Eicosanoids and Exosomes: a Link Between Macrophages and Lung Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Eicosanoids in Carcinogenesis
4open 2019, 2,9 © B.L.D.M. Brücher and I.S. Jamall, Published by EDP Sciences 2019 https://doi.org/10.1051/fopen/2018008 Special issue: Disruption of homeostasis-induced signaling and crosstalk in the carcinogenesis paradigm “Epistemology of the origin of cancer” Available online at: Guest Editor: Obul R. Bandapalli www.4open-sciences.org REVIEW ARTICLE Eicosanoids in carcinogenesis Björn L.D.M. Brücher1,2,3,*, Ijaz S. Jamall1,2,4 1 Theodor-Billroth-Academy®, Germany, USA 2 INCORE, International Consortium of Research Excellence of the Theodor-Billroth-Academy®, Germany, USA 3 Department of Surgery, Carl-Thiem-Klinikum, Cottbus, Germany 4 Risk-Based Decisions Inc., Sacramento, CA, USA Received 21 March 2018, Accepted 16 December 2018 Abstract- - Inflammation is the body’s reaction to pathogenic (biological or chemical) stimuli and covers a burgeoning list of compounds and pathways that act in concert to maintain the health of the organism. Eicosanoids and related fatty acid derivatives can be formed from arachidonic acid and other polyenoic fatty acids via the cyclooxygenase and lipoxygenase pathways generating a variety of pro- and anti-inflammatory mediators, such as prostaglandins, leukotrienes, lipoxins, resolvins and others. The cytochrome P450 pathway leads to the formation of hydroxy fatty acids, such as 20-hydroxyeicosatetraenoic acid, and epoxy eicosanoids. Free radical reactions induced by reactive oxygen and/or nitrogen free radical species lead to oxygenated lipids such as isoprostanes or isolevuglandins which also exhibit pro-inflammatory activities. Eicosanoids and their metabolites play fundamental endocrine, autocrine and paracrine roles in both physiological and pathological signaling in various diseases. These molecules induce various unsaturated fatty acid dependent signaling pathways that influence crosstalk, alter cell–cell interactions, and result in a wide spectrum of cellular dysfunctions including those of the tissue microenvironment. -

Leukotriene D4induced Caco2 Cell Proliferation Is Mediated By
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Diposit Digital de la Universitat de Barcelona Physiological Reports ISSN 2051-817X ORIGINAL RESEARCH Leukotriene D4-induced Caco-2 cell proliferation is mediated by prostaglandin E2 synthesis Marisol Cabral, Raquel Martın-Venegas & Juan J. Moreno Departament de Fisiologia, Facultat de Farmacia, Universitat de Barcelona, Barcelona, Spain Keywords Abstract 5-lipoxygenase, arachidonic acid cascade, cell cycle, cell growth, colon cancer. Leukotriene D4 (LTD4) is a pro-inflammatory mediator formed from arachi- donic acid through the action of 5-lipoxygenase (5-LOX). Its biological effects Correspondence are mediated by at least two G-coupled plasmatic cysteinyl LT receptors (Cys- Juan Jose Moreno, Departament de LT1-2R). It has been reported an upregulation of the 5-LOX pathway in tumor Fisiologia, Facultat de Farmacia, Universitat tissue unlike in normal colon mucosa. Colon tumors generally have an de Barcelona, Avda. Joan XXIII s/n, 08028 increased expression of CysLT1R and colon cancer patients with high expres- Barcelona, Spain. sion levels of CysLT R have poor prognosis. We previously observed that the Tel: +34 93 402 4505 1 Fax: +34 93 403 5901 cyclooxygenase pathway is involved in the control of intestinal epithelial can- E-mail: [email protected] cer cell growth through PGE2 production. The aim of this study was therefore to assess the effect of LTD4 binding with CysLT1R on Caco-2 cell growth. We Funding Information note a number of key findings from this research. We observed that at a con- This research was supported by Spanish centration similar to that found under inflammatory conditions, LTD4 was Ministry of Science and Innovation (BFU2007- able to induce Caco-2 cell proliferation and DNA synthesis. -
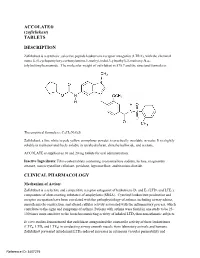
ACCOLATE® (Zafirlukast) TABLETS DESCRIPTION
ACCOLATE® (zafirlukast) TABLETS DESCRIPTION Zafirlukast is a synthetic, selective peptide leukotriene receptor antagonist (LTRA), with the chemical name 4-(5-cyclopentyloxy-carbonylamino-1-methyl-indol-3-ylmethyl)-3-methoxy-N-o tolylsulfonylbenzamide. The molecular weight of zafirlukast is 575.7 and the structural formula is: The empirical formula is: C31H33N3O6S Zafirlukast, a fine white to pale yellow amorphous powder, is practically insoluble in water. It is slightly soluble in methanol and freely soluble in tetrahydrofuran, dimethylsulfoxide, and acetone. ACCOLATE is supplied as 10 and 20 mg tablets for oral administration. Inactive Ingredients: Film-coated tablets containing croscarmellose sodium, lactose, magnesium stearate, microcrystalline cellulose, povidone, hypromellose, and titanium dioxide. CLINICAL PHARMACOLOGY Mechanism of Action: Zafirlukast is a selective and competitive receptor antagonist of leukotriene D4 and E4 (LTD4 and LTE4), components of slow-reacting substance of anaphylaxis (SRSA). Cysteinyl leukotriene production and receptor occupation have been correlated with the pathophysiology of asthma, including airway edema, smooth muscle constriction, and altered cellular activity associated with the inflammatory process, which contribute to the signs and symptoms of asthma. Patients with asthma were found in one study to be 25 100 times more sensitive to the bronchoconstricting activity of inhaled LTD4 than nonasthmatic subjects. In vitro studies demonstrated that zafirlukast antagonized the contractile activity of three leukotrienes (LTC4, LTD4 and LTE4) in conducting airway smooth muscle from laboratory animals and humans. Zafirlukast prevented intradermal LTD4-induced increases in cutaneous vascular permeability and Reference ID: 3407275 inhibited inhaled LTD4-induced influx of eosinophils into animal lungs. Inhalational challenge studies in sensitized sheep showed that zafirlukast suppressed the airway responses to antigen; this included both the early- and late-phase response and the nonspecific hyperresponsiveness. -

Montelukast, a Leukotriene Receptor Antagonist, Reduces the Concentration of Leukotrienes in the Respiratory Tract of Children with Persistent Asthma
Montelukast, a leukotriene receptor antagonist, reduces the concentration of leukotrienes in the respiratory tract of children with persistent asthma Benjamin Volovitz, MD,a,b Elvan Tabachnik, MD,c Moshe Nussinovitch, MD,b Biana Shtaif, MSc,b Hanna Blau, MD,a Irit Gil-Ad, PhD,b Abraham Weizman, MD,b and Itzhak Varsano, MDa,b Petah Tikva, Tel Aviv, and Rehovot, Israel Background: Leukotrienes are bronchoactive mediators secreted by inflammatory cells in the respiratory mucosa on Abbreviations used exposure to asthma triggers. BAL: Bronchoalveolar lavage Objective: We investigated the effect of montelukast, a CysLT1: Cysteinyl leukotriene 1 (receptor) leukotriene receptor antagonist, on the release of leukotrienes ECP: Eosinophilic cationic protein in the respiratory mucosa of children with persistent asthma. LTC4: Leukotriene C4 Method: Twenty-three children aged 6 to 11 years with moder- LTD4: Leukotriene D4 ately severe asthma were treated in a cross-over design start- LTE4: Leukotriene E4 ing, after a 2-week run in period, with either montelukast (n = 12) or cromolyn (n = 11) for 4 weeks with a 2-week washout period between treatments. Twelve of them were then treated Cysteinyl leukotrienes are potent proinflammatory with either montelukast or beclomethasone for 6 months. The mediators produced from a variety of inflammatory use of β -agonists was recorded on a diary card. The concen- 2 cells, including mast cells, eosinophils, basophils and tration of leukotriene C4 (LTC4) was measured by HPLC in nasal washes obtained before and at the end of each treatment macrophages. Leukotriene C4 (LTC4) is metabolized period. Eosinophilic cationic protein (ECP) was measured in enzymatically to leukotriene D4 (LTD4) and subsequent- the nasal washes by RIA. -
Effects of Maresin 1, an Omega-3 Fatty Acid-Derived Lipid Mediator, on Adipose Tissue and Liver Function in Obesity [Tesis Docto
Facultad de Farmacia y Nutrición Effects of Maresin 1, an omega-3 fatty acid-derived lipid mediator, on adipose tissue and liver function in obesity Efectos de Maresina 1, un mediador lipídico derivado de los ácidos grasos omega-3, en la función del tejido adiposo y el hígado en obesidad Laura Laiglesia González Pamplona, 2017 Facultad de Farmacia y Nutrición Memoria presentada por Dña. Laura Laiglesia González para aspirar al grado de Doctor por la Universidad de Navarra. Fdo. Laura Laiglesia González El presente trabajo ha sido realizado bajo nuestra dirección en el Departamento de Ciencias de la Alimentación y Fisiología de la Facultad de Farmacia y Nutrición de la Universidad de Navarra y autorizamos su presentación ante el Tribunal que lo ha de juzgar. VºBº Directora VºBº Co-Directora María Jesús Moreno Aliaga Silvia Lorente Cebrián Este trabajo ha sido posible gracias a la financiación de diversas entidades: Gobierno de España (Ministerio de Economía, Industria y Competitividad) [BFU2012-36089 y BFU2015-65937-R], Gobierno de Navarra (Departamento de Salud) [67-2015], Centro de Investigación Biomédica en Red de Fisiopatología de la Obesidad y Nutrición (CIBERObn) Instituto de Salud Carlos III (ISCIII) [CB12/03/30002], Centro de Investigación en Nutrición (Universidad de Navarra). Beca predoctoral 2013-2017: La investigación que ha dado lugar a estos resultados ha sido impulsada por la Obra Social "la Caixa” y la Asociación de Amigos de la Universidad de Navarra. Acknowledgements Me gustaría expresar mi agradecimiento a esas personas que han hecho posible la realización de este trabajo durante los últimos cuatro años, hasta aquellos que me han escuchado a pesar de no entender muy bien que es lo que estaba haciendo. -

Strict Regio-Specificity of Human Epithelial 15-Lipoxygenase-2
Strict Regio-specificity of Human Epithelial 15-Lipoxygenase-2 Delineates its Transcellular Synthesis Potential Abigail R. Green, Shannon Barbour, Thomas Horn, Jose Carlos, Jevgenij A. Raskatov, Theodore R. Holman* Department Chemistry and Biochemistry, University of California Santa Cruz, 1156 High Street, Santa Cruz CA 95064, USA *Corresponding author: Tel: 831-459-5884. Email: [email protected] FUNDING: This work was supported by the NIH NS081180 and GM56062. Abbreviations: LOX, lipoxygenase; h15-LOX-2, human epithelial 15-lipoxygenase-2; h15-LOX-1, human reticulocyte 15-lipoxygenase-1; sLO-1, soybean lipoxygenase-1; 5-LOX, leukocyte 5-lipoxygenase; 12-LOX, human platelet 12-lipoxygenase; GP, glutathione peroxidase; AA, arachidonic acid; HETE, hydoxy-eicosatetraenoic acid; HPETE, hydroperoxy-eicosatetraenoic acid; diHETEs, dihydroxy-eicosatetraenoic acids; 5-HETE, 5-hydroxy-6E,8Z,11Z,14Z-eicosatetraenoic acid; 5-HPETE, 5-hydro peroxy-6E,8Z,11Z,14Z-eicosatetraenoic acid; 12-HPETE, 12-hydroperoxy-5Z,8Z,10E, 14Z-eicosatetraenoic acid; 15-HPETE, 15-hydroperoxy-5Z,8Z,10Z,13E- eicosatetraenoic acid; 5,15-HETE, 5S,15S-dihydroxy-6E,8Z,10Z,13E-eicosatetraenoic acid; 5,15-diHPETE, 5,15-dihydroperoxy-6E,8Z,10Z,13E-eicosatetraenoic acid; 5,6- diHETE, 5S,6R-dihydroxy-7E,9E,11Z,14Z-eicosatetraenoic acid; LTA4, 5S-trans-5,6- oxido-7E,9E,11Z,14Z-eicosatetraenoic acid; LTB4, 5S,12R-dihydroxy-6Z,8E,10E,14Z- eicosatetraenoic acid; LipoxinA4 (LxA4), 5S,6R,15S-trihydroxy-7E,9E,11Z,13E- eicosatetraenoic acid; LipoxinB4 (LxB4), 5S,14R,15S-trihydroxy-6E,8Z,10E,12E- eicosatetraenoic acid. Abstract Lipoxins are an important class of lipid mediators that induce the resolution of inflammation, and arise from transcellular exchange of arachidonic acid (AA)- derived lipoxygenase products. -

Maresin 1 Biosynthesis During Platelet–Neutrophil Interactions Is Organ-Protective
Maresin 1 biosynthesis during platelet–neutrophil interactions is organ-protective Raja-Elie E. Abdulnoura,1, Jesmond Dallib,1, Jennifer K. Colbya, Nandini Krishnamoorthya, Jack Y. Timmonsa, Sook Hwa Tana, Romain A. Colasb, Nicos A. Petasisc, Charles N. Serhanb, and Bruce D. Levya,b,2 aPulmonary and Critical Care Medicine and bCenter for Experimental Therapeutics and Reperfusion Injury, Department of Anesthesiology, Perioperative and Pain Medicine, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA 02115; and cDepartment of Chemistry, University of Southern California, Los Angeles, CA 90089 Edited by Derek William Gilroy, University College London, London, United Kingdom, and accepted by the Editorial Board October 10, 2014 (received for review April 17, 2014) Unregulated acute inflammation can lead to collateral tissue injury 12-lipoxygenase that may be capable of generating the 13S,14S- in vital organs, such as the lung during the acute respiratory distress epoxy-maresin intermediate and participating in MaR1 production syndrome. In response to tissue injury, circulating platelet–neutro- at sites of vascular inflammation. Here, we provide evidence for phil aggregates form to augment neutrophil tissue entry. These a MaR1 biosynthetic route during platelet–neutrophil interactions early cellular events in acute inflammation are pivotal to timely that is operative in vivo in a murine model of ARDS to restrain resolution by mechanisms that remain to be elucidated. Here, we inflammation and restore homeostasis of the injured lung. identified a previously undescribed biosynthetic route during hu- man platelet–neutrophil interactions for the proresolving mediator Results maresin 1 (MaR1; 7R,14S-dihydroxy-docosa-4Z,8E,10E,12Z,16Z,19Z- To determine if platelets can participate in vascular MaR1 bio- hexaenoic acid). -

Therapeutic Effects of Specialized Pro-Resolving Lipids Mediators On
antioxidants Review Therapeutic Effects of Specialized Pro-Resolving Lipids Mediators on Cardiac Fibrosis via NRF2 Activation 1, 1,2, 2, Gyeoung Jin Kang y, Eun Ji Kim y and Chang Hoon Lee * 1 Lillehei Heart Institute, University of Minnesota, Minneapolis, MN 55455, USA; [email protected] (G.J.K.); [email protected] (E.J.K.) 2 College of Pharmacy, Dongguk University, Seoul 04620, Korea * Correspondence: [email protected]; Tel.: +82-31-961-5213 Equally contributed. y Received: 11 November 2020; Accepted: 9 December 2020; Published: 10 December 2020 Abstract: Heart disease is the number one mortality disease in the world. In particular, cardiac fibrosis is considered as a major factor causing myocardial infarction and heart failure. In particular, oxidative stress is a major cause of heart fibrosis. In order to control such oxidative stress, the importance of nuclear factor erythropoietin 2 related factor 2 (NRF2) has recently been highlighted. In this review, we will discuss the activation of NRF2 by docosahexanoic acid (DHA), eicosapentaenoic acid (EPA), and the specialized pro-resolving lipid mediators (SPMs) derived from polyunsaturated lipids, including DHA and EPA. Additionally, we will discuss their effects on cardiac fibrosis via NRF2 activation. Keywords: cardiac fibrosis; NRF2; lipoxins; resolvins; maresins; neuroprotectins 1. Introduction Cardiovascular disease is the leading cause of death worldwide [1]. Cardiac fibrosis is a major factor leading to the progression of myocardial infarction and heart failure [2]. Cardiac fibrosis is characterized by the net accumulation of extracellular matrix proteins in the cardiac stroma and ultimately impairs cardiac function [3]. Therefore, interest in substances with cardioprotective activity continues. -

Supplementary Information Optimization of a Method For
Supplementary Information Optimization of a method for the simultaneous extraction of polar and non-polar oxylipin metabolites, DNA, RNA, small RNA, and protein from a single small tissue sample Yu Hasegawa, Yurika Otoki, Shannon McClorry, Laurynne C. Coates, Rachel L. Lombardi, Ameer Y. Taha, Carolyn M. Slupsky Procedure for Methods A and B For Methods A and B, the following steps were modified: 3.1. Preparation of Reagents 1. Prepare chloroform:methanol (2:1) with 0.002% BHT [Solution 1]. Pre-chill in a -20 °C freezer. 2. Prepare 1 mM EDTA dissolved in Type I water [Solution 2]. Pre-chill to 4 °C. 3. Prepare chloroform:methanol (10:1) [Solution 3]. Pre-chill in a -20 °C freezer. 3.3. Metabolite Extraction 3.3.1. Method A 1. Add 1600 µL of chloroform, 800 µL of methanol, and 600 µL of Type I ultrapure water to tubes with ground brain tissue and mix by vortexing for 20 seconds. 2. Centrifuge the tubes for 15 min at 2,000 rpm at 0 °C to separate the sample into three layers. 3. Collect the upper layer into a new 15 mL conical centrifuge tube. Do not disturb the cell layer. Keep the tube on ice and proceed to step 22. 4. Using a 9-inch glass Pasteur pipette, collect the bottom layer and place in a new 8 mL glass tube. Place the tube on ice and proceed to step 31. 5. Proceed to step 42 to process the middle layer. 3.3.2. Method B 1. Add 2.4 mL of cold Solution 1 into the 8 mL glass tube with the cryoground tissue. -

Maresin 1 Promotes Inflammatory Resolution, Neuroprotection and Functional Neurological Recovery After Spinal Cord Injury
This Accepted Manuscript has not been copyedited and formatted. The final version may differ from this version. Research Articles: Development/Plasticity/Repair Maresin 1 promotes inflammatory resolution, neuroprotection and functional neurological recovery after spinal cord injury Isaac Francos Quijorna1, Eva Santos-Nogueira1, Karsten Gronert2, Aaron B. Sullivan2, Marcel A Kopp3, Benedikt Brommer3,4, Samuel David5, Jan M. Schwab3,6,7 and Ruben Lopez Vales1 1Departament de Biologia Cel·lular, Fisiologia i Immunologia, Institut de Neurociències, Centro de Investigación Biomédica en Red sobre Enfermedades Neurodegenerativas (CIBERNED), Universitat Autònoma de Barcelona, 08193 Bellaterra, Catalonia Spain 2Vision Science Program, School of Optometry, University of California Berkeley, Berkeley, CA 94598, USA 3Spinal Cord Alliance Berlin (SCAB) and Department of Neurology and Experimental Neurology, Charité Campus Mitte, Clinical and Experimental Spinal Cord Injury Research Laboratory (Neuroparaplegiology), Charité-Universitätsmedizin Berlin, Berlin, Germany 4F.M. Kirby Neurobiology Center, Boston Children's Hospital, and Department of Neurology, Harvard Medical School, 300 Longwood Avenue, Boston, MA 02115, USA 5Centre for Research in Neuroscience, The Research Institute of the McGill University Health Centre, Montreal, Canada 6Department of Neurology, Spinal Cord Injury Division, The Neurological Institute, The Ohio State University, Wexner Medical Centre, Columbus, OH 43210, USA 7Department of Neuroscience and Center for Brain and Spinal Cord Repair, Department of Physical Medicine and Rehabilitation, The Neurological Institute, The Ohio State University, Wexner Medical Centre, Columbus, OH 43210, USA. DOI: 10.1523/JNEUROSCI.1395-17.2017 Received: 22 May 2017 Revised: 27 September 2017 Accepted: 1 October 2017 Published: 3 November 2017 Author contributions: I.F.Q., J.S., and R.L.-V. -
Inflammation, Cancer and Oxidative Lipoxygenase Activity Are Intimately Linked
Cancers 2014, 6, 1500-1521; doi:10.3390/cancers6031500 OPEN ACCESS cancers ISSN 2072-6694 www.mdpi.com/journal/cancers Review Inflammation, Cancer and Oxidative Lipoxygenase Activity are Intimately Linked Rosalina Wisastra and Frank J. Dekker * Pharmaceutical Gene Modulation, Groningen Research Institute of Pharmacy, University of Groningen, Antonius Deusinglaan 1, 9713 AV Groningen, The Netherlands; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +31-5-3638030; Fax: +31-5-3637953. Received: 16 April 2014; in revised form: 27 June 2014 / Accepted: 2 July 2014 / Published: 17 July 2014 Abstract: Cancer and inflammation are intimately linked due to specific oxidative processes in the tumor microenvironment. Lipoxygenases are a versatile class of oxidative enzymes involved in arachidonic acid metabolism. An increasing number of arachidonic acid metabolites is being discovered and apart from their classically recognized pro-inflammatory effects, anti-inflammatory effects are also being described in recent years. Interestingly, these lipid mediators are involved in activation of pro-inflammatory signal transduction pathways such as the nuclear factor κB (NF-κB) pathway, which illustrates the intimate link between lipid signaling and transcription factor activation. The identification of the role of arachidonic acid metabolites in several inflammatory diseases led to a significant drug discovery effort around arachidonic acid metabolizing enzymes. However, to date success in this area has been limited. This might be attributed to the lack of selectivity of the developed inhibitors and to a lack of detailed understanding of the functional roles of arachidonic acid metabolites in inflammatory responses and cancer. -

Maresin 1 Activates LGR6 Receptor Promoting Phagocyte Immunoresolvent Functions
Maresin 1 activates LGR6 receptor promoting phagocyte immunoresolvent functions Nan Chiang, … , Xavier de la Rosa, Charles N. Serhan J Clin Invest. 2019;129(12):5294-5311. https://doi.org/10.1172/JCI129448. Research Article Inflammation Graphical abstract Find the latest version: https://jci.me/129448/pdf RESEARCH ARTICLE The Journal of Clinical Investigation Maresin 1 activates LGR6 receptor promoting phagocyte immunoresolvent functions Nan Chiang, Stephania Libreros, Paul C. Norris, Xavier de la Rosa, and Charles N. Serhan Center for Experimental Therapeutics and Reperfusion Injury, Department of Anesthesiology, Perioperative and Pain Medicine, Brigham and Women’s Hospital and Harvard Medical School, Boston, Massachusetts, USA. Resolution of acute inflammation is an active process orchestrated by endogenous mediators and mechanisms pivotal in host defense and homeostasis. The macrophage mediator in resolving inflammation, maresin 1 (MaR1), is a potent immunoresolvent, stimulating resolution of acute inflammation and organ protection. Using an unbiased screening of greater than 200 GPCRs, we identified MaR1 as a stereoselective activator for human leucine-rich repeat containing G protein–coupled receptor 6 (LGR6), expressed in phagocytes. MaR1 specificity for recombinant human LGR6 activation was established using reporter cells expressing LGR6 and functional impedance sensing. MaR1-specific binding to LGR6 was confirmed using 3H-labeled MaR1. With human and mouse phagocytes, MaR1 (0.01–10 nM) enhanced phagocytosis, efferocytosis, and phosphorylation of a panel of proteins including the ERK and cAMP response element-binding protein. These MaR1 actions were significantly amplified with LGR6 overexpression and diminished by gene silencing in phagocytes. Thus, we provide evidence for MaR1 as an endogenous activator of human LGR6 and a novel role of LGR6 in stimulating MaR1’s key proresolving functions of phagocytes.