Living with Low Vision: How You Can Help
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Protocol P-321-202
Clinical Protocol P-321-202 Project Number P-1003-I101 Compound Number/ Name P-321 Ophthalmic Solution Protocol Number P-321-202 Protocol Title Randomized, Double-Masked, Parallel Group Study of P-321 Ophthalmic Solution Compared to Placebo in Subjects with Dry Eye Disease Assessing Safety and Efficacy Over 28 Days Sponsor Parion Sciences, Inc. 2800 Meridian Parkway Suite 195 Durham, NC 27713 Medical Monitor Authors Issue Date Original: Version 1.0 released 29 April 2016 Amendment 1.0: Version 2.0 Released 10 February 2017 Sponsor Signature and Date _____________________________________________ The information in this document is confidential and is provided to you as an investigator or consultant for review by you, your staff, and the applicable Institutional Review Board/Independent Ethics Committee. Your acceptance of this document constitutes agreement that you will not disclose the information contained herein to others without written authorization from Parion Sciences. Parion Sciences, Inc. P-321 Ophthalmic Solution Protocol P-321-202 Amendment 01 PARION SCIENCES, INC. Clinical Protocol P-321-202 Investigator Signature Page Project Number P-1003-I101 Compound Number/ Name P-321 Ophthalmic Solution Protocol Number P-321-202 Protocol Title Randomized, Double-Masked, Parallel Group Study of P - 321 Ophthalmic Solution Compared to Placebo in Subjects with Dry Eye Disease Assessing Safety and Efficacy Over 28 Days Sponsor Parion Sciences, Inc. 2800 Meridian Parkway Suite 195 Durham, NC 27713 Issue Date Original: Version 1.0 released 29 April 2016 Amendment 1.0: Version 2.0: Released 10 February 2017 I have reviewed and understand this protocol and all amendments associated with it. -
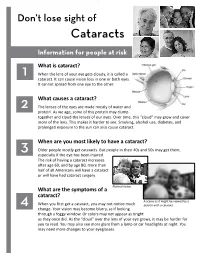
Don't Lose Sight of Cataract
Don’t lose sight of Cataracts Information for people at risk What is cataract? 1 When the lens of your eye gets cloudy, it is called a cataract. It can cause vision loss in one or both eyes. It cannot spread from one eye to the other. What causes a cataract? 2 The lenses of the eyes are made mostly of water and protein. As we age, some of this protein may clump together and cloud the lenses of our eyes. Over time, this “cloud” may grow and cover more of the lens. This makes it harder to see. Smoking, alcohol use, diabetes, and prolonged exposure to the sun can also cause cataract. When are you most likely to have a cataract? 3 Older people mostly get cataracts. But people in their 40s and 50s may get them, especially if the eye has been injured. The risk of having a cataract increases after age 60, and by age 80, more than half of all Americans will have a cataract or will have had cataract surgery. Normal vision. What are the symptoms of a cataract? A scene as it might be viewed by a 4 When you first get a cataract, you may not notice much person with a cataract. change. Your vision may become blurry, as if looking through a foggy window. Or colors may not appear as bright as they once did. As the “cloud” over the lens of your eye grows, it may be harder for you to read. You may also see more glare from a lamp or car headlights at night. -

National Institutes of Health
Trusted Health Information from the National Institutes of Health ® MedlineNIHFall 2011 Plusthe magazine Plus, in this issue! • Controlling High Blood Pressure Young adults at risk • Managing Asthma Actress Turning discovery Debra Winger into health “Everyone is touched • Millions by addiction...” Untreated Get tested for peripheral Speaking out for artery disease Drug Abuse Education A publication of the NATIONAL INSTITUTES OF HEALTH and the FRIE NDS of the NATIONAL LIBRARY OF MEDICINE FRIENDS OF THE NATIONAL LIBRARY OF MEDICINE 2011 Awards Gala Celebrating Leadership in Health and Medicine & 175th Anniversary of the National Library of Medicine Thursday, November 3, 2011 6:30 – 9:30 PM Great Hall, Jefferson Building Library of Congress Photo: NLM Photo: Washington, DC Donald West King, M.D. FNLM Chairman Photo: LibraryPhoto: of Congress t is an honor and pleasure each year for the Friends to hold an Awards Gala to celebrate the For more information advancements made in public health, medicine, and health communications, along with the on how to attend, visit individuals and organizations who are dedicated to this cause. The 2011 Annual Awards Gala on November 3 will bring together representatives from the public, professional, and business sectors in www.fnlm.org or call Ihealth care to show their support for the Library—this year celebrating its 175th anniversary. 202-679-9930. For their achievements and support of the advancement of health, five recipients will be honored: n Distinguished Medical Informatics Award Larry Ellison, Founder and CEO, Oracle n Paul G. Rogers Health Communications Award Mehmet Oz, MD, and Michael Roizen, MD, co-authors, YOU: The Owner’s Manual Let Us Hear From You! n Distinguished Medical Science Award Purnell W. -

Incorporating Sex As Biologic Variable to Advance Health
Connors-BRI Symposium: Incorporating Sex as Biologic Variable to Advance Health Monday, May 24th, 2021 3:00 - 5:00PM ET || Virtual AGENDA Welcoming Remarks Hadine Joffe, MD, MSc 3:00PM Executive Director, Mary Horrigan Connors Center for Women’s Health and Gender Biology Paula A. Johnson Professor of Psychiatry in the Field of Women’s Health Vice Chair for Research, Department of Psychiatry Brigham and Women’s Hospital / Harvard Medical School INTRODUCTION BY: Keynote Address 3:05PM Kathryn Rexrode, MD, MPH Chief, Division of Women’s Health, Department of Medicine Associate Professor of Medicine Brigham and Women’s Hospital / Harvard Medical School KEYNOTE: Why Studying Sex and Gender is Square One Janine Austin Clayton, MD Associate Director for Research on Women’s Health Director of the Office of Research on Women’s Health National Institutes of Health Featured Short Talks INTRODUCTION BY: 3:45PM Laura M. Holsen, MS, PhD Associate Psychologist Assistant Professor of Psychiatry Brigham and Women’s Hospital / Harvard Medical School SHORT TALKS BY: Sexual dimorphism in genetic associations of testosterone and sex-hormone binding globulin with coronary heart disease Jie Hu, MD, PhD, Brigham and Women’s Hospital Network medicine approaches reveal sex differences in lung cancer gene regulation Camila Lopes-Ramos, PhD, Harvard TH Chan School of Public Health Plasma glycated CD59 (pGCD59) accurately predicts early gestational diabetes (GDM) Michelle Toth-Castillo, BSc, Brigham and Women’s Hospital INTRODUCTION BY: 4:20PM Lightning Talks P. Emanuela Voinescu, MD, PhD Assistant Professor of Neurology Brigham and Women’s Hospital / Harvard Medical School Dawn L. DeMeo, MD, MPH Closing Remarks 4:50PM Associate Professor of Medicine Brigham and Women’s Hospital / Harvard Medical School KEYNOTE SPEAKER Janine Austin Clayton, M.D. -

Pilot Phase I/II Study of the Evaluation of Interferon Gamma-1B
RCD ESCS May 27, 2016 Protocol Title: Pilot Phase I/II Study of the Evaluation of Interferon Gamma-1b Administered Topically for Macular Edema/Intraretinal Schisis Cysts in Rod-Cone Dystrophy (RCD) and Enhanced S-Cone Syndrome (ESCS) Protocol Number: 15-EI-0052 Date of This Submission/Version: May 27, 2016/ v5.0 Principal Investigator (PI) Bldg. 10, Wadih Zein, MD NEI/NIH 301-496-8118 [email protected] Rm. 10D45 Accountable Investigator Bldg. 10, Wadih Zein, MD NEI/NIH 301-496-8118 [email protected] Rm. 10D45 Associate Investigators (AI) Bldg. 10, Catherine Cukras, MD, PhD NEI/NIH 301-435-5061 [email protected] Rm. 10C438 Bldg. 10, Brett Jeffrey, PhD NEI/NIH 301-402-2391 [email protected] Rm. 10C442 Bldg. 10, Emily Chew, MD NEI/NIH 301-496-6583 [email protected] Rm. 3-2531 Bldg. 10, Amy Turriff, ScM NEI/NIH 301-402-4175 [email protected] Rm. 11C432B Bldg. 10, Henry Wiley, MD NEI/NIH 301-451-4260 [email protected] Rm. 10D45 Bldg. 6, Wai T. Wong, MD, PhD NEINIH 301-496-7566 [email protected] Rm. 217 Bldg. 10, Brian Brooks, MD, PhD NEI/NIH 301-451-2238 [email protected] Room 10B16 Bldg. 35, Kapil Bharti, PhD NEI/NIH 301-496-9661 [email protected] Rm. 2A-102 Bldg. 6, Anand Swaroop, PhD NEI/NIH 301-435-5754 [email protected] Rm. 338 Bldg. 10, Arvydas Maminishkis, PhD NEI/NIH 301-435-4902 [email protected] Rm. 10B04 Bldg. 31, Sheldon Miller, PhD NEI/NIH 301-496-3180 [email protected] Rm. -

Departments of Labor, Health and Human Services, and Education, and Related Agencies Appropriations for Fiscal Year 2014
DEPARTMENTS OF LABOR, HEALTH AND HUMAN SERVICES, AND EDUCATION, AND RELATED AGENCIES APPROPRIATIONS FOR FISCAL YEAR 2014 WEDNESDAY, APRIL 2, 2014 U.S. SENATE, SUBCOMMITTEE OF THE COMMITTEE ON APPROPRIATIONS, Washington, DC. The subcommittee met at 10 a.m., in room SD–192, Dirksen Sen- ate Office Building, Hon. Tom Harkin (chairman) presiding. Present: Senators Harkin, Durbin, Mikulski, Moran, Cochran, Shelby, and Kirk. DEPARTMENT OF HEALTH AND HUMAN SERVICES NATIONAL INSTITUTES OF HEALTH STATEMENT OF FRANCIS S. COLLINS, M.D., PH.D., DIRECTOR ACCOMPANIED BY: ANTHONY S. FAUCI, M.D., DIRECTOR, NATIONAL INSTITUTE OF AL- LERGY AND INFECTIOUS DISEASES HAROLD E. VARMUS, M.D., DIRECTOR, NATIONAL CANCER INSTI- TUTE GARY H. GIBBONS, M.D., DIRECTOR, NATIONAL HEART, LUNG AND BLOOD INSTITUTE STORY C. LANDIS, PH.D., DIRECTOR, NATIONAL INSTITUTE OF NEUROLOGICAL DISORDERS AND STROKE CHRISTOPHER P. AUSTIN, M.D., DIRECTOR, NATIONAL CENTER FOR ADVANCING TRANSLATIONAL SCIENCES OPENING STATEMENT OF SENATOR TOM HARKIN Senator HARKIN. The Appropriations Subcommittee on Labor, Health and Human Services, and Education, and Related Agencies will come to order. Good morning, everyone, and welcome. Sorry we are a little late. We had a vote at 10—that is all. Well, today will be my final Appropriations budget hearing for the NIH (National Institutes of Health) as the chair of this sub- committee. I took over this subcommittee from Senator Lawton Chiles in 1989. That is a long time ago it seems, a quarter century. I am so proud of all that we have done—all of us here—often on a bipartisan basis, to transform the National Institutes of Health into truly the jewel and the crown of biomedical research not only in the United States, but globally. -

The National Institutes of Health (NIH): Background and Congressional Issues
The National Institutes of Health (NIH): Background and Congressional Issues Updated April 19, 2019 Congressional Research Service https://crsreports.congress.gov R41705 SUMMARY R41705 The National Institutes of Health (NIH): April 19, 2019 Background and Congressional Issues Judith A. Johnson The National Institutes of Health (NIH), under the Department of Health and Human Specialist in Biomedical Services (HHS), is the primary federal agency charged with performing and supporting Policy biomedical and behavioral research. In FY2018, NIH used its over $34 billion budget to support more than 300,000 scientists and research personnel working at over 2,500 Kavya Sekar institutions across the United States and abroad, as well as to conduct biomedical and Analyst in Health Policy behavioral research and research training at its own facilities. The agency consists of the Office of the Director, in charge of overall policy and program coordination, and 27 institutes and centers, each of which focuses on particular diseases or research areas in human health. A broad range of research is funded through a highly competitive system of peer-reviewed grants and contracts. The Public Health Service Act (PHSA) provides the statutory basis for NIH programs, and funding levels are mostly provided through the annual appropriations process. In December 2016, Congress introduced major reforms and programs at the NIH through the 21st Century Cures Act (P.L. 114-255). Prior to 2016, the last time Congress addressed NIH with comprehensive legislation was in December 2006, when it passed the NIH Reform Act (P.L. 109-482). Congress also gives direction to NIH through appropriations report language, but usually not through budget line items or earmarks. -

NEI 50 Years of Advance in Vision Research
NEI: 50 years of advances in vision research 1 From the director The National Eye Institute was established by Congress in 1968 with an urgent mission: to protect and prolong vision. At the time, millions of Americans were going blind from common eye diseases and facing isolation and a diminished quality of life. Over the past 50 years, public investment in vision research has paid remarkable dividends. Research supported by NEI and conducted at medical centers, universities, and other institutions across the country and around the world—as well as in laboratory and clinical settings at the National Institutes of Health—has led to breakthrough discoveries and treatments. Today, many eye diseases can be treated with sight-saving therapies that stabilize or even reverse vision loss. NEI-supported advances have led to major improvements in the treatment of glaucoma, uveitis, retinopathy of prematurity, and childhood amblyopia. We have more effective treatments and preventive strategies for age-related macular degeneration and diabetic retinopathy. Recent successes in gene therapy and regenerative medicine suggest the future looks even brighter for both rare and common eye diseases. Basic research has revealed new insights about the structure and function of the eye, which also offers a unique window into the brain. In fact, much of what we know about how the brain works comes from studies of the retina. Decades of NEI research on retinal cells has led to fundamental discoveries about how one nerve cell communicates with another, how sets of cells organize into circuits that process different kinds of sensory information, and how neural tissue develops and organizes itself. -

Diabetic Eye Disease Projected to Increase Among U.S. Population—Disease Will Reach 11 Million People by 2030
Diabetic Eye Disease Projected To Increase Among U.S. Population Disease will reach 11 million people by 2030 Today, diabetes affects more than 29 million people in the United States or over 9 percent of the population. In addition, another 86 million American adults, more than one out of three individuals, have pre-diabetes, a condition that puts people at increased risk for diabetes. All people with diabetes, type 1 and type 2, are at risk for diabetic eye disease, a leading cause of vision loss and blindness. Diabetic eye disease refers to a group of eye problems that people with diabetes may face as a complication of the disease and includes cataract, diabetic retinopathy, and glaucoma. Diabetic retinopathy, the most common form of diabetic eye disease, is the leading cause of blindness in adults 20–74 years of age. According to the National Eye Institute (NEI), 7.7 million people age 40 and older have diabetic retinopathy, and this number is projected to increase to approximately 11 million people by 2030. “The longer a person has diabetes, the greater is his or her risk of developing diabetic eye disease,” said Paul A. Sieving, M.D., Ph.D., director of NEI. “If you have diabetes, be sure to have a comprehensive dilated eye exam at least once a year. Diabetic eye disease often has no early warning signs, but can be detected early and treated before vision loss occurs. Don’t wait until you notice an eye problem to have a dilated eye exam, because vision that is lost often cannot be restored.” While all people with diabetes can develop diabetic eye disease, African Americans, American Indians/Alaska Natives, and Hispanics/Latinos with diabetes are at higher risk of losing vision or going blind from it. -

2015 Statutory Report.Pdf
May 27, 2016 Francis S. Collins, M.D., Ph.D. Director National Institutes of Health Building 1 Room 26 Bethesda, MD 20814 Dear Dr. Collins: Per statutory requirement, enclosed you will find the 2015 FNIH Annual Report to NIH. The report is comprised of the following: • Brief FNIH overview • 2015 Allocation of NIH’s Statutory Contribution to the FNIH • 2015 Operating Revenues and Expenses • 2015 Program Revenues and Expenses • FNIH Board of Directors • 2015 NIH Proposal Review Committee Submissions to FNIH • FNIH Project Summaries through December 31, 2015 • 2015 Financial Statements and Independent Auditor Letter • 2015 FNIH Summary Annual Report You will find the first eight items together in the spiral bound booklet. The 2015 FNIH Summary Annual Report is a separate document included in the package. Please do not hesitate to contact me if you have any questions. Sincerely yours, Maria C. Freire, Ph.D. President and Executive Director cc: Steven M. Paul, M.D., Chairman 2015 Annual Report to the National Institutes of Health May 27, 2016 Table of Contents Tab One ………………………………………………….….….….….….………….Brief FNIH Overview Tab Two……………………………………..2015 Allocation of NIH’s Statutory Contribution to the FNIH Tab Three…..………………….……………………………………2015 Operating Revenues and Expenses Tab Four……………….……….………………………………....….2015 Program Revenues and Expenses Tab Five…..……………….………………………………………………………FNIH Board of Directors Tab Six……………………………………….2015 NIH Proposal Review Committee Submissions to FNIH Tab Seven…..………………...………………………FNIH Project Summaries through December 31, 2015 Tab Eight…………….……………....….2015 Financial Statements and Report of the Independent Auditors Enclosure…..…………………………………………………..………2015 FNIH Summary Annual Report The Foundation for the National Institutes of Health organizes productive research collaborations, incubates new research models and channels resources for maximum impact in order to support the mission of the National Institutes of Health, the largest biomedical research agency in the world, as it works to turn discovery into health. -
It's Time to Celebrate Your Doctor Corneal Transplant Patients
It's time to Celebrate Your Doctor Subscribers to NKCF Update can send a special THANK YOU to their favorite eye doctor before March 30. Share the story of how your optometrist or ophthalmologist makes a difference in your life. NKCF will send your doctor a special message on your behalf on Honor Your Doctor Day. Check our next newsletter for a list of all doctors nominated and our choice for Top Docs of 2021. Submit a Top Doc Nomination! Corneal Transplant Patients & COVID-19 This past year has presented a host of challenges, particularly for those with existing health concerns. A portion of individuals with severe keratoconus undergo one or more corneal transplants when options like specialized contact lenses can no longer help achieve the best possible vision. In the age of coronavirus, two common questions arise: Are individuals with corneal transplants at greater risk for contracting COVID-19? And, is it safe for someone with a corneal transplant to get the COVID-19 vaccine? Dr. Christopher Sales, MD, MPH, Associate Professor of Ophthalmology at the University of Iowa reports that, “The average corneal transplant recipient is not at increased risk for contracting COVID-19 because of their use of steroid eye drops.” Eye surgeons will normally prescribe maintenance eyedrops for several months or even years after corneal transplant surgery to decrease the unlikely rejection of donor tissue. The drops concentrate their effect within the eye and do not have the same result that a medication designed to offer systemic (or body-wide) suppression would provide a patient who has had a transplant where the organ shares a blood supply like a heart, kidney, or liver. -

Deciphering NIH Application/Grant Numbers
Deciphering NIH Application/Grant Numbers Application Type Activity Code Institute Code (IC) Serial Number Support Year Other Suffixes 1 R01 CA 654321 01 A1 Application Types NIH Funding Institutes 1=New Request for support of a project that has not yet been funded. Acronym Full Name Code FIC John E. Fogarty International Center TW 2=Renewal Request for additional funding for a period subsequent to that provided by a current award. NCATS National Center for Advancing Translational Sciences (NCATS) TR NCCIH National Center for Complementary and Integrative Health AT 3=Revision Request for (or the award of) additional funds during a current project period to support new or additional activities that are not NCI National Cancer Institute CA identified in the current award. This request reflects an expansion of NEI National Eye Institute EY the scope of the grant‐approved activities. Competitive revisions NHGRI National Human Genome Research Institute HG require peer review. NHLBI National Heart, Lung, and Blood Institute HL An administrative supplement is a request for (or the award of) NIA National Institute on Aging AG additional funds during a current project period to provide for an increase in costs due to unforeseen circumstances. All additional NIAAA National Institute on Alcohol Abuse and Alcoholism AA costs must be within the scope of the peer reviewed and approved NIAID National Institute of Allergy and Infectious Diseases AI project. NIAMS National Institute of Arthritis and Musculoskeletal and Skin AR 4=Extension Request for additional years of support beyond the years previously Diseases awarded. (Used only for select programs.) NIBIB National Institute of Biomedical Imaging and Bioengineering EB NICHD Eunice Kennedy Shriver National Institute of Child Health and HD 5=Non‐ Request or award for a subsequent budget period within a previously Human Development competing approved project for which a recipient does not have to compete Continuation with other applications.