A New Approach to Atopic Dermatitis Control with Low-Concentration Propolis-Loaded Cold Cream
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Sanitization: Concentration, Temperature, and Exposure Time
Sanitization: Concentration, Temperature, and Exposure Time Did you know? According to the CDC, contaminated equipment is one of the top five risk factors that contribute to foodborne illnesses. Food contact surfaces in your establishment must be cleaned and sanitized. This can be done either by heating an object to a high enough temperature to kill harmful micro-organisms or it can be treated with a chemical sanitizing compound. 1. Heat Sanitization: Allowing a food contact surface to be exposed to high heat for a designated period of time will sanitize the surface. An acceptable method of hot water sanitizing is by utilizing the three compartment sink. The final step of the wash, rinse, and sanitizing procedure is immersion of the object in water with a temperature of at least 170°F for no less than 30 seconds. The most common method of hot water sanitizing takes place in the final rinse cycle of dishwashing machines. Water temperature must be at least 180°F, but not greater than 200°F. At temperatures greater than 200°F, water vaporizes into steam before sanitization can occur. It is important to note that the surface temperature of the object being sanitized must be at 160°F for a long enough time to kill the bacteria. 2. Chemical Sanitization: Sanitizing is also achieved through the use of chemical compounds capable of destroying disease causing bacteria. Common sanitizers are chlorine (bleach), iodine, and quaternary ammonium. Chemical sanitizers have found widespread acceptance in the food service industry. These compounds are regulated by the U.S. Environmental Protection Agency and consequently require labeling with the word “Sanitizer.” The labeling should also include what concentration to use, data on minimum effective uses and warnings of possible health hazards. -

Mucoadhesive Buccal Drug Delivery System: a Review
REVIEW ARTICLE Am. J. PharmTech Res. 2020; 10(02) ISSN: 2249-3387 Journal home page: http://www.ajptr.com/ Mucoadhesive Buccal Drug Delivery System: A Review Ashish B. Budhrani* , Ajay K. Shadija Datta Meghe College of Pharmacy, Salod (Hirapur), Wardha – 442001, Maharashtra, India. ABSTRACT Current innovation in pharmaceuticals determine the merits of mucoadhesive drug delivery system is particularly relevant than oral control release, for getting local systematic drugs distribution in GIT for a prolong period of time at a predetermined rate. The demerits relative with the oral drug delivery system is the extensive presystemic metabolism, degrade in acidic medium as a result insufficient absorption of the drugs. However parental drug delivery system may beat the downside related with oral drug delivery system but parental drug delivery system has significant expense, least patient compliance and supervision is required. By the buccal drug delivery system the medication are directly pass via into systemic circulation, easy administration without pain, brief enzymatic activity, less hepatic metabolism and excessive bioavailability. This review article is an outline of buccal dosage form, mechanism of mucoadhesion, in-vitro and in-vivo mucoadhesion testing technique. Keywords: Buccal drug delivery system, Mucoadhesive drug delivery system, Mucoadhesion, mucoadhesive polymers, Permeation enhancers, Bioadhesive polymers. *Corresponding Author Email: [email protected] Received 10 February 2020, Accepted 29 February 2020 Please cite this article as: Budhrani AB et al., Mucoadhesive Buccal Drug Delivery System: A Review . American Journal of PharmTech Research 2020. Budhrani et. al., Am. J. PharmTech Res. 2020; 10(02) ISSN: 2249-3387 INTRODUCTION Amongst the numerous routes of drug delivery system, oral drug delivery system is possibly the maximum preferred to the patient. -

An Overview On: Sublingual Route for Systemic Drug Delivery
International Journal of Research in Pharmaceutical and Biomedical Sciences ISSN: 2229-3701 __________________________________________Review Article An Overview on: Sublingual Route for Systemic Drug Delivery K. Patel Nibha1 and SS. Pancholi2* 1Department of Pharmaceutics, BITS Institute of Pharmacy, Gujarat Technological university, Varnama, Vadodara, Gujarat, India 2BITS Institute of Pharmacy, Gujarat Technological University, Varnama, Vadodara, Gujarat, India. __________________________________________________________________________________ ABSTRACT Oral mucosal drug delivery is an alternative and promising method of systemic drug delivery which offers several advantages. Sublingual literally meaning is ''under the tongue'', administrating substance via mouth in such a way that the substance is rapidly absorbed via blood vessels under tongue. Sublingual route offers advantages such as bypasses hepatic first pass metabolic process which gives better bioavailability, rapid onset of action, patient compliance , self-medicated. Dysphagia (difficulty in swallowing) is common among in all ages of people and more in pediatric, geriatric, psychiatric patients. In terms of permeability, sublingual area of oral cavity is more permeable than buccal area which is in turn is more permeable than palatal area. Different techniques are used to formulate the sublingual dosage forms. Sublingual drug administration is applied in field of cardiovascular drugs, steroids, enzymes and some barbiturates. This review highlights advantages, disadvantages, different sublingual formulation such as tablets and films, evaluation. Key Words: Sublingual delivery, techniques, improved bioavailability, evaluation. INTRODUCTION and direct access to systemic circulation, the oral Drugs have been applied to the mucosa for topical mucosal route is suitable for drugs, which are application for many years. However, recently susceptible to acid hydrolysis in the stomach or there has been interest in exploiting the oral cavity which are extensively metabolized in the liver. -

Lecture 3. the Basic Properties of the Natural Atmosphere 1. Composition
Lecture 3. The basic properties of the natural atmosphere Objectives: 1. Composition of air. 2. Pressure. 3. Temperature. 4. Density. 5. Concentration. Mole. Mixing ratio. 6. Gas laws. 7. Dry air and moist air. Readings: Turco: p.11-27, 38-43, 366-367, 490-492; Brimblecombe: p. 1-5 1. Composition of air. The word atmosphere derives from the Greek atmo (vapor) and spherios (sphere). The Earth’s atmosphere is a mixture of gases that we call air. Air usually contains a number of small particles (atmospheric aerosols), clouds of condensed water, and ice cloud. NOTE : The atmosphere is a thin veil of gases; if our planet were the size of an apple, its atmosphere would be thick as the apple peel. Some 80% of the mass of the atmosphere is within 10 km of the surface of the Earth, which has a diameter of about 12,742 km. The Earth’s atmosphere as a mixture of gases is characterized by pressure, temperature, and density which vary with altitude (will be discussed in Lecture 4). The atmosphere below about 100 km is called Homosphere. This part of the atmosphere consists of uniform mixtures of gases as illustrated in Table 3.1. 1 Table 3.1. The composition of air. Gases Fraction of air Constant gases Nitrogen, N2 78.08% Oxygen, O2 20.95% Argon, Ar 0.93% Neon, Ne 0.0018% Helium, He 0.0005% Krypton, Kr 0.00011% Xenon, Xe 0.000009% Variable gases Water vapor, H2O 4.0% (maximum, in the tropics) 0.00001% (minimum, at the South Pole) Carbon dioxide, CO2 0.0365% (increasing ~0.4% per year) Methane, CH4 ~0.00018% (increases due to agriculture) Hydrogen, H2 ~0.00006% Nitrous oxide, N2O ~0.00003% Carbon monoxide, CO ~0.000009% Ozone, O3 ~0.000001% - 0.0004% Fluorocarbon 12, CF2Cl2 ~0.00000005% Other gases 1% Oxygen 21% Nitrogen 78% 2 • Some gases in Table 3.1 are called constant gases because the ratio of the number of molecules for each gas and the total number of molecules of air do not change substantially from time to time or place to place. -

Carbon Monoxide Levels and Risks
Carbon Monoxide Levels and Risks CO Level Action CO Level Action 0.1 ppm Natural atmosphere level or clean air. 70-75 ppm Heart patients experience an increase in chest pain. Significant decrease in 1 ppm An increase of 1 ppm in the maximum dai- oxygen available to the myocardium/ ly one-hour exposure is associated with a heart (HbCO 10%). 0.96 percent increase in the risk of hospi- 100 ppm Headache, tiredness, dizziness, nausea talization from cardiovascular disease within 2 hrs of exposure. At 5 hrs, dam- among people over the age of 65. age to hearts and brains. (Lewey & Drabkin) (Circulation: Journal of the AHA, Sept, 2009) 200 ppm Healthy adults will have headache, nau- 3-7 ppm 6% increase in the rate of admission in sea at this level. hospitals of non-elderly for asthma. (L. Shep- pard et al.,Epidemiology, Jan 1999) NIOSH & OSHA recommend evacua- tion of the workplace at this level. 5-6 ppm Significant risk of low birth weight if exposed during last trimester - in a study 400 ppm Frontal headache within 1-2 hours—life of 125,573 pregnancies (Ritz & Yu, Environ. threatening within 3 hours. Health Perspectives, 1999). 500 ppm Concentration in a garage when a cold 9 ppm EPA and WHO maximum outdoor air lev- car is started in an open garage and el, all ages, (TWA, 8 hrs). Maximum allow- warmed up for 2 minutes. (Greiner, 1997) able indoor level (ASHRAE) 800 ppm Healthy adults will have nausea, dizzi- Lowest CO level producing significant ef- ness and convulsions within 45 fects on cardiac function (ST-segment minutes. -

CURRENT STATUS of BUCCAL DRUG DELIVERY SYSTEM: a REVIEW Srivastava Namita *, Monga Munish Garg R
Srivastava et al Journal of Drug Delivery & Therapeutics. 2015; 5(1):34-40 34 Available online on 15.01.2015 at http://jddtonline.info Journal of Drug Delivery and Therapeutics Open access to Pharmaceutical and Medical research © 2014, publisher and licensee JDDT, This is an Open Access article which permits unrestricted noncommercial use, provided the original work is properly cited REVIEW ARTICLE CURRENT STATUS OF BUCCAL DRUG DELIVERY SYSTEM: A REVIEW Srivastava Namita *, Monga Munish Garg R. V. Northland Institute, Chithera, Dadri, Gautama Buddha Nagar, Uttar Pradesh, India-203207 ABSTRACT Buccal mucosa is the preferred site for both systemic and local drug action. The mucosa has a rich blood supply and it relatively permeable. The buccal region of the oral cavity is an attractive target for administration of the drug of choice, particularly in overcoming deficiencies associated with the latter mode of administration. Problems such as first-pass metabolism and drug degradation in the gastrointestinal environment can be circumvented by administering the drug via the buccal route. Moreover, rapid onset of action can be achieved relative to the oral route and the formulation can be removed if therapy is required to be discontinued. It is also possible to administer drugs to patients who unconscious and less co-operative. In buccal drug delivery systems mucoadhesion is the key element so various mucoadhesive polymers have been utilized in different dosages form. Mucoadhesion may be defined as the process where polymers attach to biological substrate or a synthetic or natural macromolecule, to mucus or an epithelial surface. When the biological substrate is attached to a mucosal layer then this phenomenon is known as mucoadhesion. -
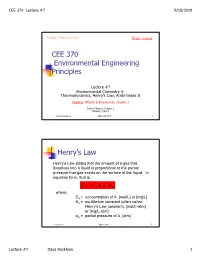
CEE 370 Environmental Engineering Principles Henry's
CEE 370 Lecture #7 9/18/2019 Updated: 18 September 2019 Print version CEE 370 Environmental Engineering Principles Lecture #7 Environmental Chemistry V: Thermodynamics, Henry’s Law, Acids-bases II Reading: Mihelcic & Zimmerman, Chapter 3 Davis & Masten, Chapter 2 Mihelcic, Chapt 3 David Reckhow CEE 370 L#7 1 Henry’s Law Henry's Law states that the amount of a gas that dissolves into a liquid is proportional to the partial pressure that gas exerts on the surface of the liquid. In equation form, that is: C AH = K p A where, CA = concentration of A, [mol/L] or [mg/L] KH = equilibrium constant (often called Henry's Law constant), [mol/L-atm] or [mg/L-atm] pA = partial pressure of A, [atm] David Reckhow CEE 370 L#7 2 Lecture #7 Dave Reckhow 1 CEE 370 Lecture #7 9/18/2019 Henry’s Law Constants Reaction Name Kh, mol/L-atm pKh = -log Kh -2 CO2(g) _ CO2(aq) Carbon 3.41 x 10 1.47 dioxide NH3(g) _ NH3(aq) Ammonia 57.6 -1.76 -1 H2S(g) _ H2S(aq) Hydrogen 1.02 x 10 0.99 sulfide -3 CH4(g) _ CH4(aq) Methane 1.50 x 10 2.82 -3 O2(g) _ O2(aq) Oxygen 1.26 x 10 2.90 David Reckhow CEE 370 L#7 3 Example: Solubility of O2 in Water Background Although the atmosphere we breathe is comprised of approximately 20.9 percent oxygen, oxygen is only slightly soluble in water. In addition, the solubility decreases as the temperature increases. -

Pressure Vs. Volume and Boyle's
Pressure vs. Volume and Boyle’s Law SCIENTIFIC Boyle’s Law Introduction In 1642 Evangelista Torricelli, who had worked as an assistant to Galileo, conducted a famous experiment demonstrating that the weight of air would support a column of mercury about 30 inches high in an inverted tube. Torricelli’s experiment provided the first measurement of the invisible pressure of air. Robert Boyle, a “skeptical chemist” working in England, was inspired by Torricelli’s experiment to measure the pressure of air when it was compressed or expanded. The results of Boyle’s experiments were published in 1662 and became essentially the first gas law—a mathematical equation describing the relationship between the volume and pressure of air. What is Boyle’s law and how can it be demonstrated? Concepts • Gas properties • Pressure • Boyle’s law • Kinetic-molecular theory Background Open end Robert Boyle built a simple apparatus to measure the relationship between the pressure and volume of air. The apparatus ∆h ∆h = 29.9 in. Hg consisted of a J-shaped glass tube that was Sealed end 1 sealed at one end and open to the atmosphere V2 = /2V1 Trapped air (V1) at the other end. A sample of air was trapped in the sealed end by pouring mercury into Mercury the tube (see Figure 1). In the beginning of (Hg) the experiment, the height of the mercury Figure 1. Figure 2. column was equal in the two sides of the tube. The pressure of the air trapped in the sealed end was equal to that of the surrounding air and equivalent to 29.9 inches (760 mm) of mercury. -

Worksheet 6 Solutions MATH 1A Fall 2015
Worksheet 6 Solutions MATH 1A Fall 2015 for 27 October 2015 These problems are taken from a set of science problems for calculus written by Jim Belk, avail- able at math.bard.edu/belk/writing.htm. If you’re looking for more practice on related rates or exponential growth, check it out! His problems are less terminally boring than the textbook’s problems. Exercise 6.1. In chemistry and physics, Boyle’s Law describes the relationship between the pressure and volume of a fixed quantity of gas maintained at a constant temperature. The law states that: PV = a constant where P is the pressure of the gas, and V is the volume. dP dV 1. Take the derivative of Boyle’s law to find an equation relating , , P, and V. dt dt 2. A sample of gas is placed in a cylindrical piston. At the beginning of the experiment, the gas occupies a volume of 250 cm3, and has a pressure of 100 kPa. The piston is slowly compressed, decreasing the volume of the gas at a rate of 50 cm3/min. How quickly will the pressure of the gas initially increase? Solution. For the first question, by taking an implicit derivative (using the product rule on the left hand side) we find dP dV V + P = 0. dt dt For the second question, we simply plug the values provided into the equation we’ve just found, dP (250) + (100)(50) = 0, dt dP and solve to find dt = 20 kPa/min. Exercise 6.2. In chemistry, the pH of a solution is defined by the formula pH = −0.4343 ln(a), where a is the hydrogen ion activity (a measure of the “effective concentration” of hydrogen ions). -

Influence of Hydrophobe Fraction Content on the Rheological Properties of Hydrosoluble Associative Polymers Obtained by Micellar Polymerization
http://www.e-polymers.org e-Polymers 2012, no. 009 ISSN 1618-7229 Influence of hydrophobe fraction content on the rheological properties of hydrosoluble associative polymers obtained by micellar polymerization Enrique J. Jiménez-Regalado,1* Elva B. Hernández-Flores2 1Centro de Investigación en Química Aplicada (CIQA) Blvd. Enrique Reyna #140, 25253, Saltillo, Coahuila, México; e-mail: [email protected] bCentro de Investigación en Química Aplicada (CIQA) Blvd. Enrique Reyna #140, 25253, Saltillo, Coahuila, México; e-mail: [email protected] (Received: 20 November, 2009; published: 22 January, 2012) Abstract: The synthesis, characterization and rheological properties in aqueous solutions of water-soluble associative polymers (AP’s) are reported. Polymer chains consisting of water-soluble polyacrylamides, hydrophobically modified with low amounts of N,N-dihexylacrylamide (1, 2, 3 and 4 mol%) were prepared via free radical micellar polymerization. The properties of these polymers, with respect to the concentration of hydrophobic groups, using steady-flow and oscillatory experiments were compared. An increase of relaxation time (TR) and modulus plateau (G0) was observed in all samples studied. Two different regimes can be clearly distinguished: a first unentangled regime where the viscosity increase rate strongly depends on hydrophobic content and a second entangled regime where the viscosity follows a scaling behavior of the polymer concentration with an exponent close to 4. Introduction Water-soluble polymers are of great interest from the scientific as well as the technological point of view. These polymers have been subjected to extensive research [1]. Water-soluble polymers are present in the composition of different types of industrial formulations as stabilizing, flocculants, absorbent, emulsifiers, thickeners, etc. -

The Small-Molecule BGP-15 Protects Against Heart Failure and Atrial fibrillation in Mice
ARTICLE Received 15 Sep 2014 | Accepted 30 Oct 2014 | Published 9 Dec 2014 DOI: 10.1038/ncomms6705 The small-molecule BGP-15 protects against heart failure and atrial fibrillation in mice Geeta Sapra1,*, Yow Keat Tham1,*, Nelly Cemerlang1, Aya Matsumoto1, Helen Kiriazis1, Bianca C. Bernardo1, Darren C. Henstridge1, Jenny Y.Y. Ooi1, Lynette Pretorius1,2, Esther J.H. Boey1, Lydia Lim1, Junichi Sadoshima3, Peter J. Meikle1, Natalie A. Mellet1, Elizabeth A. Woodcock1, Silvana Marasco4, Tomomi Ueyama5, Xiao-Jun Du1, Mark A. Febbraio1,2 & Julie R. McMullen1,2 Heart failure (HF) and atrial fibrillation (AF) share common risk factors, frequently coexist and are associated with high mortality. Treatment of HF with AF represents a major unmet need. Here we show that a small molecule, BGP-15, improves cardiac function and reduces arrhythmic episodes in two independent mouse models, which progressively develop HF and AF. In these models, BGP-15 treatment is associated with increased phosphorylation of the insulin-like growth factor 1 receptor (IGF1R), which is depressed in atrial tissue samples from patients with AF. Cardiac-specific IGF1R transgenic overexpression in mice with HF and AF recapitulates the protection observed with BGP-15. We further demonstrate that BGP-15 and IGF1R can provide protection independent of phosphoinositide 3-kinase-Akt and heat-shock protein 70; signalling mediators often defective in the aged and diseased heart. As BGP-15 is safe and well tolerated in humans, this study uncovers a potential therapeutic approach for HF and AF. 1 Baker IDI Heart and Diabetes Institute, PO Box 6492, Melbourne, Victoria 3004, Australia. 2 Monash University, Melbourne, Victoria 3800, Australia. -

Concentration and Fractionation of Hydrophobic Organic Acid Constituents from Natural Waters by Liquid Chromatography
Concentration and Fractionation of Hydrophobic Organic Acid Constituents from Natural Waters by Liquid Chromatography GEOLOGICAL SURVEY WATER-SUPPLY PAPER 1817-G Concentration and Fractionation of Hydrophobic Organic Acid Constituents from Natural Waters by Liquid Chromatography By E. M. THURMAN and R. L. MALCOLM ORGANIC SUBSTANCES INW^TER GEOLOGICAL SURVEY WATER-SUPPLY PAPER 1817-G UNITED STATES GOVERNMENT PRINTING OFFICE, WASHINGTON : 1979 UNITED STATES DEPARTMENT OF THE INTERIOR CECIL D. ANDRUS, Secretary GEOLOGICAL SURVEY H. William Menard, Director Library of Congress Cataloging in Publication Data Thurman, Earl M. Concentration and fractionation of hydrophobic organic acid constituents from natural waters by liquid chromatography. (Organic substances in water) (Geological Survey water-supply paper 1817-G) Bibliography: p. 15, 16. Supt.ofDocs.no.: I 19.13:1817-G 1. Acids, Organic. 2. Liquid chromatography. 3. Water chemistry. I. Malcolm, R. L., joint author. II. Title. III. Series. IV. Series: United States. Geological Survey. Water-supply paper ; 1817-G. TC801.U2 no. 1817-G [QD305.A2] 553'.7'0973s 79-607114 [628.1'61] For sale by the Superintendent of Documents, U. S. Government Printing Office Washington, D. C. 20402 Stock Number 024-001-03226-1 CONTENTS Page Abstract _____________________________________---_--___-___Gl Introduction ________-_____________________________________ 1 Acknowledgments _____________________________ 2 Experimental procedures ______________________________________ 2 Resin and column packings _________________________________