Alzheimer Syllabus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Opioid-Induced Hyperalgesia in Humans Molecular Mechanisms and Clinical Considerations
SPECIAL TOPIC SERIES Opioid-induced Hyperalgesia in Humans Molecular Mechanisms and Clinical Considerations Larry F. Chu, MD, MS (BCHM), MS (Epidemiology),* Martin S. Angst, MD,* and David Clark, MD, PhD*w treatment of acute and cancer-related pain. However, Abstract: Opioid-induced hyperalgesia (OIH) is most broadly recent evidence suggests that opioid medications may also defined as a state of nociceptive sensitization caused by exposure be useful for the treatment of chronic noncancer pain, at to opioids. The state is characterized by a paradoxical response least in the short term.3–14 whereby a patient receiving opioids for the treatment of pain Perhaps because of this new evidence, opioid may actually become more sensitive to certain painful stimuli. medications have been increasingly prescribed by primary The type of pain experienced may or may not be different from care physicians and other patient care providers for the original underlying painful condition. Although the precise chronic painful conditions.15,16 Indeed, opioids are molecular mechanism is not yet understood, it is generally among the most common medications prescribed by thought to result from neuroplastic changes in the peripheral physicians in the United States17 and accounted for 235 and central nervous systems that lead to sensitization of million prescriptions in the year 2004.18 pronociceptive pathways. OIH seems to be a distinct, definable, One of the principal factors that differentiate the use and characteristic phenomenon that may explain loss of opioid of opioids for the treatment of pain concerns the duration efficacy in some cases. Clinicians should suspect expression of of intended use. -

E30 SEM. O.C. Disclosed Is a Compound Represented by the Formula (1) (51) Int
USOO9453000B2 (12) United States Patent (10) Patent No.: US 9.453,000 B2 Kimura et al. (45) Date of Patent: *Sep. 27, 2016 (54) POLYCYCLIC COMPOUND (56) References Cited (75) Inventors: Teiji Kimura, Tsukuba (JP); Noritaka U.S. PATENT DOCUMENTS Kitazawa, Tsukuba (JP); Toshihiko 3,470,167 A 9, 1969 Sarkar Kaneko, Tsukuba (JP); Nobuaki Sato, 3,989,816 A 1 1/1976 Rajadhyaksha Tsukuba (JP); Koki Kawano, Tsukuba 4,910,200 A 3, 1990 Curtze et al. (JP): Koichi Ito, Tsukuba (JP); 5,281,626 A 1/1994 Oinuma et al. M s Tak ishi Tsukub JP 5,563,162 A 10, 1996 Oku et al. amoru Takaishi Tsukuba (JP); 5,804,577 A 9, 1998 Hebeisen et al. Takeo Sasaki, Tsukuba (JP); Yu 5,985,856 A 11/1999 Stella et al. Yoshida, Tsukuba (JP); Toshiyuki 6,235,728 B1 5, 2001 Golik et al. Uemura, Tsukuba (JP); Takashi Doko, g R 1939. E. al. Its SE E. Shinmyo, 7,138.414 B2 11/2006 Schoenafingereatch et al. et al. sukuba (JP); Daiju Hasegawa, 7,300,936 B2 11/2007 Parker et al. Tsukuba (JP); Takehiko Miyagawa, 7,314,940 B2 1/2008 Graczyk et al. Hatfield (GB); Hiroaki Hagiwara, 7,618,960 B2 11/2009 Kimura et al. Tsukuba (JP) 7,667,041 B2 2/2010 Kimura et al. 7,687,640 B2 3/2010 Kimura et al. 7,713,993 B2 5/2010 Kimura et al. (73) Assignee: EISAI R&D MANAGEMENT CO., 7,737,141 B2 6/2010 Kimura et al. LTD., Tokyo (JP) 7,880,009 B2 2/2011 Kimura et al. -

WITHOUTUS010307409B2 (12 ) United States Patent ( 10 ) Patent No
WITHOUTUS010307409B2 (12 ) United States Patent ( 10 ) Patent No. : US 10 , 307 ,409 B2 Chase et al. (45 ) Date of Patent: Jun . 4 , 2019 ( 54 ) MUSCARINIC COMBINATIONS AND THEIR (52 ) U . S . CI. USE FOR COMBATING CPC . .. .. A61K 31/ 4439 (2013 . 01 ) ; A61K 9 /0056 HYPOCHOLINERGIC DISORDERS OF THE (2013 . 01 ) ; A61K 9 / 7023 ( 2013 . 01 ) ; A61K CENTRAL NERVOUS SYSTEM 31 / 166 ( 2013 . 01 ) ; A61K 31 / 216 ( 2013 . 01 ) ; A61K 31 /4178 ( 2013 .01 ) ; A61K 31/ 439 (71 ) Applicant: Chase Pharmaceuticals Corporation , ( 2013 .01 ) ; A61K 31 /44 (2013 . 01 ) ; A61K Washington , DC (US ) 31/ 454 (2013 .01 ) ; A61K 31/ 4725 ( 2013 .01 ) ; A61K 31 /517 (2013 .01 ) ; A61K 45 / 06 ( 72 ) Inventors : Thomas N . Chase , Washington , DC (2013 . 01 ) (US ) ; Kathleen E . Clarence -Smith , ( 58 ) Field of Classification Search Washington , DC (US ) CPC .. A61K 31/ 167 ; A61K 31/ 216 ; A61K 31/ 439 ; A61K 31 /454 ; A61K 31 /4439 ; A61K (73 ) Assignee : Chase Pharmaceuticals Corporation , 31 /4175 ; A61K 31 /4725 Washington , DC (US ) See application file for complete search history. ( * ) Notice : Subject to any disclaimer, the term of this (56 ) References Cited patent is extended or adjusted under 35 U . S . C . 154 (b ) by 0 days . U . S . PATENT DOCUMENTS 5 ,534 ,520 A 7 / 1996 Fisher et al. ( 21) Appl . No. : 15 /260 , 996 2008 /0306103 Al 12 /2008 Fisher et al. 2011/ 0021503 A1* 1/ 2011 Chase . .. A61K 31/ 27 ( 22 ) Filed : Sep . 9 , 2016 514 / 215 2011/ 0071135 A1 * 3 / 2011 Chase . .. .. .. A61K 31/ 166 (65 ) Prior Publication Data 514 / 215 2011 /0245294 Al 10 / 2011 Paborji et al. -

Wo 2007/128674 A2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (43) International Publication Date (10) International Publication Number 15 November 2007 (15.11.2007) PCT WO 2007/128674 A2 (51) International Patent Classification: Houtenlaan 36, NL-1381 CP Weesp (NL). KRUSE, Cor- A61K 31/00 (2006.01) A61K 31/551 (2006.01) nelis G. [NL/NL]; c/o SOLVAY PHARMACEUTICALS A61K 31/439 (2006.01) A61P 25/18 (2006.01) B.V., IPSI Department, CJ. Van Houtenlaan 36, NL-1381 A61K 31/4439 (2006.01) CP Weesp (NL). (21) International Application Number: (74) Agent: VERHAGE, Marinus; Octrooibureau Zoan B.V., PCT/EP2007/053934 NL-1380 AC Weesp (NL). (22) International Filing Date: 23 April 2007 (23.04.2007) (81) Designated States (unless otherwise indicated, for every kind of national protection available): AE, AG, AL, AM, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, (25) Filing Language: English CN, CO, CR, CU, CZ, DE, DK, DM, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, (26) Publication Language: English IS, JP, KE, KG, KM, KN, KP, KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY,MA, MD, MG, MK, MN, MW, MX, MY, (30) Priority Data: MZ, NA, NG, NI, NO, NZ, OM, PG, PH, PL, PT, RO, RS, 061 13476.3 4 May 2006 (04.05.2006) EP RU, SC, SD, SE, SG, SK, SL, SM, SV, SY, TJ, TM, TN, 60/797,355 4 May 2006 (04.05.2006) US TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW (71) Applicant (for all designated States except US): SOLVAY (84) Designated States (unless otherwise indicated, for every PHARMACEUTICALS B.V. -

Role of a Hippocampal Src-Family Kinase-Mediated Glutamatergic Mechanism in Drug Context-Induced Cocaine Seeking
Neuropsychopharmacology (2013) 38, 2657–2665 & 2013 American College of Neuropsychopharmacology. All rights reserved 0893-133X/13 www.neuropsychopharmacology.org Role of a Hippocampal Src-Family Kinase-Mediated Glutamatergic Mechanism in Drug Context-Induced Cocaine Seeking 1 1 1 1 ,1 Xiaohu Xie , Amy A Arguello , Audrey M Wells , Andrew M Reittinger and Rita A Fuchs* 1 Department of Psychology, University of North Carolina, Chapel Hill, NC, USA Glutamatergic neurotransmission in the dorsal hippocampus (DH) is necessary for drug context-induced reinstatement of cocaine- seeking behavior in an animal model of drug relapse. Furthermore, in vitro studies suggest that the Src family of tyrosine kinases critically regulates glutamatergic cellular functions within the DH. Thus, Src-family kinases in the DH may similarly control contextual cocaine- seeking behavior. To test this hypothesis, rats were trained to lever press for un-signaled cocaine infusions in a distinct context followed by extinction training in a different context. Cocaine-seeking behavior (non-reinforced active lever pressing) was then assessed in the previously cocaine-paired and extinction contexts after AP5 (N-methyl-D-aspartate glutamate (NMDA) receptor (NMDAR) antagonist; 0.25 or 2.5 mg/0.5 ml/hemisphere), PP2 (Src-family kinase inhibitor; 6.25 or 62.5 ng/0.5 ml/hemisphere), Ro25-6981 (NR2B subunit- containing NMDAR antagonist; 0.2 or 2 mg/0.5 ml/hemisphere), or vehicle administration into the DH. Administration of AP5, PP2, or Ro25-6981 into the DH dose-dependently impaired drug context-induced reinstatement of cocaine-seeking behavior relative to vehicle, without altering instrumental behavior in the extinction context or food-reinforced instrumental responding and general motor activity in control experiments. -

Estimating Your Air Consumption
10/29/2019 Alert Diver | Estimating Your Air Consumption Estimating Your Air Consumption Advanced Diving Public Safety Diving By Mike Ange Mastering Neutral Buoyancy and Trim Military Diving Technical Diving Scientific Diving and Safety Program Oversight Seeing the Reef in a New Light ADVERTISEMENT Do you have enough breathing gas to complete the next dive? Here's how to find out. It is a warm clear day, and the Atlantic Ocean is like glass. As you drop into the water for a dive on North Carolina's famous U-352 wreck, you can see that the :: captain has hooked the wreck very near the stern. It is your plan to circumnavigate the entire structure and get that perfect photograph near the exposed bow torpedo tube. You descend to slightly below 100 feet, reach the structure and take off toward the bow. Unfortunately, you are only halfway, just approaching the conning tower, when your buddy signals that he is running low on air. Putting safety first, you return with him to the ascent line — cursing the lost opportunity and vowing to find a new buddy. If you've ever experienced the disappointment of ending a dive too soon for lack of breathing gas or, worse, had to make a hurried ascent because you ran out of air, it may surprise you to learn that your predicament was entirely predictable. With a little planning and some basic calculations, you can estimate how much breathing gas you will need to complete a dive and then take steps to ensure an adequate supply. It's a process that technical divers live by and one that can also be applied to basic open-water diving. -

Performance Enhancement at the Cost of Potential Brain Plasticity: Neural Ramifications of Nootropic Drugs in the Healthy Developing Brain
REVIEW ARTICLE published: 13 May 2014 SYSTEMS NEUROSCIENCE doi: 10.3389/fnsys.2014.00038 Performance enhancement at the cost of potential brain plasticity: neural ramifications of nootropic drugs in the healthy developing brain Kimberly R. Urban 1 and Wen-Jun Gao 2* 1 Department of Psychology, University of Delaware, Newark, DE, USA 2 Department of Neurobiology and Anatomy, Drexel University College of Medicine, Philadelphia, PA, USA Edited by: Cognitive enhancement is perhaps one of the most intriguing and controversial Mikhail Lebedev, Duke University, topics in neuroscience today. Currently, the main classes of drugs used as potential USA cognitive enhancers include psychostimulants (methylphenidate (MPH), amphetamine), Reviewed by: Kimberly Simpson, University of but wakefulness-promoting agents (modafinil) and glutamate activators (ampakine) are Mississippi Medical Center, USA also frequently used. Pharmacologically, substances that enhance the components Christopher R. Madan, University of of the memory/learning circuits—dopamine, glutamate (neuronal excitation), and/or Alberta, Canada norepinephrine—stand to improve brain function in healthy individuals beyond their *Correspondence: baseline functioning. In particular, non-medical use of prescription stimulants such as Wen-Jun Gao, Department of Neurobiology and Anatomy, Drexel MPH and illicit use of psychostimulants for cognitive enhancement have seen a recent University College of Medicine, rise among teens and young adults in schools and college campuses. However, this 2900 Queen Lane, Philadelphia, PA enhancement likely comes with a neuronal, as well as ethical, cost. Altering glutamate 19129, USA function via the use of psychostimulants may impair behavioral flexibility, leading to e-mail: [email protected] the development and/or potentiation of addictive behaviors. Furthermore, dopamine and norepinephrine do not display linear effects; instead, their modulation of cognitive and neuronal function maps on an inverted-U curve. -
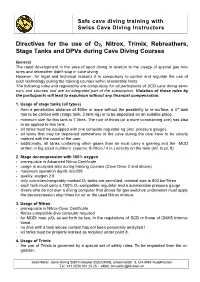
Directives for the Use of O 2, Nitrox, Trimix, Rebreathers, Stage Tanks
Safe cave diving training with Swiss Cave Diving Instructors Directives for the use o f O 2 , Nitrox, Trimix, Rebreathers, S tage Tanks and DPVs during Cave Diving Courses General The rapid development in the area of sport diving in relation to the u sage of special gas mi x- tures and rebreather didn't stop in cave diving. However, for legal and technical reasons it is compulsory to control and regulate the use of such tec h nology during the training courses within reasonable limits. The following rules a nd regulations are compulsory for all participants of SCD cave diving sem i- nars and courses and are an integrated part of the subscription. Violation of those rules by the participants will lead to expulsion without any financial compensation. 1. Usage of stage tanks (all types) - from a penetration distance of 500m or more without the possibility to re - surface, a 3 rd tank has to be carried with (stage tank, 3 tank rig) or to be deposited on an suitable place. - minimum size for this tank is 7 litres. The r ule of thirds (or a more constraining one) has also to be applied to this tank. - all tanks must be equipped with one complete regulator rig (incl. pressure gauge). - all tanks that may be deposited somewhere in the cave during the dive have to be clearly marked with the name of the user . - addition ally , a ll tanks containing other gases than air must carr y a gas - tag and the MOD written in big sized numbers (approx. -

Tinnitus Hopes Put to Sleep by Latest Auris Failure
March 14, 2018 Tinnitus hopes put to sleep by latest Auris failure Madeleine Armstrong Ketamine is best known as a horse tranquiliser or a recreational drug, but it has also been proposed as a treatment for various disorders from depression to Alzheimer’s. Hopes of developing the drug in tinnitus have been dashed by the failure of Auris’s Keyzilen in a second phase III trial. As well as leaving Auris’s future looking bleak – Keyzilen is the second of its phase III candidates to flunk in four months – the setback could also be bad news for the sparse tinnitus pipeline. According to EvaluatePharma there is only one other candidate in active clinical development, Otonomy’s OTO-313, and this uses the same mechanism of action as Keyzilen (see table below). Tinnitus pipeline Generic Project Company Pharma class Trial(s) Notes name Phase III Auris Esketamine TACTT2 Keyzilen NMDA antagonist Failed Aug 2016 Medical hydrochloride (NCT01803646) TACTT3 Failed Mar 2018 (NCT02040194) Phase I OTO- Phase I/II trial to OTO-311 abandoned in Otonomy NMDA antagonist Gacyclidine 313 start H1 2019 favour of this formulation Preclinical Auris AM-102 Undisclosed - - Medical KCNQ2 Knopp Kv7 potassium - - Program Biosciences channel modulator Source: EvaluatePharma. Both projects are psychoactive drugs targeting the NMDA receptor. Tinnitus is commonly caused by loud noise and resulting damage to the sensory hair cells in the cochlea. Initial trauma to the inner ear has been shown to trigger excess production of glutamate, which leads to the hyperactivation of NMDA receptors and, in turn, cell death. Blocking the NMDA receptor could therefore have a protective effect – but it is unclear how this mechanism would work once the damage to hair cells had been done. -

Underwater Photography Made Easy
Underwater Photography Made Easy Create amazing photos & video with by Annie Crawley IncludingIncluding highhigh definitiondefinition videovideo andand photophoto galleriesgalleries toto showshow youyou positioningpositioning andand bestbest techniques!techniques! BY ANNIE CRAWLEY SeaLife Cameras Perfect for every environment whether you are headed on a tropical vacation or diving the Puget Sound. These cameras meet all of your imaging needs! ©2013 Annie Crawley www.Sealife-cameras.com www.DiveIntoYourImagination.com Edmonds Underwater Park, Washington All rights reserved. This interactive book, or parts thereof, may not be reproduced in any form without permission in writing from the publisher, Dive Into Your Imagination, LLC a company founded by Annie Crawley committed to change the way a new generation views the Ocean and themselves. Dive Into Your Imagination, Reg. Pat. & Tm. Off. Underwater Photography Made Easy shows you how to take great photos and video with your SeaLife camera system. After our introduction to this interactive book you will learn: 1. Easy to apply tips and tricks to help you create great images. 2. Five quick review steps to make sure your SeaLife camera system is ready before every dive. 3. Neutral buoyancy tips to help you take great underwater photos & video with your SeaLife camera system. 4. Macro and wide angle photography and video basics including color, composition, understanding the rule of thirds, leading diagonals, foreground and background considerations, plus lighting with strobes and video lights. 5. Techniques for both temperate and tropical waters, how to photograph divers, fish behavior and interaction shots, the difference in capturing animal portraits versus recording action in video. You will learn how to capture sharks, turtles, dolphins, clownfish, plus so much more. -

General Anesthesia and Altered States of Arousal: a Systems Neuroscience Analysis
General Anesthesia and Altered States of Arousal: A Systems Neuroscience Analysis The MIT Faculty has made this article openly available. Please share how this access benefits you. Your story matters. Citation Brown, Emery N., Patrick L. Purdon, and Christa J. Van Dort. “General Anesthesia and Altered States of Arousal: A Systems Neuroscience Analysis.” Annual Review of Neuroscience 34, no. 1 (July 21, 2011): 601–628. As Published http://dx.doi.org/10.1146/annurev-neuro-060909-153200 Publisher Annual Reviews Version Author's final manuscript Citable link http://hdl.handle.net/1721.1/86331 Terms of Use Creative Commons Attribution-Noncommercial-Share Alike Detailed Terms http://creativecommons.org/licenses/by-nc-sa/4.0/ NIH Public Access Author Manuscript Annu Rev Neurosci. Author manuscript; available in PMC 2012 July 06. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: Annu Rev Neurosci. 2011 ; 34: 601–628. doi:10.1146/annurev-neuro-060909-153200. General Anesthesia and Altered States of Arousal: A Systems Neuroscience Analysis Emery N. Brown1,2,3, Patrick L. Purdon1,2, and Christa J. Van Dort1,2 Emery N. Brown: [email protected]; Patrick L. Purdon: [email protected]; Christa J. Van Dort: [email protected] 1Department of Anesthesia, Critical Care and Pain Medicine, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts 02114 2Department of Brain and Cognitive Sciences, Massachusetts Institute of Technology, Cambridge, Massachusetts 02139 3Harvard-MIT Division of Health Sciences and Technology, Massachusetts Institute of Technology, Cambridge, Massachusetts 02139 Abstract Placing a patient in a state of general anesthesia is crucial for safely and humanely performing most surgical and many nonsurgical procedures. -

(Tert- Butoxycarbonyl)Amino](3 361442- 3
Alternative Name CAS 1. Product Name Use Number 320345- 2. Aclidinium bromide API 99-1 (2S)-[(tert- Butoxycarbonyl)amino](3 361442- 3. Saxagliptin int -hydroxyadamant-1- 00-4 yl)ethanoic acid 1,3- 1,3- 5001-18- 4. Dihydroxyadamantane Adamantanediol 3 1,3-Dimethyladamantane 702-79-4 memantine intermediate 5. 1-Acetylamido-3,5- 19982- 6. Memantine int dimethyladamantane 07-1 1- 7. 880-52-4 Acetylaminoadamantane 1- 4942-47- 8. 1-Adamantaneacetic acid Adamantylacetic 6 acid [2-(1- 6240-11- 9. 1-Adamantaneethanol Adamantylethano 5 l)] 1- 10. 1-Adamantanemethanol Adamantylmetha 770-71-8 nol 1- 1660-04- 1-Adamantyl methyl rimantadine intermediate; 11. Acetyladamantan 4 ketone e 1-Chloro-3,5- 707-36-8 memantine intermediate; 12. dimethyladamantane 1-Hydroxy-3,5- memantine intermediate; 13. 707-37-9 dimethyladamantane 2- 14. 2-Adamantanol Hydroxyadamant 700-57-2 ane 15. 2-Adamantanone 700-58-3 2-Aminoadamantane 10523- 16. hydrochloride 68-9 3-Amino-1-hydroxy- 3-Amino-1- 702-82-9 vildagliptin intermediate; 17. adamantane adamantanol 3- 38584- 18. (Hydroxymethyl)adamant 37-1 -1-ol 19. 3-aminomethyl- 865887- mequitazine intermediate; 20. quinuclidine 14-5 dihydrochloride zacopride intermediate; 6530-09- mezacopride intermediate; 3-Aminoquinuclidine 21. 2 pancopride intermediate; dihydrochloride azasetron intermediate; 3-Carbethoxy-dehydro- quifenadine intermediate; 50790- 22. quinuclidine sequifenadine intermediate; 85-7 hydrochloride quifenadine intermediate; 3- 6238-33- 23. sequifenadine intermediate; Carbethoxyquinuclidine 1 3-hydroxymethyl 79221- mequitazine intermediate; 24. quinuclidine 75-3 hydrochloride 3-Quinuclidine 6238-34- 25. carboxylic acid 2 hydrochloride 1619-34- penehyclidine intermediate; 26. 3-Quinuclidinol 7 clidinium intermediate; cevimeline intermediate; 3-Quinuclidinone 1193-65- 27.