Perinatal Health Services Component Plan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Connected Members (Query-Based Exchange) As of 9/1/19
Connected Members (Query-Based Exchange) As of 9/1/19 State Georgia Department of Behavioral Health and Development Disabilities Agencies (DBHDD) – Shares patient discharge records Georgia Department of Juvenile Justice (DJJ) – Views patient health information for youth in their care Georgia Department of Public Health (DPH) – Bi-directional submission gateway for immunization data (GRITS), eLab and Syndromic Surveillance reporting; contributes immunization information Georgia Division of Family and Children Services (DFCS) – Views patient health information for youth in their care Georgia Medicaid/Department of Community Health (DCH) – Contributes Medicaid claims (health, dental, pharmacy) information. Medicaid providers using GAMMIS can view patient health information. Care Care Management Organizations facilitate care coordination for Medicare and Medicaid patients, Management including PeachCare for Kids(r), Georgia Families(r) and Planning for Healthy Babies (r) (P4HB(r)) Organizations Amerigroup – shares care plans and views patient health information CareSource – shares care plans and views patient health information Peach State – views patient health information WellCare – views patient health information Health Shares patient health information from their connected providers Systems Children’s Healthcare of Atlanta (CHOA) – Georgia’s largest children’s hospital Emory Healthcare – Georgia’s largest academic hospital Grady Health System – Georgia’s largest public hospital Gwinnett Health System – Serves one of the -

Moms Æ FLIP OVER for Atlanta Parent!
atlanta BABYFROM ATLANTA PARENT MAGAZINE Delivery Decisions Words of Wisdom for New Moms æ FLIP OVER for Atlanta Parent! Mom- Approved Obstetricians Feeding Help for Parents. Powered by Experts. Strong4Life.com By the age of 3, your baby will develop eating habits that can last a lifetime, so you’re smart to get a jump on your baby’s nutrition. It’s easy with Strong4Life.com—a unique parenting website from the experts you trust at Children’s Healthcare of Atlanta. At Strong4Life.com, you can: Ask an expert Sign up for Browse for who is a our monthly tips by age parent too e-newsletter ©2018 Children’s Healthcare of Atlanta Inc. All rights reserved. The Doctor’s Office to your Doorstep Moms-to-be: We Come to You! Are you tired of ... OB2me alleviates all of these and provides l fighting Atlanta traffic to get the luxury and convenience of bringing to the doctor’s office? quality prenatal care to your doorstep while l having to take time off from still delivering your baby at the hospital! work or finding childcare? l extended, unpredictable OB2me.com waiting room times? l minimal face to face time with your provider? l inconvenient appointment times? OB2me is a Division of 2me Healthcare, LLC atlanta BABYFROM ATLANTA PARENT MAGAZINE Guide for New and Expectant Parents 7 / Advice for New Moms 20 / Where Will You While many “words of wisdom” new mothers Have Your Baby? receive may sound clichéd, here are a few Use Atlanta truths that help with life in general, and Parent’s easy- parenthood in particular. -

Georgia Committee for Trauma Excellence
Georgia Committee for Trauma Excellence MEETING MINUTES Thursday November 8, 2018 Conference Call MEMBERS ON CALL REPRESENTING Liz Atkins, Chair Grady Memorial Gina Solomon, Past Chair Gwinnett MediCal Center Regina Medeiros, GTC Georgia Trauma Commission Kristal Smith, Injury Prevention NaviCent Health MediCal Center Anastasia Hartigan, PI DoCtors Hospital of Augusta Erin MoorCones, Education Grady Memorial Hospital OTHERS ON CALL REPRESENTING Amanda Wright Augusta University NanCy Friedel CHOA Egleston Jennifer Hutchinson CHOA at Scottish Rite Joni Napier Crisp Regional Hospital Janann Dunnavant Crisp Regional Hospital Farrah Parker DoCtor’s Hospital, HCA Gail Thornton Emanuel County Hospital Kristen Campbell Fairview Park Hospital Melissa Parris Floyd MediCal Center Katie Hasty Floyd MediCal Center Susan Campis Grady Burn Center Kenya Cosby Grady Burn Center Bernadette Frias Grady Memorial Hospital Elizabeth Williams Mays Grady Memorial Hospital Sarah Parker Grady Memorial Hospital Rayma Stephens Gwinnett MediCal Center RaChelle Bloom Gwinnett MediCal Center Colleen Horne Gwinnett MediCal Center Barlynda Bryant Gwinnett MediCal Center Georgia Committee of Trauma Excellence Meeting Minutes: 08 November 2018 Page 1 Kim Brown Hamilton MediCal Center Karrie Page Meadows Regional MiChele Benton Morgan Memorial University Tawnie Campbell NaviCent Health MediCal Center Josephine Fabico-Dulin NaviCent Health MediCal Center Jessica Mantooth Northeast Georgia MediCal Center Jesse Gibson Northeast Georgia MediCal Center Laura Wolf Northeast Georgia -

March 6, 2019 – March 12, 2019 Need Projection Analyses
Use the links below for easy navigation Letters of Intent Letters of Intent - Expired New CON Applications Pending/Complete Applications Pending Review/Incomplete CON Applications Office of Health Planning Recently Approved CON Applications Recently Denied CON Applications Appealed CON Projects Letters of Determination Requests for Miscellaneous Letters of Determination Appealed Determinations DET Review LNR Conversion Requests for LNR for Diagnostic or Therapeutic Equipment Requests for LNR for Establishment CERTIFICATE OF NEED of Physician-Owned Ambulatory Surgery Facilities Appealed LNRs Requests for Extended Implementation/Performance Period Batching Notifications - Fall March 6, 2019 – March 12, 2019 Need Projection Analyses New Batching Review Winter Cycle Fall Cycle Non-Filed or Incomplete Surveys Georgia Department of Community Health Office of Health Planning Indigent-Charity Shortfalls 2 Peachtree Street 5th Floor CON Filing Requirements (effective July 18, 2017) Atlanta, Georgia 30303-3159 Contact Information (404) 656-0409 (404) 656-0442 Fax Verification of Lawful Presence within U.S. www.dch.georgia.gov Periodic Reporting Requirements CON Thresholds Open Record Request Form Web Links Certificate of Need Appeal Panel www.GaMap2Care.info Letters of Intent LOI2019010 Tanner Imaging Center, Inc. Development of Freestanding Imaging Center on Tanner Medical Center-Carrollton Campus Received: 2/15/2019 Application must be submitted on: 3/18/2019 Site: 706 Dixie Street, Carrollton, GA 30117 (Carroll County) Estimated Cost: $2,200,000 -

Health Planning Review Board Members
Use the links below for easy navigation Letters of Intent Expired Letters of Intent New CON Applications Pending Review/Incomplete Applications Pending Review/Complete Applications Recently Approved Applications OFFICE OF HEALTH PLANNING Recently Denied Applications Withdrawn Applications Appealed Determinations Appealed LNRs Appealed CON Projects Requests for LNR for Establishment of Physician-Owned Ambulatory Surgery Facilities Requests for LNR for Diagnostic or Therapeutic Equipment Requests for Miscellaneous Letters of CERTIFICATE OF NEED Determination Requests for Extended Implementation/Performance Period Batching Notifications-Fall Need Projection Analyses December 9, 2015 – December 15, 2015 New Batching Review Summer Cycle Fall Cycle Non-Filed or Incomplete Surveys Indigent-Charity Shortfalls Legislation Affecting CON CON Filing Requirements (effective July 1, 2008) Georgia Department of Community Health Reporting Requirements Office of Health Planning (effective July 1, 2008) 2 Peachtree Street Certificate of Need Appeal Panel 5th Floor Atlanta, Georgia 30303-3159 Contact Information (404) 656-0409 Open Record Request Form (404) 656-0442 Fax Special Note www.dch.georgia.gov New CON Thresholds www.GaMap2Care.info New! Web Links Letters of Intent LOI2015073 Hamilton Medical Center Consolidation of OP Cancer Services into Single Facility on Campus Received: 11/19/2015 Application must be submitted on: 12/21/2015 Site: 1200 Memorial Drive, Dalton, GA 30720 (Whitfield County) Estimated Cost: $30,000,000 LOI2015074 Floyd Medical Center -

General Hospitals Meeting Safety Net Hospital Criteria
General Hospitals Meeting Safety Net Hospital Criteria Medicaid & Teaching or Designated Peachcare Adms Uncomp Indigent Uncomp Indigent & SSDR County Facility Name Children's Hospitals Trauma Center >20% Care >6% Charity >10% 1 Paulding WellStar Paulding Hospital X X 1 Whitfield Hamilton Medical Center X X X 1 Polk Polk Medical Center X X 1 Bartow Cartersville Medical Center X X 1 Floyd Floyd Medical Center X X X X 1 Floyd Redmond Regional Medical Center X X 2 Lumpkin Chestatee Regional Hospital X X 3 Douglas WellStar Douglas Hospital X X 3 Gwinnett Gwinnett Medical Center X X X Children's Healthcare of Atlanta at 3 DeKalb Egleston X X X Children's Healthcare of Atlanta at Scottish 3 Fulton Rite X X X 3 Cherokee Northside Hospital Cherokee X X 3 Cobb WellStar Cobb Hospital X X X Children's Healthcare of Atlanta at Hughes 3 Fulton Spalding X X X X 3 Cobb WellStar Kennestone Hospital X X 3 Fulton Emory University Hospital Midtown X X 3 Fulton WellStar Atlanta Medical Center X X X 3 Fulton Grady Memorial Hospital X X X X X Prepared: 10/5/2018 Page 1 of 3 General Hospitals Meeting Safety Net Hospital Criteria Medicaid & Teaching or Designated Peachcare Adms Uncomp Indigent Uncomp Indigent & SSDR County Facility Name Children's Hospitals Trauma Center >20% Care >6% Charity >10% 3 DeKalb DeKalb Medical Center X X 3 DeKalb DeKalb Medical Center at Hillandale X X 4 Spalding WellStar Spalding Regional Hospital X X 4 Upson Upson Regional Medical Center X X X 4 Troup WellStar West Georgia Medical Center X X 5 Newton Piedmont Newton Hospital X X -

Health-Careers-Manual-2016.Pdf
30417 Health Career Booklet Cvr_r1.indd 1 3/15/16 12:42 PM Table of Contents Acknowledgments Foothills Area Health Education Center (AHEC) is pleased to present the 10th edition of Health Careers in Georgia. This publication is produced through the partnership of the Georgia Statewide AHEC Network consisting of six centers with support from the Georgia legislature and the US Department of Title Page ........................................................................3 Health and Human Services Health Resources and Services Administration. Many community and academic partners contributed time, expertise, and resources in producing this resource for the current and future healthcare workforce. Some content, photos, and/or layout ideas were provided by Pam What is AHEC? ....................................................................4 Reynolds and SOWEGA AHEC, staff from other Georgia AHECs, Jeremy Whigham Design, the Georgia Department of Labor, Phyllis Johnson with the Georgia Department of Education, Ralph Morrison and the Georgia Health Information & Management Association Board of Directors, the American AHEC Spotlight ....................................................................5 Society for Cytotechnology, Sheri Porter with American Academy of Family Physicians News, and Dru Nadler Photography. We appreciate all of the Healthcare Trends ...............................................................6-7 expert readers listed below for reviewing and editing the content of each career page thereby enabling us to produce -

2019 Ambetter and Bluecross Hospital List.Xlsx
Ambetter and BlueCross Hospital List Most doctors that practice at an in‐network hospital will also be in‐network. One exception we know is Piedmont Atlanta Hospital. Piedmont Hospital is in the Ambetter netwok, but very few Piedmont Doctors are. It's always best to check with the insurance company's Search Tool or with the Provider directly. Hospital Name City Zip Ambetter BlueCross Emory University Hospital Atlanta 30322 X Emory University Hospital Midtown Atlanta 30308 X Emory Saint Joseph Atlanta 30342 X Emory Johns Creek Duluth 30097 X Emory Wesley Woods Hospital Atlanta 30329 X Northside Hospital Atlanta 30342 X Northside Hospital Cherokee Canton 30115 X Northside Hospital Forsyth Cumming 30041 X WellStar Atlanta Medical Center Atlanta 30312 X X WellStar Windy Hill Marietta 30067 X X WellStar Cobb Austell 30106 X X WellStar North Fulton Hospital Roswell 30076 X X WellStar Douglas Douglasville 30134 X Wellstar Kennestone Hospital Marietta 30060 X X WellStar Paulding Hiram 30141 X X WellStar Spalding Griffin 30224 X X WellStar Sylvan Grove Jackson 30233 X X WellStar Atlanta Medical Center South East Point 30344 X X Wellstar West Georgia Medical Center Lagrange 30240 X X DeKalb Medical Center Decatur 30033 X X Dekalb Medical Center at Hillendale Lithonia 30058 X X Shepherd Center Atlanta 30305 X X Gwinnett Medical Center Duluth Lawrenceville 30096 X X Gwinnett Medical Center Lawrenceville 30046 X X Childrens Healthcare of Atlanta Scottish Rite Atlanta 30342 X X Children Healthcare of Atl Hughes Spaulding Atlanta 30303 X X Childrens -
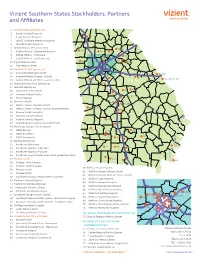
2018 Vizient Southern States Membership Map-Apr
Vizient Southern States Stockholders, Partners and Affiliates 1 Archbold Medical Center, Inc. 2 Brooks County Hospital 18 3 Grady General Hospital 19 16 4 John D. Archbold Memorial Hospital 5 Mitchell County Hospital 6 DeKalb Regional Health System 27, 28 28, 31 10 7 DeKalb Medical - Downtown Decatur 3433 35 30 8 DeKalb Medical - Hillandale 14, 63 33 30 9 DeKalb Medical - North Decatur 11 29 7 10 Floyd Medical Center 66 43 11 Polk Medical Center 12 Gwinnett Health System, Inc. 51, 52, 53 13 Glancy Rehabilitation Center 54, 56 69 14 Gwinnett Medical Center - Duluth 58 15 Gwinnett Medical Center - Lawrenceville 53, 55, 57, 59 70 GEORGIA 16 Hamilton Health Care System, Inc. 68 17 Houston Healthcare 25, 26 25 18 Houston Heart Institute 26 19 Houston Medical Center 24 24, 64 21, 22, 27 20 Perry Hospital 21 Navicent Health 23 17, 18, 19 22 Medical Center, Navicent Health 20, 21, 22 44, 45, 46 23 Medical Center of Peach County, Navicent Health 20 69 24 Monroe County Hospital 73 8, 9, 11, 61 25 Navicent Health Baldwin 23 26 Putnam General Hospital 40 68, 70 10 27 Rehabilitation Hospital, Navicent Health 75 28 Northeast Georgia Health System 29 NGMC Barrow 42 39 62 76 30 NGMC Braselton 66 31 NGMC Gainesville 37, 38 41 50, 52 6774 32 Northside Hospital 36 33 Northside Alpharetta 65 5 72 47, 48 34 Northside Hospital - Cherokee 51 41 34 35 50 35 Northside Hospital - Forsyth 40, 42, 43, 44 36 Northside Hospital Outpatient Center @ Meridian Mark 3 37 Phoebe Health 1, 4 3 260 49 38 Phoebe – Main Campus 6 48 46 39 Phoebe – North Campus 60 WellStar Health -

DPH Letterhead
GEORGIA DESIGNATED TRAUMA & SPECIALTY CARE CENTERS FACILITY CITY COUNTY NUMBER LEVEL I *Augusta University Medical Center Augusta RICHMOND 706-721-3153 *Grady Memorial Hospital Atlanta FULTON 404-616-6200 *Medical Center-Navicent Health Macon BIBB 478-633-1584 Memorial Health Univ. Medical Center Savannah CHATHAM 912-350-8861 Wellstar Atlanta Medical Center Atlanta FULTON 404-265-6577 (See Specialty Care Centers for Pediatric Center) LEVEL II *Doctors Hospital of Augusta Augusta RICHMOND 706-651-3232 Floyd Medical Center Rome FLOYD 706-509-5000 Gwinnett Medical Center Lawrenceville GWINNETT 678-312-4321 Hamilton Medical Center Dalton WHITFIELD 706-272-6150 *Northeast GA Medical Center Gainesville HALL 770-219-1200 Piedmont Athens Regional Athens CLARKE 706-475-3020 Piedmont Columbus Regional Columbus MUSCOGEE 706-571-1901 Wellstar Kennestone Hospital Marietta COBB 770-793-5000 *Wellstar North Fulton Hospital Roswell FULTON 770-751-2559 (See Specialty Care Centers for Pediatric Center) (*ACS Verified at level specified) Page 2 of 3 FACILITY CITY COUNTY NUMBER LEVEL III Cartersville Medical Center Cartersville BARTOW 770-382-1530 Crisp Regional Cordele CRISP 229-276-3100 Fairview Park Hospital Dublin LAURENS 478-275-2000 John D. Archbold Memorial Hospital Thomasville THOMAS 229-228-2834 Piedmont Walton Monroe WALTON 770-267-1781 Redmond Regional Medical Center Rome FLOYD 706-291-0291 Taylor Regional Hospital Hawkinsville PULASKI 478-783-0369 Wellstar Cobb Hospital Austell COBB 470-732-4000 LEVEL IV Appling Healthcare Baxley APPLING 912-367-9841 Effingham Health System Springfield EFFINGHAM 912-754-6451 Emanuel Medical Center Swainsboro EMANUEL 478-289-1100 Meadows Regional Medical Center Vidalia TOOMBS 912-535-5555 Morgan Memorial Hospital Madison MORGAN 706-752-2261 Polk Medical Center Cedartown POLK 770-748-2500 Winn Army Community Hospital Ft. -
The Changing Face Of
The Changing Face of HEALTHCARE THE 2006-2007 GEORGIA ALLIANCE OF COMMUNITY HOSPITALS YEAR IN REVIEW Georgia Alliance of Table of Contents Community Hospitals 2006-2007 Members Letter from the President ....................................................1 Archbold Medical Center Athens Regional Medical Center The Changing Face of Healthcare ..........2 Brooks County Hospital Clinch Memorial Hospital Georgia’s community hospitals at their best Colquitt Regional Medical Center Columbus Regional Healthcare System, Inc. Save Georgia Healthcare ................................8 DeKalb Medical Center Why Georgia needs to save, strengthen and streamline Dodge County Hospital its Certifi cate of Need (CON) program Donalsonville Hospital, Inc. Early Memorial Hospital Emanuel Medical Center 700 Reginas ................................................................14 Emory Healthcare Floyd Medical Center Upgrading Georgia’s trauma system could save Grady General Hospital hundreds of lives a year Grady Health System Gwinnett Health System, Inc. Gwinnett Medical Center - Duluth Remembering Robert A. Lipson, M.D. .....18 Hamilton Health Care System Houston Healthcare 28th Annual Conference Awards ........................................20 Jeff Davis Hospital Louis Smith Memorial Hospital Meadows Regional Medical Center Hospital of the Year .............................................................21 MCG Health Inc. Medical Center of Central Georgia Sponsors ...............................................................................22 Memorial -

Clicf SM+ GA 05-2009 Hosp.Sv
GEORGIA SUPERMED HOSPITAL NETWORK LIST ALPHABETIC LIST Anchor Hospital Bacon Cnty Hospital & Health System Central Georgia Rehab Hospital 5454 Yorktown Dr 302 S Wayne St 3351 Northside Dr Atlanta 30349 Alma 31510 Macon 31210 (770) 991-6044 (912) 632-8961 (478) 201-6500 Clayton County Bacon County Bibb County Appling Healthcare System Barrow Regional Medical Center Charlton Memorial Hospital 163 E Tollison St 316 N Broad St 1203 N 3rd St Baxley 31513 Winder 30680 Folkston 31537 (911) 367-9841 (770) 867-3400 (912) 496-2531 Appling County Barrow County Charlton County Appling Healthcare System Baxley BJC Medical Center Chatuge Regional Hospital 301 E Tollison St 70 Medical Center Dr 110 Main St Baxley 31513 Commerce 30529 Hiawassee 30546 (912) 367-9841 (706) 335-1000 (706) 896-2222 Appling County Jackson County Towns County Archbold Cardiac Rehab Center Bleckley Memorial Hospital Chestatee Regional Hospital 100 Mimosa Dr 145 E Peacock St 227 Mountain Dr Thomasville 31792 Cochran 31014 Dahlonega 30533 (229) 228-8053 (478) 934-6211 (706) 864-6136 Thomas County Bleckley County Lumpkin County 408 Peacock St Archbold Northside Cochran 31014 Child Healthcr Atlanta Egleston 401 Old Albany Rd 1405 Clifton Rd (478) 934-6211 Thomasville 31792 Atlanta 30322 (229) 228-8100 Bleckley County (770) 594-2940 Thomas County Dekalb County Brooks County Hospital 903 N Court St Archbold Northside Hospital Childrens Health Atl At Egleston 401 Old Northside Rd Quitman 31643 1405 Clifton Rd (912) 263-4171 Thomasville 31792 Atlanta 30322 (229) 228-8100 Brooks County