Lopinavir; Ritonavir (All Populations Monograph)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

35 Cyproterone Acetate and Ethinyl Estradiol Tablets 2 Mg/0
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION PrCYESTRA®-35 cyproterone acetate and ethinyl estradiol tablets 2 mg/0.035 mg THERAPEUTIC CLASSIFICATION Acne Therapy Paladin Labs Inc. Date of Preparation: 100 Alexis Nihon Blvd, Suite 600 January 17, 2019 St-Laurent, Quebec H4M 2P2 Version: 6.0 Control # 223341 _____________________________________________________________________________________________ CYESTRA-35 Product Monograph Page 1 of 48 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION ....................................................................... 3 SUMMARY PRODUCT INFORMATION ............................................................................................. 3 INDICATION AND CLINICAL USE ..................................................................................................... 3 CONTRAINDICATIONS ........................................................................................................................ 3 WARNINGS AND PRECAUTIONS ....................................................................................................... 4 ADVERSE REACTIONS ....................................................................................................................... 13 DRUG INTERACTIONS ....................................................................................................................... 16 DOSAGE AND ADMINISTRATION ................................................................................................ 20 OVERDOSAGE .................................................................................................................................... -

KALETRA (Lopinavir/Ritonavir)
HIGHLIGHTS OF PRESCRIBING INFORMATION CONTRAINDICATIONS These highlights do not include all the information needed to use • Hypersensitivity to KALETRA (e.g., toxic epidermal necrolysis, Stevens- KALETRA safely and effectively. See full prescribing information for Johnson syndrome, erythema multiforme, urticaria, angioedema) or any of KALETRA. its ingredients, including ritonavir. (4) • Co-administration with drugs highly dependent on CYP3A for clearance KALETRA (lopinavir and ritonavir) tablet, for oral use and for which elevated plasma levels may result in serious and/or life- KALETRA (lopinavir and ritonavir) oral solution threatening events. (4) Initial U.S. Approval: 2000 • Co-administration with potent CYP3A inducers where significantly reduced lopinavir plasma concentrations may be associated with the potential for RECENT MAJOR CHANGES loss of virologic response and possible resistance and cross resistance. (4) Contraindications (4) 12/2019 WARNINGS AND PRECAUTIONS The following have been observed in patients receiving KALETRA: INDICATIONS AND USAGE • The concomitant use of KALETRA and certain other drugs may result in KALETRA is an HIV-1 protease inhibitor indicated in combination with other known or potentially significant drug interactions. Consult the full antiretroviral agents for the treatment of HIV-1 infection in adults and prescribing information prior to and during treatment for potential drug pediatric patients (14 days and older). (1) interactions. (5.1, 7.3) • Toxicity in preterm neonates: KALETRA oral solution should not be used DOSAGE AND ADMINISTRATION in preterm neonates in the immediate postnatal period because of possible Tablets: May be taken with or without food, swallowed whole and not toxicities. A safe and effective dose of KALETRA oral solution in this chewed, broken, or crushed. -

Truvada (Emtricitabine / Tenofovir Disoproxil)
Pre-exposure Prophylaxis (2.3) HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use Recommended dose in HIV-1 uninfected adults: One tablet TRUVADA safely and effectively. See full prescribing information (containing 200 mg/300 mg of emtricitabine and tenofovir for TRUVADA. disoproxil fumarate) once daily taken orally with or without food. (2.3) TRUVADA® (emtricitabine/tenofovir disoproxil fumarate) tablets, for oral use Recommended dose in renally impaired HIV-uninfected Initial U.S. Approval: 2004 individuals: Do not use TRUVADA in HIV-uninfected individuals if CrCl is below 60 mL/min. If a decrease in CrCl is observed in WARNING: LACTIC ACIDOSIS/SEVERE HEPATOMEGALY WITH uninfected individuals while using TRUVADA for PrEP, evaluate STEATOSIS, POST-TREATMENT ACUTE EXACERBATION OF potential causes and re-assess potential risks and benefits of HEPATITIS B, and RISK OF DRUG RESISTANCE WITH USE OF continued use. (2.4) TRUVADA FOR PrEP IN UNDIAGNOSED HIV-1 INFECTION -----------------------DOSAGE FORMS AND STRENGTHS------------------- See full prescribing information for complete boxed warning. Tablets: 200 mg/300 mg, 167 mg/250 mg, 133 mg/200 mg, and 100 Lactic acidosis and severe hepatomegaly with steatosis, mg/150 mg of emtricitabine and tenofovir disoproxil fumarate . (3) including fatal cases, have been reported with the use of nucleoside analogs, including VIREAD, a component of TRUVADA. (5.1) --------------------------------CONTRAINDICATIONS----------------------------- TRUVADA is not approved for the treatment of chronic Do not use TRUVADA for pre-exposure prophylaxis in individuals with hepatitis B virus (HBV) infection. Severe acute unknown or positive HIV-1 status. TRUVADA should be used in exacerbations of hepatitis B have been reported in patients HIV-infected patients only in combination with other antiretroviral coinfected with HIV-1 and HBV who have discontinued agents. -
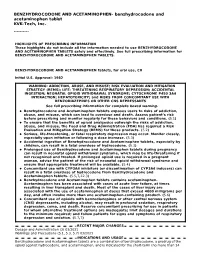
These Highlights Do Not Include All the Information Needed to Use BENZHYDROCODONE and ACETAMINOPHEN TABLETS Safely and Effectively
BENZHYDROCODONE AND ACETAMINOPHEN- benzhydrocodone and acetaminophen tablet KVK-Tech, Inc. ---------- HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use BENZHYDROCODONE AND ACETAMINOPHEN TABLETS safely and effectively. See full prescribing information for BENZHYDROCODONE AND ACETAMINOPHEN TABLETS. BENZHYDROCODONE AND ACETAMINOPHEN tablets, for oral use, CII Initial U.S. Approval: 1982 WARNING: ADDICTION, ABUSE, AND MISUSE; RISK EVALUATION AND MITIGATION STRATEGY (REMS); LIFE- THREATENING RESPIRATORY DEPRESSION; ACCIDENTAL INGESTION; NEONATAL OPIOID WITHDRAWAL SYNDROME; CYTOCHROME P450 3A4 INTERACTION; HEPATOTOXICITY; and RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS See full prescribing information for complete boxed warning. Benzhydrocodone and Acetaminophen tablets exposes users to risks of addiction, abuse, and misuse, which can lead to overdose and death. Assess patient’s risk before prescribing and monitor regularly for these behaviors and conditions. (5.1) To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the Food and Drug Administration (FDA) has required a Risk Evaluation and Mitigation Strategy (REMS) for these products. (5.2) Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely, especially upon initiation or following a dose increase. (5.3) Accidental ingestion of Benzhydrocodone and Acetaminophen tablets, especially by children, can result in a fatal overdose of hydrocodone. (5.3) Prolonged use of Benzhydrocodone and Acetaminophen tablets during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated. If prolonged opioid use is required in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available. -

Glaxosmithkline Bangladesh Limited (GSK)
GlaxoSmithKline Bangladesh Limited (GSK) Recruitment and Selection Process of GlaxoSmithKline Bangladesh Limited: An Evaluation nd Date of Submission: 2 September, 2014 ©Daffodil International University DAFFODIL INTERNATIONAL UNIVERSITY Internship Report On Recruitment and Selection Process of GlaxoSmithKline Bangladesh Limited: An Evaluation Submitted To Dr. Zakir Hossain Dean& Professor Faculty of Business & Economics Daffodil International University Submitted By Ishrat Jahan ID: 131-14-1019 Masters of Business Administration Daffodil International University Date of Submission: 2nd September, 2014 ©Daffodil International University Letter of Transmittal September 2, 2014 To Dr. Zakir Hossain Dean & Professor Faculty of Business and Economics Daffodil International University Dhaka-1205 Subject: Submission of internship report on recruitment and selection process: An evaluation of GlaxoSmithKline Bangladesh Limited Sir, I am highly satisfied to submit my report on recruitment and selection process: an evaluation of GSK. For preparing this report I tried my best to accumulate relevant and upgraded information from available sources. In preparing this report, I tried my level best to make it a complete one and sincerely look forward to any possible correction. I am very glad because you also given the opportunity to prepare this report .I hope that this report will meet the standards of your judgments. Your Sincerely ---------------- Ishrat Jahan ©Daffodil International University i Certificate of the Supervisor This is to certify that the internship report titled ―Recruitment and Selection Process of GlaxoSmithKline Bangladesh Limited: An Evaluation‖, has been prepared by Ms. Ishrat Jahan bearing ID: 131-14-1019 under my supervision, a practical study on GlaxoSmithKline Bangladesh Limited. I think on the basic of declaration Ms. -

Summary Analgesics Dec2019
Status as of December 31, 2019 UPDATE STATUS: N = New, A = Advanced, C = Changed, S = Same (No Change), D = Discontinued Update Emerging treatments for acute and chronic pain Development Status, Route, Contact information Status Agent Description / Mechanism of Opioid Function / Target Indication / Other Comments Sponsor / Originator Status Route URL Action (Y/No) 2019 UPDATES / CONTINUING PRODUCTS FROM 2018 Small molecule, inhibition of 1% diacerein TWi Biotechnology / caspase-1, block activation of 1 (AC-203 / caspase-1 inhibitor Inherited Epidermolysis Bullosa Castle Creek Phase 2 No Topical www.twibiotech.com NLRP3 inflamasomes; reduced CCP-020) Pharmaceuticals IL-1beta and IL-18 Small molecule; topical NSAID Frontier 2 AB001 NSAID formulation (nondisclosed active Chronic low back pain Phase 2 No Topical www.frontierbiotech.com/en/products/1.html Biotechnologies ingredient) Small molecule; oral uricosuric / anti-inflammatory agent + febuxostat (xanthine oxidase Gout in patients taking urate- Uricosuric + 3 AC-201 CR inhibitor); inhibition of NLRP3 lowering therapy; Gout; TWi Biotechnology Phase 2 No Oral www.twibiotech.com/rAndD_11 xanthine oxidase inflammasome assembly, reduced Epidermolysis Bullosa Simplex (EBS) production of caspase-1 and cytokine IL-1Beta www.arraybiopharma.com/our-science/our-pipeline AK-1830 Small molecule; tropomyosin Array BioPharma / 4 TrkA Pain, inflammation Phase 1 No Oral www.asahi- A (ARRY-954) receptor kinase A (TrkA) inhibitor Asahi Kasei Pharma kasei.co.jp/asahi/en/news/2016/e160401_2.html www.neurosmedical.com/clinical-research; -

Annual Report 2013
Annual Report 2013 “ Being active and having a positive outlook on life is what keeps me going every day.” Overview of 2013 “ Our performance in 2013 was defined by remarkable &R D output and further delivery of sustained financial performance for our shareholders.” Please go to page 4 for more More at gsk.com Performance highlights £26.5bn £8.0bn £7.0bn £5.2bn Group turnover Core* operating profit Total operating profit Returned to shareholders 6 112.2p 112.5p 13% Major medicines approved Core* earnings per share Total earnings per share Estimated return on R&D investment 10 6 1st 1st Potential phase III study starts in 2014/15 Potential medicines with phase III data in Access to Medicines Index Pharmaceutical company to sign AllTrials expected 2014/15 campaign for research transparency Front cover story Betty, aged 65, (pictured) has Chronic “ Health is important to me, Obstructive Pulmonary Disease (COPD). She only has 25% lung capacity. This means I try to take care of my she finds even everyday tasks difficult, but medicines and inhaled oxygen allow her to health with all the tools live as normal a life as she can. Betty’s mindset I have and do the best is to stay busy and active, so every week she goes to rehab exercise classes. that I can with it.” COPD is a disease of the lungs that leads to Betty, COPD patient, damaged airways, causing them to become North Carolina, USA narrower and making it harder for air to get in and out. 210 million people around the world are estimated to have COPD. -

Ritonavir Mylan, INN-Ritonavir
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Ritonavir Mylan 100 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each film-coated tablet contains 100 mg of ritonavir. Excipient with known effect Each film-coated tablet contains 87.75 mg of sodium. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet (tablet). Yellow, capsule shaped, biconvex, beveled edge film-coated tablet, approximately 19.1 mm x 10.2 mm, debossed with ‘M163’ on one side and blank on the other side. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Ritonavir is indicated in combination with other antiretroviral agents for the treatment of HIV-1 infected patients (adults and children of 2 years of age and older). 4.2 Posology and method of administration Ritonavir Mylan should be administered by physicians who are experienced in the treatment of HIV infection. Posology Ritonavir dosed as a pharmacokinetic enhancer When ritonavir is used as a pharmacokinetic enhancer with other protease inhibitors the Summary of Product Characteristics for the particular protease inhibitor must be consulted. The following HIV-1 protease inhibitors have been approved for use with ritonavir as a pharmacokinetic enhancer at the noted doses. Adults Amprenavir 600 mg twice daily with ritonavir 100 mg twice daily. Atazanavir 300 mg once daily with ritonavir 100 mg once daily. Fosamprenavir 700 mg twice daily with ritonavir 100 mg twice daily. Lopinavir co-formulated with ritonavir (lopinavir/ritonavir) 400 mg/100 mg or 800 mg/200 mg. Saquinavir 1,000 mg twice daily with ritonavir 100 mg twice daily in ART experienced patients. -

A Case Study of Glaxosmithkline Plc )
)l GROWTH THROUGH MERGER: A CASE STUDY OF GLAXOSMITHKLINE PLC ) / BY JUNE WANGARI UNIVERSITY OF NAIR03J LOWER KABETE LIBRARY A MANAGEMENT RESEARCH PROJECT SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE AWARD OF DEGREE OF MASTER OF BUSINESS ADMINISTRATION (MBA), SCHOOL OF BUSINESS, UNIVERSITY OF NAIROBI JULY, 2008 DECLARATION I declare that this project is my original work and has never been presented for academic purposes in any other University. CANDIDATE: JUNE WANGARI DATE .(.91. This research project has been submitted for examination with my approval as the University Supervisor SIGNED. DATE. Prof. Evans Aosa Department Of Business Administration, School Of Business, University Of Nairobi 11 DEDICATION I dedicate this project to my daughter Jemima, who was born within the first year of my post graduate studies. And now that she is in kindergarten, I see that I have instilled in her the love for reading and learning and I trust that she will go very far. iii ACKNOWLEDGEMENT I thank God for seeing me through my studies as I tried to balance between my family, my work and my studies. I wish to acknowledge the contributions that were made in the course of this project by several individuals and organizations. I wish to acknowledge gratefully the following people, whose effort influenced the content and direction of this project. My first thanks go to my Supervisor Prof. Evans Aosa for his constant analytical criticism and encouragement. Thanks a lot. I wish to thank my friends for a lot of support and encouragement to me in pursuit of this goal. -

Administering Medications Through Feeding Tubes (GT, NG, JT, NJ, Etc.)
Administering Medications through Feeding Tubes (GT, NG, JT, NJ, etc.) This content was developed by: Adrian Turner, Pharm.D.- Cook Children’s Medical Center, Ft. Worth, TX Marry Vuong, Pharm.D.- Nicklaus Children’s Health System, Miami, FL Veronica Hood, PhD- Dravet Syndrome Foundation, Cherry Hill, NJ This information should not replace guidance from a health care professional managing the care of your child or loved one. Caregivers should use this guide to help inform conversations as part of the health care team, working with medical professionals to determine the best medications and routes of administration to use given the individual patient’s medical history and needs. Sometimes oral intake is not possible or is not ideal. In these instances, the use of alternative routes can be quite beneficial. Both nutrition and medication administration can be improved or maintained through the appropriate use of enteral alternatives such as gastrostomy tubes (GT), nasogastric tubes (NG), gastrostomy buttons (G-Buttons; GB), jejunostomy tubes (JT), and nasojejunal tubes (NJ). However, these routes present unique barriers and considerations the traditional oral route does not. Miscellaneous tips for medication administration via feeding tubes1-8: • Product choices: o Generally, products that are extended release or delayed release should not be crushed. There are a few exceptions, outlined below. o If using a liquid formulation, elixirs and suspensions may be less likely to clump with enteral nutrition compared to syrups. o Some liquids may contain high amounts of sugar alcohols (e.g. sorbitol, malitol) or have a high osmolality. Both of these can increase the risk of developing abdominal cramping, bloating, nausea, and diarrhea. -

Managing Drug Interactions in the Treatment of HIV-Related Tuberculosis
Managing Drug Interactions in the Treatment of HIV-Related Tuberculosis National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention Division of Tuberculosis Elimination Managing Drug Interactions in the Treatment of HIV-Related Tuberculosis Centers for Disease Control and Prevention Office of Infectious Diseases National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention Division of Tuberculosis Elimination June 2013 This document is accessible online at http://www.cdc.gov/tb/TB_HIV_Drugs/default.htm Suggested citation: CDC. Managing Drug Interactions in the Treatment of HIV-Related Tuberculosis [online]. 2013. Available from URL: http://www.cdc.gov/tb/TB_HIV_Drugs/default.htm Table of Contents Introduction 1 Methodology for Preparation of these Guidelines 2 The Role of Rifamycins in Tuberculosis Treatment 4 Managing Drug Interactions with Antivirals and Rifampin 5 Managing Drug Interactions with Antivirals and Rifabutin 9 Treatment of Latent TB Infection with Rifampin or Rifapentine 10 Treating Pregnant Women with Tuberculosis and HIV Co-infection 10 Treating Children with HIV-associated Tuberculosis 12 Co-treatment of Multidrug-resistant Tuberculosis and HIV 14 Limitations of these Guidelines 14 HIV-TB Drug Interaction Guideline Development Group 15 References 17 Table 1a. Recommendations for regimens for the concomitant treatment of tuberculosis and HIV infection in adults 21 Table 1b. Recommendations for regimens for the concomitant treatment of tuberculosis and HIV infection in children 22 Table 2a. Recommendations for co-administering antiretroviral drugs with RIFAMPIN in adults 23 Table 2b. Recommendations for co-administering antiretroviral drugs with RIFAMPIN in children 25 Table 3. Recommendations for co-administering antiretroviral drugs with RIFABUTIN in adults 26 ii Introduction Worldwide, tuberculosis is the most common serious opportunistic infection among people with HIV infection. -

DESCOVY, and Upon Diagnosis of These Highlights Do Not Include All the Information Needed to Use Any Other Sexually Transmitted Infections (Stis)
HIGHLIGHTS OF PRESCRIBING INFORMATION once every 3 months while taking DESCOVY, and upon diagnosis of These highlights do not include all the information needed to use any other sexually transmitted infections (STIs). (2.2) DESCOVY safely and effectively. See full prescribing information • Recommended dosage: for DESCOVY. • Treatment of HIV-1 Infection: One tablet taken once daily with or ® without food in patients with body weight at least 25 kg. (2.3) DESCOVY (emtricitabine and tenofovir alafenamide) tablets, for • HIV-1 PrEP: One tablet taken once daily with or without food in oral use individuals with body weight at least 35 kg. (2.4) Initial U.S. Approval: 2015 • Renal impairment: DESCOVY is not recommended in individuals with WARNING: POST-TREATMENT ACUTE EXACERBATION OF estimated creatinine clearance below 30 mL per minute. (2.5) HEPATITIS B and RISK OF DRUG RESISTANCE WITH USE ----------------------DOSAGE FORMS AND STRENGTHS-------------------- OF DESCOVY FOR HIV-1 PRE-EXPOSURE PROPHYLAXIS Tablets: 200 mg of FTC and 25 mg of TAF (3) (PrEP) IN UNDIAGNOSED EARLY HIV-1 INFECTION See full prescribing information for complete boxed warning. -------------------------------CONTRAINDICATIONS------------------------------ DESCOVY for HIV-1 PrEP is contraindicated in individuals with Severe acute exacerbations of hepatitis B (HBV) have been unknown or positive HIV-1 status. (4) reported in HBV-infected individuals who have discontinued products containing emtricitabine (FTC) and/or tenofovir -----------------------WARNINGS AND PRECAUTIONS----------------------- disoproxil fumarate (TDF), and may occur with • Comprehensive management to reduce the risk of sexually discontinuation of DESCOVY. Hepatic function should be transmitted infections (STIs), including HIV-1, when DESCOVY is monitored closely in these individuals.