8Th PGRC Health Report.Cdr
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

014 5891Ny0504 88 93
New York Science Journal 2012;5(7) http://www.sciencepub.net/newyork Estimation of Area under Winter Vegetables in Punjab Districts: through Remote Sensing & GIS Technology 1 Singh Avtar, 2 Khanduri Kamlesh 1 Technical Associate, JRF,Forest Survey of India(FSI),Dehradun,India 2D.Phil Research Scholar,Dpt. of Geography,HNBGU,JRF(FSI), Uttrakhand,India [email protected] Abstract: The Study area consists of five northern districts (ex.Gurdaspur) of Punjab State, namely, Amritsar, Tarn Taran, Kapurthala, Jalandhar and Hoshiarpur. In this study, Acreage Estimation of Vegetables in northern Punjab is carried out by using Multidate IRS - P6 AWiFS Data sets of seven dates viz., September (30), October (14, 24), November (17), December (25), January (4, 13). The aim of this study is to detect area estimation under winter vegetables in Punjab districts between 2005 - 2008 using satellite images. Vegetable area carried out by decision rule based classification: two models are created, one for acreage estimation of vegetables the other for generation of NDVI of all date satellite data. After classification of the image, classified image is recoded to merge different classes of the single output category in one category. Winter Vegetables have been detected by image processing method in EDRAS imagine9.3, ArcGIS9.3. In study area, as a whole there is positive change (14.9%) in area under vegetable crop. But two districts, namely, Kapurthala and Jalandhar have experienced negative change .But in another three districts Amritsar, Tarn Taran and Hoshiarpur districts have recorded positive change in area under vegetable. [Singh Avtar, Khanduri Kamlesh. Estimation of Area under Winter Vegetables in Punjab Districts: through Remote Sensing & GIS Technology. -

State Profiles of Punjab
State Profile Ground Water Scenario of Punjab Area (Sq.km) 50,362 Rainfall (mm) 780 Total Districts / Blocks 22 Districts Hydrogeology The Punjab State is mainly underlain by Quaternary alluvium of considerable thickness, which abuts against the rocks of Siwalik system towards North-East. The alluvial deposits in general act as a single ground water body except locally as buried channels. Sufficient thickness of saturated permeable granular horizons occurs in the flood plains of rivers which are capable of sustaining heavy duty tubewells. Dynamic Ground Water Resources (2011) Annual Replenishable Ground water Resource 22.53 BCM Net Annual Ground Water Availability 20.32 BCM Annual Ground Water Draft 34.88 BCM Stage of Ground Water Development 172 % Ground Water Development & Management Over Exploited 110 Blocks Critical 4 Blocks Semi- critical 2 Blocks Artificial Recharge to Ground Water (AR) . Area identified for AR: 43340 sq km . Volume of water to be harnessed: 1201 MCM . Volume of water to be harnessed through RTRWH:187 MCM . Feasible AR structures: Recharge shaft – 79839 Check Dams - 85 RTRWH (H) – 300000 RTRWH (G& I) - 75000 Ground Water Quality Problems Contaminants Districts affected (in part) Salinity (EC > 3000µS/cm at 250C) Bhatinda, Ferozepur, Faridkot, Muktsar, Mansa Fluoride (>1.5mg/l) Bathinda, Faridkot, Ferozepur, Mansa, Muktsar and Ropar Arsenic (above 0.05mg/l) Amritsar, Tarantaran, Kapurthala, Ropar, Mansa Iron (>1.0mg/l) Amritsar, Bhatinda, Gurdaspur, Hoshiarpur, Jallandhar, Kapurthala, Ludhiana, Mansa, Nawanshahr, -
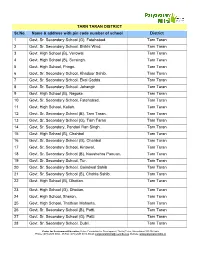
TARN TARAN DISTRICT Sr.No. Name & Address With
TARN TARAN DISTRICT Sr.No. Name & address with pin code number of school District 1 Govt. Sr. Secondary School (G), Fatehabad. Tarn Taran 2 Govt. Sr. Secondary School, Bhikhi Wind. Tarn Taran 3 Govt. High School (B), Verowal. Tarn Taran 4 Govt. High School (B), Sursingh. Tarn Taran 5 Govt. High School, Pringri. Tarn Taran 6 Govt. Sr. Secondary School, Khadoor Sahib. Tarn Taran 7 Govt. Sr. Secondary School, Ekal Gadda. Tarn Taran 8 Govt. Sr. Secondary School, Jahangir Tarn Taran 9 Govt. High School (B), Nagoke. Tarn Taran 10 Govt. Sr. Secondary School, Fatehabad. Tarn Taran 11 Govt. High School, Kallah. Tarn Taran 12 Govt. Sr. Secondary School (B), Tarn Taran. Tarn Taran 13 Govt. Sr. Secondary School (G), Tarn Taran Tarn Taran 14 Govt. Sr. Secondary, Pandori Ran Singh. Tarn Taran 15 Govt. High School (B), Chahbal Tarn Taran 16 Govt. Sr. Secondary School (G), Chahbal Tarn Taran 17 Govt. Sr. Secondary School, Kirtowal. Tarn Taran 18 Govt. Sr. Secondary School (B), Naushehra Panuan. Tarn Taran 19 Govt. Sr. Secondary School, Tur. Tarn Taran 20 Govt. Sr. Secondary School, Goindwal Sahib Tarn Taran 21 Govt. Sr. Secondary School (B), Chohla Sahib. Tarn Taran 22 Govt. High School (B), Dhotian. Tarn Taran 23 Govt. High School (G), Dhotian. Tarn Taran 24 Govt. High School, Sheron. Tarn Taran 25 Govt. High School, Thathian Mahanta. Tarn Taran 26 Govt. Sr. Secondary School (B), Patti. Tarn Taran 27 Govt. Sr. Secondary School (G), Patti. Tarn Taran 28 Govt. Sr. Secondary School, Dubli. Tarn Taran Centre for Environment Education, Nehru Foundation for Development, Thaltej Tekra, Ahmedabad 380 054 India Phone: (079) 2685 8002 - 05 Fax: (079) 2685 8010, Email: [email protected], Website: www.paryavaranmitra.in 29 Govt. -

Census of India 2011
Census of India 2011 PUNJAB SERIES-04 PART XII-B DISTRICT CENSUS HANDBOOK TARN TARAN VILLAGE AND TOWN WISE PRIMARY CENSUS ABSTRACT (PCA) DIRECTORATE OF CENSUS OPERATIONS PUNJAB CENSUS OF INDIA 2011 PUNJAB SERIES-04 PART XII - B DISTRICT CENSUS HANDBOOK TARN TARAN VILLAGE AND TOWN WISE PRIMARY CENSUS ABSTRACT (PCA) Directorate of Census Operations PUNJAB MOTIF GURU ANGAD DEV GURUDWARA Khadur Sahib is the sacred village where the second Guru Angad Dev Ji lived for 13 years, spreading the universal message of Guru Nanak. Here he introduced Gurumukhi Lipi, wrote the first Gurumukhi Primer, established the first Sikh school and prepared the first Gutka of Guru Nanak Sahib’s Bani. It is the place where the first Mal Akhara, for wrestling, was established and where regular campaigns against intoxicants and social evils were started by Guru Angad. The Stately Gurudwara here is known as The Guru Angad Dev Gurudwara. Contents Pages 1 Foreword 1 2 Preface 3 3 Acknowledgement 4 4 History and Scope of the District Census Handbook 5 5 Brief History of the District 7 6 Administrative Setup 8 7 District Highlights - 2011 Census 11 8 Important Statistics 12 9 Section - I Primary Census Abstract (PCA) (i) Brief note on Primary Census Abstract 16 (ii) District Primary Census Abstract 21 Appendix to District Primary Census Abstract Total, Scheduled Castes and (iii) 29 Scheduled Tribes Population - Urban Block wise (iv) Primary Census Abstract for Scheduled Castes (SC) 37 (v) Primary Census Abstract for Scheduled Tribes (ST) 45 (vi) Rural PCA-C.D. blocks wise Village Primary Census Abstract 47 (vii) Urban PCA-Town wise Primary Census Abstract 133 Tables based on Households Amenities and Assets (Rural 10 Section –II /Urban) at District and Sub-District level. -

Punjab Financial Corporation Sco No. 95-98, Bank Square, Sector 17-B Chandigarh 0172-2708435
PUNJAB FINANCIAL CORPORATION SCO NO. 95-98, BANK SQUARE, SECTOR 17-B CHANDIGARH 0172-2708435 LIST OF PROPERTIES FOR E-AUCTION ON AS IS WHERE IS BASIS (Rs. in lacs) S.NO. Name & Address Land Area Product Land Building Machinery Reserve Price/ (M/s) Earnest Money Deposited/ Bid increased amount DISTT. PATIALA 1. M/s Honey Plywood (P) E-auction of land measuring 4K-0M comprised of Khewat False Ceiling 12.96 3.45 0.00 16.41 Ltd. No. 1066, Khatauni No. 1751, R.No. 121, Killa No. 22 Min Tiles 0.83 Vill. Bhamana, (4-0) situated in Village Bahamna, Tehsil Samana, District 0.10 Bhawanigarh Road, Patiala as entered in jamabandi for the year 1994-95 (held Samana, Distt. Patiala and owned by M/s Honey Plywood (P) Ltd., Samana, Distt.Patiala alongwith building constructed thereon. 2. M/s Neetu Color Lab (P) E-auction of land measuring 136 sq.yds comprised in Processing & 69.63 14.13 0.64 84.40 Ltd., Khata/Khatauni No. 1816/2847, Khasra No. 3317/2394/871 Developing. 4.22 Opp. Bus Stand, min situated in Tehsil & Distt. Patiala as entered in the Coloured 0.10 Patiala jamabandi for the year 1986-87 alongwith building & printing machinery constructed thereon. 3. M/s Paras Containers (P) E-auction of land measuring 2K-1M being 41/160 share of HDDE & PVC 20.70 4.38 0.00 25.08 Ltd., Rajla-Kamaspur land measuring 8K-0M comprised of Khewat No.841, Packing 1.26 Road, Samana, Distt. Khatauni No. 1328, Khasra No. 133, Killa No. -

17 Harmanjit Singh.P65
Indian J. Phys. 83 (7), 1039-1044 (2009) Uranium concentration in drinking water samples using the SSNTDs Harmanjit Singh*, Joga Singh, Surinder Singh and B S Bajwa Department of Physics, Guru Nanak Dev University, Amritsar-143 005, Punjab, India E-mail : [email protected] Abstract : Uranium concentrations in the drinking water samples collected mainly from hand pumps along the Amritsar to Bathinda track are presented. Uranium concentration values in these samples show a wide range of variation depending upon different factors like source, location, depth and local geology etc. The observed uranium content in water samples has been found to be varying from 0.9 ± 0.08 to 63 ± 0.21 ppb and even the radon activity in ground water observed in our earlier survey carried out in this area has been found to be increasing from Amritsar towards Bathinda. The higher values were observed from the ground water samples particularly of the areas falling in belt from Zira to Maur towards the Haryana border. The values observed at certain locations are found to be higher than the highest recommended value of 15 ppb [1]. The high uranium concentration observed particularly in certain areas along this track can be attributed due to interaction of ground water with the soil formation of this region and the local subsurface geology of the region. Keywords : Water, uranium, geology, sources. PACS Nos. : 93.85.Np, 92.20.Td 1. Introduction Uranium often is grouped into a broader classification of contaminants particularly for drinking water, known as the radionuclides. The most common radionuclides found in drinking water include uranium, radon and radium. -

Brief Industrial Profile of Tarntarn District
Government of India Ministry of MSME Brief Industrial Profile of Tarntarn District Carried out by MSME DEVELOPMENT INSTITUTE Government of India, Ministry of MSME Industrial Area-‘B’ LUDHIANA-141 003 (Punjab) Telephone No.: 2531733-34-35 Fax: 091-0161-2533225 Email : [email protected] Website : www.msmedildh.gov.in Contents S. No. Topic Page No. 1. General Characteristics of the District 1.1 Location & Geographical Area 2 1.2 Topography 2 1.3 Availability of Minerals. 2 1.4 Forest 3 1.5 Administrative set up 3 2. District at a Glance 4,5 3. Industrial Scenario of District 3.1 Existing Status of Industrial Area in the District 6 3.2 Industry at a Glance 6 3.3 Year Wise Trend of Units Registered 6 3.4 Details Of Existing MSEs & Artisan Units In the District 6,7 3.5.1 Large Scale Enterprises / Public Sector Undertakings 7 3.5.2 Major Exportable Item 7 3.5.3 Growth Trends 8 3.5.4 Vendorisation / Ancillarisation of the Industry 8 3.6 Service Enterprises 8 3.6.1 Existing Service Sector 8 3.6.2 Potentials Areas for Service Sector 8 3.7 Unregistered Sector 8 3.8 Potential for New MSMEs 8 4. Existing Clusters of Micro & Small Enterprises 4.1 Detail of Major Clusters 9 4.1.1 Manufacturing Sector 9 4.1.2 Service Sector 9 4.2 Details of Identified Cluster 9 5. General issues raised by Industrial Associations 9 6. Prospects of Training Programmes(2012-13) 9 7. Action Plan for MSME Schemes(2012-13) 10 8. -

Availability of Institutions Imparting Higher Education: a Review (A Comparative Study of Punjab and Haryana)
INTERNATIONAL JOURNAL FOR INNOVATIVE RESEARCH IN MULTIDISCIPLINARY FIELD ISSN – 2455-0620 Volume - 3, Issue - 7, July - 2017 Availability of Institutions Imparting Higher Education: A Review (A Comparative Study of Punjab and Haryana) Dr. Aparna Joshi Assistant Professor, Department of Geography, Lovely Professional University, Phagwara, Punjab, India Email - [email protected] Abstract: Higher education must provide knowledge and skills to build productive careers so that the people have professionally satisfying lives and also contribute positively to a strong and vibrant economy. The greater the weightage within an economy of the components representing higher levels of educational attainment and professional expertise, the higher is the level of technology being used within the economy. Further, given the significance of human capital stock for achieving higher levels of development, an examination of the structure of human capital stock and the nature of relationship between attainment in terms of the different components of human capital stock and the level of development becomes an issue of considerable significance. The present paper accesses the availability of educational institutions imparting higher education in Punjab and Haryana region by taking into account the number of different types of recognized higher education institutions. The study is totally based upon secondary sources of data and aims to analyse the growth of higher education institutions during 1971-2011, understand their spatial pattern at the district level in 2010-11 and compare the two states of Punjab and Haryana to find out the overall performance with respect to availability of recognized institutions imparting higher education in the study region. Key Words: Higher education, Educational institutions, Growth, Level of Development. -

Changing Scenario of Education in Educationally Backward Areas of Punjab
International Journal of Humanities and Social Science Invention (IJHSSI) ISSN (Online): 2319 – 7722, ISSN (Print): 2319 – 7714 www.ijhssi.org ||Volume 7 Issue 09 Ver. II ||September 2018 || PP 01-06 Changing Scenario of Education in Educationally Backward Areas of Punjab Mridula Pushkarna Deptt of GeographyR K Arya College, Nawanshahr ABSTRACT:For any nation education plays an important role for the development. If the literacy rate is in the particular area is high that clearly depicts the prosperity in terms of economic conditions, labour productivity, health and culture. Improvement in education has a very long term effects on the welfare of the nation. It should always be very important for all the policymakers that improvement in the education sector and every community of the society and each part of the region should be benefitted; no caste or no gender should be given priority. Education is the basic necessity so it should be affordable to all. Equalization at education levels removes all the barriers of regional inequalities and gender discrimination. From the last few decades, with all the efforts of government and nongovernmental organisations there is an improvements in education levels as well as literacy rates but some regions of India are still deprived. For the recognition of those particular areas, the educationally backward districts were recognised and further for the implementation of the policies in a proper manner, Educationally Backward Blocks (EBB) were recognised in 2007 on the basis of census records of 2001. The researcher is trying to find out the improvements in the EBB’S of one of the prosperous state of Punjab where 21blocks were recognised as backward in education. -

BADP Tarn Taran Report
CHAPTER - I INTRODUCTION 1.1 Introduction Border Area Development Programme (BADP) had been started by the Department of Border Management, Ministry of Home Affairs, Government of India during VII Five Year Plan in Western Region of India. During the VIII FYP, the programme was extended to the States that had an international border with Bangladesh. During the IX FYP, the programme was further extended to the States having international border with Myanmar, China, Bhutan and Nepal. At present, BADP covers 362 blocks located along the international border in 96 border districts of 17 States that share an international land border with India‟s neighbouring countries. 1.2 Objectives of BADP The main objective of the programme is to meet the special developmental needs of the people living in remote and inaccessible areas situated near the international border and to saturate the border areas with essential infrastructure through convergence of BADP/Central/State//Local schemes and through a participatory approach. The specific objectives of the programme are:- • balanced development of sensitive border areas through adequate provision of infrastructure; and • promotion of a sense of security amongst the local population. 1.3 Coverage of Border Area Development Programme Punjab has 553 KM long international border with Pakistan that spread along 4 districts, viz.,Ferozepur, Gurdaspur, Amritsar and Tarn Taran (the last was created in April 2006). As many as 19 blocks in the State of Punjab (Attari block included in 2010-11), with an aggregate geographical area of 6369.82 Sq.km, are being covered under Border Area Development Programme (Table 1.1). -

No. EARO (MPLADS)-2006/21933-55 Government of Punjab Department
No. E.A.R.O (MPLADS)-2006/21933-55 Government of Punjab Department of Planning (MPLADS Section) To 1. Dr.R.C. Panda, Secretary, MOSPI Government of India 2. Principal Secretary to Govt. of Punjab , Deptt. Of Rural Development. 3. Principal Secretary to Govt. of Punjab, Deptt. Of Local Government. 4. All Deputy Commissioners in the State. Dated Chandigarh, the 27 November, 2006. Subject: Meeting of the State MPLADS Committee. Sir/Madam It is intimated that the first meeting of the State Committee on MPLADS under the Chairmanship of Worthy Chief Secretary, Punjab will be held on 11-12-06 at 12.45 PM at Punjab Bhawan, Sector-3, Chandigarh. All Hon’ble Members of Parliament from Punjab are special invitees to the meeting. The agenda of the meeting is enclosed which is based on the figures upto 31.10.06. Uptodate agenda (upto 30.11.06) will be supplied in the meeting. Kindly make it convenient to attend the meeting. Sd/- Special Secretary to Govt. of Punjab Department of Planning Endst. No.ESO.Pb.(MPLADS)-2006/21956-75 Dated:27-11-06 A copy is forwarded to all Hon’ble Members of Parliament from Punjab with the request that they may please make it convenient to attend the meeting. Sd/- Special Secretary to Govt. of Punjab Department of Planning. To All Members of Parliament (As per list) Endst. No.ESO.Pb.(MPLADS)-2006/21976 Dated:27-1106 A copy is forwarded to the Secretary to Chief Secretary for the information of Worthy Chief Secretary to Govt.of Punjab. Sd/- Special Secretary to Govt. -

Tranche 3: Imperial Highway Heritage
Initial Environmental Examination Project Number: 40648-034 May 2018 IND: Infrastructure Development Investment Program for Tourism (IDIPT) - Tranche 3 Package : Imperial Highway Heritage Conservation and Visitor Facility Development (Lot -2), Baradari and Kos Minars in TarnTaran District, Punjab Submitted by: Program Management Unit, Punjab Heritage and Tourism Board, Chandigarh This report has been submitted to ADB by the Program Management Unit, Punjab Heritage and Tourism Board, Chandigarh and is made publicly available in accordance with ADB’s Public Communications Policy (2011). It does not necessarily reflect the views of ADB. This initial environment examination report is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. Compliance matrix to the Queries from ADB Package no. PB/IDIPT/T3/12/18 (Lot-2): Imperial Highway Heritage conservation and visitor facility development (Lot-2) Baradari and Kos Minars in Tarn Taran district, Punjab Sl.no Comments from ADB Response from PMU 1. We note from para 7 (page 1 and 2) that the Noted. The given information in the para 7 (pg 1 scope of works are conservation works for & 2) is for the Executive Summary and hence it is monuments at (i) Baradari located in not in detail.