PHD DAVID IKLÉ, PHD NANCY BRIDGES, MD Associate Professor Senior Statistical Scientist Chief, Transplantation Branch Director, UCSF Transplantation Rho, Inc. Division of Allergy, Immunology, Research Lab 6330 Quadrangle Drive and Transplantation University of California, San Chapel Hill, NC 27517 NIAID Francisco Phone: (910) 558-6678 -

Java Based Distributed Learning Platform
Journal of Pharmacy and Pharmacology 8 (2020) 110-123 doi: 10.17265/2328-2150/2020.04.003 D DAVID PUBLISHING Blood Group Cartography (ABO, RHESUS, KELL and DUFFY) and Hemogram of Icteric Newborn in Sendwe Hospital, Lubumbashi/D.R.C Monga Kalenga J. J1, Monga Ngoy Davidson2, Matanda Kapend Serge3, Masendu Kalenga Paulin4, Haumont Dominique5 and Luboya Numbi Oscar1 1. Department of Pediatrics, Faculty of Medicine, University of Lubumbashi, Haut-Katanga 1825, DRC. 2. Laboratory Department Head Sendwe Hospital, Haut Katanga, Lubumbashi 1825, DRC 3. Department of Internal Medicine, Faculty of Medicine, University of Lubumbashi, Haut-Katanga 1825, DRC. 4. CHR The Citadel, Neonatology Department, University of Liège, Liège 4450, Belgium. 5. Free University of Brussels, Brussels 1050, Belgium Abstract: Background: Allo immunization jaundice is a common cause of neonatal jaundice. According to racial group the concerned blood group may not be the same. In our Country people are exposed to high transfusionnal risk because of malaria and sicklanemia and the blood group research in laboratory include only ABO/D. Objective: Our objective was to establish a blood group cartography of this icteric newborn population and their mother; the frequency of rare blood group and the compatibility level between mother and newborn. Our interest was also to study hemogram of this population. Methodology: We studied blood group ABO/D; RH/Kell and Duffy of 56 newborn whom developped an indirect bilirubin and their mothers. We performed bilrubin level and hemogram. Results: The frequency of icteric newborn was 17.17%. The mother blood mapping was O (60.71%), RhD positive (83.9%), C negative (91.07%) E negative (89.29%) c positive (91.07%), epositive (92.86%), kell negative (100%) and duffy null (100%). -

Humoral Alloimmunity in Cardiac Allograft Rejection
Humoral alloimmunity in cardiac allograft rejection Jawaher Alsughayyir Darwin College Department of Surgery University of Cambridge This dissertation is submitted for the degree of Doctor of Philosophy July 2018 i Declaration This dissertation is the result of my own work and includes nothing which is the outcome of work done in collaboration except where declared in the text. It has not been submitted in whole or part for a degree at any university. The length of this thesis does not exceed the 60,000 word limit i Dissertation title: Humoral alloimmunity in cardiac allograft rejection Student name: Jawaher Alsughayyir Abstract Although the short-term outcomes of solid allograft survival have improved substantially over the last few decades, there has been no significant improvement in long-term survival of solid allografts. This thesis presents the initial characterisation of alloantibody mediated rejection in a murine heart transplant model, with particular focus on the impact of the different phases of the humoral alloimmune response (follicular or germinal centre) on graft rejection. The key findings of this work are: 1) The precursor frequency of allospecific CD4 T cells determines the magnitude of the alloantibody response, with a relatively high frequency of CD4 T cells eliciting strong extrafollicular responses, while a high frequency of B cells promotes slowly-developing germinal centre responses. 2) Strong extrafollicular antibody response can mediate acute heart allograft rejection in the absence of CD8 T cells alloresponses. 3) Germinal centre humoral immunity mediates chronic antibody-mediated rejection. 4) Recipient memory, but not naïve, CD4 T cells that recognise one graft alloantigen can provide ‘unlinked’ help to allospecific B cells that recognise a different graft alloantigen for generating germinal centre alloantibody responses. -
Foundation Block Lecture Three Cell Mediated Immunity
Foundation Block Lecture Five Hypersensitivity Objectives: • To know that hypersensitivity reactions are over and excessive immune responses that can be harmful to body in four different ways • To be familiar with inflammatory processes in type I hypersensitivity reaction that mediates allergic inflammation • To recognize that type II hypersensitivity deals with immune responses against antigens that are integral part of cell membrane and are usually associated with autoimmune disorders • To know that type III hypersensitivity reactions are mediated by immune complexes and cause vasculitis • To describe type IV hypersensitivity is a purely cell mediated immune response associated with chronic inflammation ● Important. ● Extra notes. ● Females notes ● Males notes. What is hypersensitivity? Protective immunity: desirable reaction. Hypersensitivity: undesirable damaging reaction produced by excessive immune reactions. - Undesirable responses can be mediated by: - Antibody binding to antigens (Types I-III). - Cell mediated reaction to chemicals or proteins (Type IV). Types of hypersensitivity: 4 Types of hypersensitivity responses are classified by GEL AND COOMBS (names of scientists) according to the responding mechanisms, NOT the responding antigens: *From 433 team Type I: 1- Also termed as: - Immediate Hypersensitivity. - Allergic reactions. (e.g. asthma and eczema) - Anaphylactic reactions: severe and rapidly progressing systemic forms which can be quickly life threatening. …..............(causes.vasodilation and hypovolemia which causes heart stop then death) 2- Most people will not react to these allergens but some individuals “atopic” respond by producing large amounts of IgE in …........response to those otherwise harmless substances. 3- Non-allergic individuals respond to these allergens by producing IgG antibodies. 4- Features: - Antibody type: IgE - Cellular components: Mast cells, basophiles & eosinophils - Antigens: Also known as allergens ( antigens with low molecular weight & highly soluble). -

Effects of Glycosylation on the Enzymatic Activity and Mechanisms of Proteases
International Journal of Molecular Sciences Review Effects of Glycosylation on the Enzymatic Activity and Mechanisms of Proteases Peter Goettig Structural Biology Group, Faculty of Molecular Biology, University of Salzburg, Billrothstrasse 11, 5020 Salzburg, Austria; [email protected]; Tel.: +43-662-8044-7283; Fax: +43-662-8044-7209 Academic Editor: Cheorl-Ho Kim Received: 30 July 2016; Accepted: 10 November 2016; Published: 25 November 2016 Abstract: Posttranslational modifications are an important feature of most proteases in higher organisms, such as the conversion of inactive zymogens into active proteases. To date, little information is available on the role of glycosylation and functional implications for secreted proteases. Besides a stabilizing effect and protection against proteolysis, several proteases show a significant influence of glycosylation on the catalytic activity. Glycans can alter the substrate recognition, the specificity and binding affinity, as well as the turnover rates. However, there is currently no known general pattern, since glycosylation can have both stimulating and inhibiting effects on activity. Thus, a comparative analysis of individual cases with sufficient enzyme kinetic and structural data is a first approach to describe mechanistic principles that govern the effects of glycosylation on the function of proteases. The understanding of glycan functions becomes highly significant in proteomic and glycomic studies, which demonstrated that cancer-associated proteases, such as kallikrein-related peptidase 3, exhibit strongly altered glycosylation patterns in pathological cases. Such findings can contribute to a variety of future biomedical applications. Keywords: secreted protease; sequon; N-glycosylation; O-glycosylation; core glycan; enzyme kinetics; substrate recognition; flexible loops; Michaelis constant; turnover number 1. -

Serine Proteases with Altered Sensitivity to Activity-Modulating
(19) & (11) EP 2 045 321 A2 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 08.04.2009 Bulletin 2009/15 C12N 9/00 (2006.01) C12N 15/00 (2006.01) C12Q 1/37 (2006.01) (21) Application number: 09150549.5 (22) Date of filing: 26.05.2006 (84) Designated Contracting States: • Haupts, Ulrich AT BE BG CH CY CZ DE DK EE ES FI FR GB GR 51519 Odenthal (DE) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI • Coco, Wayne SK TR 50737 Köln (DE) •Tebbe, Jan (30) Priority: 27.05.2005 EP 05104543 50733 Köln (DE) • Votsmeier, Christian (62) Document number(s) of the earlier application(s) in 50259 Pulheim (DE) accordance with Art. 76 EPC: • Scheidig, Andreas 06763303.2 / 1 883 696 50823 Köln (DE) (71) Applicant: Direvo Biotech AG (74) Representative: von Kreisler Selting Werner 50829 Köln (DE) Patentanwälte P.O. Box 10 22 41 (72) Inventors: 50462 Köln (DE) • Koltermann, André 82057 Icking (DE) Remarks: • Kettling, Ulrich This application was filed on 14-01-2009 as a 81477 München (DE) divisional application to the application mentioned under INID code 62. (54) Serine proteases with altered sensitivity to activity-modulating substances (57) The present invention provides variants of ser- screening of the library in the presence of one or several ine proteases of the S1 class with altered sensitivity to activity-modulating substances, selection of variants with one or more activity-modulating substances. A method altered sensitivity to one or several activity-modulating for the generation of such proteases is disclosed, com- substances and isolation of those polynucleotide se- prising the provision of a protease library encoding poly- quences that encode for the selected variants. -

A Potential Role in the D-Binding Protein (Gc-Globulin) to Elastase
Elastase Controls the Binding of the Vitamin D-Binding Protein (Gc-Globulin) to Neutrophils: A Potential Role in the Regulation of C5a Co-Chemotactic Activity This information is current as of September 26, 2021. Stephen J. DiMartino, Anisha B. Shah, Glenda Trujillo and Richard R. Kew J Immunol 2001; 166:2688-2694; ; doi: 10.4049/jimmunol.166.4.2688 http://www.jimmunol.org/content/166/4/2688 Downloaded from References This article cites 64 articles, 19 of which you can access for free at: http://www.jimmunol.org/content/166/4/2688.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 26, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2001 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Elastase Controls the Binding of the Vitamin D-Binding Protein (Gc-Globulin) to Neutrophils: A Potential Role in the Regulation of C5a Co-Chemotactic Activity1 Stephen J. DiMartino, Anisha B. -

Suppression of Immune Complex-Induced Inflammation by the Chemotactic Factor Inactivator
Suppression of immune complex-induced inflammation by the chemotactic factor inactivator. K J Johnson, … , T P Anderson, P A Ward J Clin Invest. 1977;59(5):951-958. https://doi.org/10.1172/JCI108717. Research Article Small amounts (10(-10) mol) of purified human chemotactic factor inactivator (CFI) suppress leukocytic infiltration, permeability changes, and hemorrhage associated with acute immune complex-induced injury in rats. The reversed passive dermal Arthus reaction and acute immune complex-induced alveolitis in rats have served as the model systems of inflammation. The mechanism of inhibition does not appear to relate to interference with formation and deposition of immune complexes, or with fixation of complement in vitro or iv vivo. Human CFI inhibits in vitro the chemotactic activity generated in complement-activated rat serum. The inhibitory effects of human CFI are not seen if it is first heat inactivated. The data provide the first direct support for the conclusion that CFI has anti-inflammatory activity. Find the latest version: https://jci.me/108717/pdf Suppression of Immune Complex-Induced Inflammation by the Chemotactic Factor Inactivator KENT J. JOHNSON, THOMAS P. ANDERSON, and PETER A. WARD From the Department of Pathology, University of Connecticut Health Center, Farmington, Connecticut 06032 A B S T RA C T Small amounts (10-10 mol) of purified fested by skin tests (7-10). These observations have human chemotactic factor inactivator (CFI) suppress suggested that CFI is an important regulator of the leukocytic infiltration, permeability changes, and inflammatory response. In this communication direct hemorrhage associated with acute immune complex- evidence is presented to show that purified human CFI induced injury in rats. -
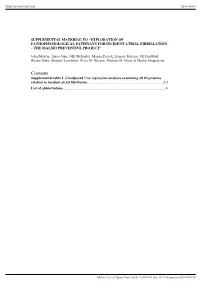
Contents Supplemental Table 1
Supplementary material Open Heart SUPPLEMENTAL MATERIAL TO “EXPLORATION OF PATHOPHYSIOLOGICAL PATHWAYS FOR INCIDENT ATRIAL FIBRILLATION – THE MALMÖ PREVENTIVE PROJECT” John Molvin, Amra Jujic, Olle Melander, Manan Pareek, Lennart Råstam, Ulf Lindblad, Bledar Daka, Margrét Leósdóttir, Peter M. Nilsson, Michael H. Olsen & Martin Magnusson Contents Supplemental table 1. Unadjusted Cox regression analyses examining all 92 proteins relation to incident atrial fibrillation ................................................................................... 2-3 List of abbreviations……………………………………………………………………………………………………………4 Molvin J, et al. Open Heart 2020; 7:e001190. doi: 10.1136/openhrt-2019-001190 Supplementary material Open Heart Supplemental table 1. Unadjusted Cox regression analyses examining all 92 proteins relation to incident atrial fibrillation Protein Hazard ratio (95% confidence interval) p-value PON3 0.80 (0.72-0.89) 7.3x10-5 IGFBP2 4.47 (1.42-14-1) 0.011 PAI 1.44 (0.65-3.18) 0.371 CTSD 2.45 (1.13-5.30) 0.023 FABP4 1.27 (1.13-1.44) 8.6x10-5 CD163 5.25 (1.14-24.1) 0.033 GAL4 1.30 (1.15-1.47) 3.5x10-5 LDL-receptor 0.81 (0.39-1.69) 0.582 IL1RT2 0.75 (0.24-2.34) 0.614 t-PA 2.75 (1.21-6.27) 0.016 SELE 0.99 (0.51-1.90) 0.969 CTSZ 2.97 (1.00-8.78) 0.050 GDF15 1.41 (1.25-1.59) 9.7x10-9 CSTB 3.75 (1.58-8.92) 0.003 MPO 4.48 (1.73-11.7) 0.002 PCSK9 1.18 (0.73-1.93) 0.501 IGFBP1 2.48 (1.42-4.35) 0.001 RARRES2 64.3 (1.87-2220.8) 0.021 ITGB2 1.01 (0.31-3.29) 0.990 CCL15 3.58 (0.96-13.3) 0.057 SCGB3A2 0.97 (0.71-1.32) 0.839 CHI3L1 1.26 (1.12-1.43) -

Understanding IDIOPATHIC PULMONARY FIBROSIS (IPF)
Understanding IDIOPATHIC PULMONARY FIBROSIS (IPF) An educational health series from National Jewish Health National Jewish Health Our Mission since 1899 is to heal, to discover, and to educate as a preeminent healthcare institution. We serve by providing the best integrated and innovative care for patients and their families; by understanding and finding cures for the diseases we research; and by educating and training the next generation of healthcare professionals to be leaders in medicine and science. njhealth.org Understanding IDIOPATHIC PULMONARY FIBROSIS (IPF) An educational health series from National Jewish Health® In this Issue What is Idiopathic Pulmonary Fibrosis or IPF? 2 Living a Full Life With IPF 6 Healthy Lifestyle 8 Treatment of IPF 12 Avoiding Infections 13 Medications 14 Oxygen Therapy 15 Breathing Techniques 17 Lung Transplant 18 Action Plan for IPF 19 Living a Full Life at Any Stage of IPF 21 Stage 1 22 Stage 2 26 Stage 3 29 Stage 4 31 Note: This information is provided to you as an educational service of National Jewish Health. It is not meant as a substitute for your own doctor. © Copyright 2017, National Jewish Health Materials were developed through a partnership between National Jewish Health and PVI, PeerView Institute for Medical Education. What is Idiopathic Pulmonary Fibrosis or IPF? What is Idiopathic Pulmonary Fibrosis or IPF? Interstitial lung disease (ILD) is a broad category of lung diseases that includes more than 200 disorders that can be characterized by fibrosis (scarring) and/or inflammation of the lungs. Despite an exhaustive evaluation, in many people the cause of ILD remains unknown. -

Understanding the Immune System: How It Works
Understanding the Immune System How It Works U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES NATIONAL INSTITUTES OF HEALTH National Institute of Allergy and Infectious Diseases National Cancer Institute Understanding the Immune System How It Works U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES NATIONAL INSTITUTES OF HEALTH National Institute of Allergy and Infectious Diseases National Cancer Institute NIH Publication No. 03-5423 September 2003 www.niaid.nih.gov www.nci.nih.gov Contents 1 Introduction 2 Self and Nonself 3 The Structure of the Immune System 7 Immune Cells and Their Products 19 Mounting an Immune Response 24 Immunity: Natural and Acquired 28 Disorders of the Immune System 34 Immunology and Transplants 36 Immunity and Cancer 39 The Immune System and the Nervous System 40 Frontiers in Immunology 45 Summary 47 Glossary Introduction he immune system is a network of Tcells, tissues*, and organs that work together to defend the body against attacks by “foreign” invaders. These are primarily microbes (germs)—tiny, infection-causing Bacteria: organisms such as bacteria, viruses, streptococci parasites, and fungi. Because the human body provides an ideal environment for many microbes, they try to break in. It is the immune system’s job to keep them out or, failing that, to seek out and destroy them. Virus: When the immune system hits the wrong herpes virus target or is crippled, however, it can unleash a torrent of diseases, including allergy, arthritis, or AIDS. The immune system is amazingly complex. It can recognize and remember millions of Parasite: different enemies, and it can produce schistosome secretions and cells to match up with and wipe out each one of them.