Treatment and Management of Venous Sinus Thrombosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Middle Cranial Fossa Sphenoidal Region Dural Arteriovenous Fistulas: Anatomic and Treatment Considerations
ORIGINAL RESEARCH INTERVENTIONAL Middle Cranial Fossa Sphenoidal Region Dural Arteriovenous Fistulas: Anatomic and Treatment Considerations Z.-S. Shi, J. Ziegler, L. Feng, N.R. Gonzalez, S. Tateshima, R. Jahan, N.A. Martin, F. Vin˜uela, and G.R. Duckwiler ABSTRACT BACKGROUND AND PURPOSE: DAVFs rarely involve the sphenoid wings and middle cranial fossa. We characterize the angiographic findings, treatment, and outcome of DAVFs within the sphenoid wings. MATERIALS AND METHODS: We reviewed the clinical and radiologic data of 11 patients with DAVFs within the sphenoid wing that were treated with an endovascular or with a combined endovascular and surgical approach. RESULTS: Nine patients presented with ocular symptoms and 1 patient had a temporal parenchymal hematoma. Angiograms showed that 5 DAVFs were located on the lesser wing of sphenoid bone, whereas the other 6 were on the greater wing of the sphenoid bone. Multiple branches of the ICA and ECA supplied the lesions in 7 patients. Four patients had cortical venous reflux and 7 patients had varices. Eight patients were treated with transarterial embolization using liquid embolic agents, while 3 patients were treated with transvenous embo- lization with coils or in combination with Onyx. Surgical disconnection of the cortical veins was performed in 2 patients with incompletely occluded DAVFs. Anatomic cure was achieved in all patients. Eight patients had angiographic and clinical follow-up and none had recurrence of their lesions. CONCLUSIONS: DAVFs may occur within the dura of the sphenoid wings and may often have a presentation similar to cavernous sinus DAVFs, but because of potential associations with the cerebral venous system, may pose a risk for intracranial hemorrhage. -

CHAPTER 8 Face, Scalp, Skull, Cranial Cavity, and Orbit
228 CHAPTER 8 Face, Scalp, Skull, Cranial Cavity, and Orbit MUSCLES OF FACIAL EXPRESSION Dural Venous Sinuses Not in the Subendocranial Occipitofrontalis Space More About the Epicranial Aponeurosis and the Cerebral Veins Subcutaneous Layer of the Scalp Emissary Veins Orbicularis Oculi CLINICAL SIGNIFICANCE OF EMISSARY VEINS Zygomaticus Major CAVERNOUS SINUS THROMBOSIS Orbicularis Oris Cranial Arachnoid and Pia Mentalis Vertebral Artery Within the Cranial Cavity Buccinator Internal Carotid Artery Within the Cranial Cavity Platysma Circle of Willis The Absence of Veins Accompanying the PAROTID GLAND Intracranial Parts of the Vertebral and Internal Carotid Arteries FACIAL ARTERY THE INTRACRANIAL PORTION OF THE TRANSVERSE FACIAL ARTERY TRIGEMINAL NERVE ( C.N. V) AND FACIAL VEIN MECKEL’S CAVE (CAVUM TRIGEMINALE) FACIAL NERVE ORBITAL CAVITY AND EYE EYELIDS Bony Orbit Conjunctival Sac Extraocular Fat and Fascia Eyelashes Anulus Tendineus and Compartmentalization of The Fibrous "Skeleton" of an Eyelid -- Composed the Superior Orbital Fissure of a Tarsus and an Orbital Septum Periorbita THE SKULL Muscles of the Oculomotor, Trochlear, and Development of the Neurocranium Abducens Somitomeres Cartilaginous Portion of the Neurocranium--the The Lateral, Superior, Inferior, and Medial Recti Cranial Base of the Eye Membranous Portion of the Neurocranium--Sides Superior Oblique and Top of the Braincase Levator Palpebrae Superioris SUTURAL FUSION, BOTH NORMAL AND OTHERWISE Inferior Oblique Development of the Face Actions and Functions of Extraocular Muscles Growth of Two Special Skull Structures--the Levator Palpebrae Superioris Mastoid Process and the Tympanic Bone Movements of the Eyeball Functions of the Recti and Obliques TEETH Ophthalmic Artery Ophthalmic Veins CRANIAL CAVITY Oculomotor Nerve – C.N. III Posterior Cranial Fossa CLINICAL CONSIDERATIONS Middle Cranial Fossa Trochlear Nerve – C.N. -

Dural Venous Channels: Hidden in Plain Sight–Reassessment of an Under-Recognized Entity
Published July 16, 2020 as 10.3174/ajnr.A6647 ORIGINAL RESEARCH INTERVENTIONAL Dural Venous Channels: Hidden in Plain Sight–Reassessment of an Under-Recognized Entity M. Shapiro, K. Srivatanakul, E. Raz, M. Litao, E. Nossek, and P.K. Nelson ABSTRACT BACKGROUND AND PURPOSE: Tentorial sinus venous channels within the tentorium cerebelli connecting various cerebellar and su- pratentorial veins, as well as the basal vein, to adjacent venous sinuses are a well-recognized entity. Also well-known are “dural lakes” at the vertex. However, the presence of similar channels in the supratentorial dura, serving as recipients of the Labbe, super- ficial temporal, and lateral and medial parieto-occipital veins, among others, appears to be underappreciated. Also under-recog- nized is the possible role of these channels in the angioarchitecture of certain high-grade dural fistulas. MATERIALS AND METHODS: A retrospective review of 100 consecutive angiographic studies was performed following identification of index cases to gather data on the angiographic and cross-sectional appearance, location, length, and other features. A review of 100 consecutive dural fistulas was also performed to identify those not directly involving a venous sinus. RESULTS: Supratentorial dural venous channels were found in 26% of angiograms. They have the same appearance as those in the tentorium cerebelli, a flattened, ovalized morphology owing to their course between 2 layers of the dura, in contradistinction to a rounded cross-section of cortical and bridging veins. They are best appreciated on angiography and volumetric postcontrast T1- weighted images. Ten dural fistulas not directly involving a venous sinus were identified, 6 tentorium cerebelli and 4 supratentorial. -

Human and Nonhuman Primate Meninges Harbor Lymphatic Vessels
SHORT REPORT Human and nonhuman primate meninges harbor lymphatic vessels that can be visualized noninvasively by MRI Martina Absinta1†, Seung-Kwon Ha1†, Govind Nair1, Pascal Sati1, Nicholas J Luciano1, Maryknoll Palisoc2, Antoine Louveau3, Kareem A Zaghloul4, Stefania Pittaluga2, Jonathan Kipnis3, Daniel S Reich1* 1Translational Neuroradiology Section, National Institute of Neurological Disorders and Stroke, National Institutes of Health, Bethesda, United States; 2Hematopathology Section, Laboratory of Pathology, National Cancer Institute, National Institutes of Health, Bethesda, United States; 3Center for Brain Immunology and Glia, Department of Neuroscience, School of Medicine, University of Virginia, Charlottesville, United States; 4Surgical Neurology Branch, National Institute of Neurological Disorders and Stroke, National Institutes of Health, Bethesda, United States Abstract Here, we report the existence of meningeal lymphatic vessels in human and nonhuman primates (common marmoset monkeys) and the feasibility of noninvasively imaging and mapping them in vivo with high-resolution, clinical MRI. On T2-FLAIR and T1-weighted black-blood imaging, lymphatic vessels enhance with gadobutrol, a gadolinium-based contrast agent with high propensity to extravasate across a permeable capillary endothelial barrier, but not with gadofosveset, a blood-pool contrast agent. The topography of these vessels, running alongside dural venous sinuses, recapitulates the meningeal lymphatic system of rodents. In primates, *For correspondence: meningeal -

The Development of Mammalian Dural Venous Sinuses with Especial Reference to the Post-Glenoid Vein
J. Anat. (1967), 102, 1, pp. 33-56 33 With 12 figures Printed in Great Britian The development of mammalian dural venous sinuses with especial reference to the post-glenoid vein H. BUTLER Department ofAnatomy, University of Saskatchewan, Saskatoon, Canada The intracranial venous outflow of mammals drains into both the internal and external jugular veins and the relative role of these two veins varies between different adult mammals as well as at different phases of embryonic and foetal life. In general, the primary head vein (consisting of venae capitis medialis and lateralis and their tributaries) gives rise to the dural venous sinuses which drain into the anterior cardinal vein (the future internal jugular vein). The external jugular veins appear as the face and jaws develop but, at all times, the two venous systems freely com- municate with each other. Morphologically, as shown by Sutton (1888), both the dural venous sinuses and the external jugular venous system are extracranial in so far as they are situated outside the dura mater. The chondrocranium and the dermocranium, however, develop in between the dural venous sinuses and the external jugular vein system (Butler, 1957). Thus, in the adult mammal, the bony skull wall separates the two venous systems, and therefore the dural venous sinuses are topographically intracranial whereas the external jugular venous system is extracranial. Furthermore the development of the skull localizes the connexions between the dural venous sinuses and the external jugular venous system to the various fontanelles and neuro-vascular foramina to form the emissary veins. The post-glenoid vein is one of the more important and controversial emissary veins since its presence or absence has been used in attempts to establish mammalian phylogenetic relationships (van Gelderen, 1925; Boyd, 1930). -

Dural Venous Sinuses Dr Nawal AL-Shannan Dural Venous Sinuses ( DVS )
Dural venous sinuses Dr Nawal AL-Shannan Dural venous sinuses ( DVS ) - Spaces between the endosteal and meningeal layers of the dura Features: 1. Lined by endothelium 2. No musculare tissue in the walls of the sinuses 3. Valueless 4.Connected to diploic veins and scalp veins by emmissary veins .Function: receive blood from the brain via cerebral veins and CSF through arachnoid villi Classification: 15 venous sinuses Paried venous sinuses Unpaired venous sinuses ( lateral in position) • * superior sagittal sinus • * cavernous sinuses • * inferior sagittal sinus • * superior petrosal sinuses • * occipital sinus • * inferior petrosal sinuses • * anterior intercavernous • * transverse sinuses • sinus * sigmoid sinuses • * posterior intercavernous • * spheno-parietal sinuses • sinus • * middle meningeal veins • * basilar plexuses of vein SUPERIOR SAGITTAL SINUS • Begins in front at the frontal crest • ends behind at the internal occipital protuberance diliated to form confluence of sinuses and venous lacunae • • The superior sagittal sinus receives the following : • 1- Superior cerebral veins • 2- dipolic veins • 3- Emissary veins • 4- arachnoid granulation • 5- meningeal veins Clinical significance • Infection from scalp, nasal cavity & diploic tissue • septic thrombosis • CSF absorption intra cranial thrombosis (ICT) • Inferior sagittal sinus - small channel occupy • lower free magin of falx cerebri ( post 2/3) - runs backward and • joins great cerebral vein at free margin of tentorium cerebelli to form straight sinus. • - receives cerebral -

The Routes of Intracranial Infections
University of Nebraska Medical Center DigitalCommons@UNMC MD Theses Special Collections 5-1-1934 The routes of intracranial infections E. Lloyd Wilbur University of Nebraska Medical Center This manuscript is historical in nature and may not reflect current medical research and practice. Search PubMed for current research. Follow this and additional works at: https://digitalcommons.unmc.edu/mdtheses Part of the Medical Education Commons Recommended Citation Wilbur, E. Lloyd, "The routes of intracranial infections" (1934). MD Theses. 364. https://digitalcommons.unmc.edu/mdtheses/364 This Thesis is brought to you for free and open access by the Special Collections at DigitalCommons@UNMC. It has been accepted for inclusion in MD Theses by an authorized administrator of DigitalCommons@UNMC. For more information, please contact [email protected]. THE ROUTES OF INTRACRANIAL INFECTIONS SENIOR THESIS 1934 E. Lloyd Wilbur April 13th, 1934 TABLE OF CONTENTS Section I Page Anatomical Considerations - - - - - - - - - - - - - - - 1 Section II The Routes of Infection - 31 Section III Case Histories -------------------- 40 Section IV SUmmary and Conclusions ---------------- 45 Bibliography --------------------- 50 PREFACE This thesis is written to discuss the anatomy of the skull and its contained structures in regard to intra oranial complioations due to preexisting routes. There is no attempt to discuss olinical medicine other than in a dir eot connection with these preexisting routes. In this way the dangerous potentialities of certain common infectious and pyogenio conditions may be more olearly understood and carefully watched for. To t~roughly comprehend these. dan gerous potentialities a knowledge of the anatomy of the skull and its ~ontents is essential. This thesis is written to mak~ this anatomy a basis of an understanding of certain types of intracranial pathology especially those arising as complications of previous pyogenic infeotious processes. -

Investigating the Mechanical and Structural Properties of the Superior Sagittal Sinus
IRC-20-64 IRCOBI conference 2020 Investigating the Mechanical and Structural Properties of the Superior Sagittal Sinus Darragh R. Walsh, Aisling M. Ross, David T. Newport, John J. E. Mulvihill Abstract The meninges, which are a composite tissue surrounding the brain, play an important role in the mechanopathology of traumatic brain injury. Studies have demonstrated that the meninges are pivotal in mitigating the damaging strains placed on the cortex from both physiological and pathophysiological head movement, which can occur during dynamic events such as traffic accidents. Conversely, structures such as the falx and tentorium have been shown to induce large deleterious strains within the brain. Understanding the mechanical behaviour of these tissues is important to predict computational model brain strains. This study provides the first biomechanical and structural evaluation of the structures anatomically tethered to the falx cerebri, the superior sagittal sinus. We utilise uniaxial tensile testing, digital image correlation analysis and scanning electron microscopy on porcine superior sagittal sinus tissue to show that these structures are mechanically stiffer (with elastic moduli ranging from 33 to 58 MPa) than the properties that are typically assigned to them in computational models of traumatic brain injury (elastic modulus of 31.5 MPa). This work has the potential to improve the biofidelity of traumatic brain injury finite element models, thus improving crash reconstruction and injury prediction efforts. Keywords Dura mater, finite element modelling, mechanical characterisation, TBI, venous sinuses. I. INTRODUCTION Traumatic brain injury (TBI) can be caused by rapid linear or rotational acceleration of the head experienced in vehicular collisions, explosions, falls, or assaults. -

Superficial Middle Cerebral Vein SUPERFICIAL CORTICAL VEINS O Superior Cerebral Veins
Cerebral Blood Circulation Khaleel Alyahya, PhD, MEd King Saud University School of Medicine @khaleelya OBJECTIVES At the end of the lecture, students should be able to: o List the cerebral arteries. o Describe the cerebral arterial supply regarding the origin, distribution and branches. o Describe the arterial Circle of Willis . o Describe the cerebral venous drainage and its termination. o Describe arterial & venous vascular disorders and their clinical manifestations. WATCH Review: THE BRAIN o Large mass of nervous tissue located in cranial cavity. o Has four major regions. Cerebrum (Cerebral hemispheres) Diencephalon: Thalamus, Hypothalamus, Subthalamus & Epithalamus Cerebellum Brainstem: Midbrain, Pons & Medulla oblongata Review: CEREBRUM o The largest part of the brain, and has two hemispheres. o The surface shows elevations called gyri, separated by depressions called sulci. o Each hemispheres divided into four lobes by deeper grooves. o Lobs are separated by deep grooves called fissures. Review: BLOOD VESSELS o Blood vessels are the part of the circulatory system that transports blood throughout the human body. o There are three major types of blood vessels: . Arteries, which carry the blood away from the heart. Capillaries, which enable the actual exchange of water and chemicals between the blood and the tissues. Veins, which carry blood from the capillaries back toward the heart. o The word vascular, meaning relating to the blood vessels, is derived from the Latin vas, meaning vessel. Avascular refers to being without (blood) vessels. Review: HISTOLOGY o The arteries and veins have three layers, but the middle layer is thicker in the arteries than it is in the veins: . -
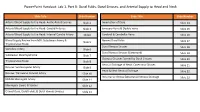
Powerpoint Handout: Lab 1, Part B: Dural Folds, Dural Sinuses, and Arterial Supply to Head and Neck
PowerPoint Handout: Lab 1, Part B: Dural Folds, Dural Sinuses, and Arterial Supply to Head and Neck Slide Title Slide Number Slide Title Slide Number Arterial Blood Supply to the Head: Aortic Arch Branches Slide 2 Innervation of Dura Slide 14 Arterial Blood Supply to the Head: Carotid Arteries Slide 3 Emissary Veins & Diploic Veins Slide 15 Arterial Blood Supply to the Head: Internal Carotid Artery Slide4 Cerebral & Cerebellar Veins Slide 16 Blood Supply Review from MSI: Subclavian Artery & Named Dural Folds Slide 5 Slide 17 Thyrocervical Trunk Dural Venous Sinuses Slide 18 Vertebral Artery Slide 6 Dural Venous Sinuses (Continued) Slide 19 Subclavian Steal Syndrome Slide 7 Osseous Grooves formed by Dural Sinuses Slide 20 Thyrocervical Trunk Slide 8 Venous Drainage of Head: Cavernous Sinuses Slide 21 Review: Suprascapular Artery Slide 9 Head & Neck Venous Drainage Slide 22 Review: Transverse Cervical Artery Slide 10 Intracranial Versus EXtracranial Venous Drainage Slide 23 Middle Meningeal Artery Slide 11 Meningeal Layers & Spaces Slide 12 Cranial Dura, Dural Folds, & Dural Venous Sinuses Slide 13 Arterial Blood Supply to the Head: Aortic Arch Branches The head and neck receive their blood supply from https://3d4medic.al/PXGmbxEt branches of the right and left common carotid and right and left subclavian arteries. • On the right side, the subclavian and common carotid arteries arise from the brachiocephalic trunk. • On the left side, these two arteries originate from the arch of the aorta. Arterial Blood Supply to the Head: Carotid Arteries On each side of the neck, the common carotid arteries ascend in the neck to the upper border of the thyroid cartilage (vertebral level C3/C4) where they divide into eXternal and internal carotid arteries at the carotid bifurcation. -

Lecture 4 Human Anatomy Second Stage احمد جسام النقيب د. the Meninges the Brain in the Skull Is Surro
Lecture 4 Human Anatomy second stage د. احمد جسام النقيب The Meninges The brain in the skull is surrounded by three protective membranes, or meninges: the dura mater, the arachnoid mater, and the pia mater. (The spinal cord in the vertebral column is also surrounded by three meninges) Dura Mater of the Brain The dura mater is conventionally described as two layers: the endosteal layer and the meningeal layer. These are closely united except along certain lines, where they separate to form venous sinuses. The endosteal layer is nothing more than the ordinary periosteum covering the inner surface of the skull bones. It does not extend through the foramen magnum to become continuous with the dura mater of the spinal cord. Around the margins of all the foramina in the skull, it becomes continuous with the periosteum on the outside of the skull bones. At the sutures, it is continuous with the sutural ligaments. It is most strongly adherent to the bones over the base of the skull. The meningeal layer is the dura mater proper. It is a dense, strong, fibrous membrane covering the brain and is continuous through the foramen magnum with the dura mater of the spinal cord. It provides tubular sheaths for the cranial nerves as the latter pass through the foramina in the skull. Outside the skull, the sheaths fuse with the epineurium of the nerves. The meningeal layer sends inward four septa that divide the cranial cavity into freely communicating spaces lodging the subdivisions of the brain. The function of these septa is to restrict the rotatory displacement of the brain. -

Reconstruction of the Superior Sagittal Sinus with Silicone Tubing
Neurosurg Focus 12 (6):Clinical Pearl 1, 2002, Click here to return to Table of Contents Reconstruction of the superior sagittal sinus with silicone tubing JINGJIAN MA, M.D., PH.D., TIANQIANG SONG, PH.D., WANG HU, PH.D., MICHAEL EDGAR MUHUMUZA, M.D., WENPING ZHAO, B.S., SHUYUAN YANG, PH.D., JINGWEN BAI, PH.D., AND HAIXIAN YANG, PH.D. Department of Neurosurgery, Tianjin Medical University, General Hospital; and The Center of Electron Microscopy, Tianjin Medical University, Tianjin, People’s Republic of China Object. The authors conducted a study to develop a safe and effective intracranial venous sinus reconstruction for extensive clinical use. Methods. After resecting the superior sagittal sinus (SSS), it was reconstructed in eight dogs by performing either a tube-insertion technique or end-to-end anastomosis procedure, in both of which a thin-walled silicone tube was used for repair. The patency of the SSS reconstruction was observed on digital subtraction angiography and transcranial Doppler ultrasonography, preoperatively and at 1, 2, 4, and 8 weeks postoperatively. Histological and ultrastructural changes were observed using light and electron microscopy. In five dogs the reconstructed SSS was patent, in one it was narrowed, in one it was completely occluded at the proximal site of the anastomosis, and one dog escaped from the laboratory 1 week postoperatively. The authors found no evidence of any additional neurological deficits, signs of toxicity, or side effects. Histological and ultrastructural studies generally showed vascular endothelial proliferation. No thrombosis occurred in the inner surface, at the site of anastomosis, or in the lumen of silicone tube nor in the sagittal sinus at up to 8 weeks postoperatively.