Mechanisms of Activation of Innate-Like Intraepithelial T Lymphocytes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Killer-Like Receptors and GPR56 Progressive Expression Defines Cytokine Production of Human CD4+ Memory T Cells
ARTICLE https://doi.org/10.1038/s41467-019-10018-1 OPEN Killer-like receptors and GPR56 progressive expression defines cytokine production of human CD4+ memory T cells Kim-Long Truong1,7, Stephan Schlickeiser1,2,7, Katrin Vogt1, David Boës1, Katarina Stanko1, Christine Appelt1, Mathias Streitz1, Gerald Grütz1,2, Nadja Stobutzki1, Christian Meisel1, Christina Iwert1, Stefan Tomiuk3, Julia K. Polansky2,4, Andreas Pascher5, Nina Babel2,6, Ulrik Stervbo 6, Igor Sauer 5, Undine Gerlach5 & Birgit Sawitzki1,2 1234567890():,; All memory T cells mount an accelerated response on antigen reencounter, but significant functional heterogeneity is present within the respective memory T-cell subsets as defined by CCR7 and CD45RA expression, thereby warranting further stratification. Here we show that several surface markers, including KLRB1, KLRG1, GPR56, and KLRF1, help define low, high, or exhausted cytokine producers within human peripheral and intrahepatic CD4+ memory T-cell populations. Highest simultaneous production of TNF and IFN-γ is observed in KLRB1+KLRG1+GPR56+ CD4 T cells. By contrast, KLRF1 expression is associated with T-cell exhaustion and reduced TNF/IFN-γ production. Lastly, TCRβ repertoire analysis and in vitro differentiation support a regulated, progressive expression for these markers during CD4+ memory T-cell differentiation. Our results thus help refine the classification of human memory T cells to provide insights on inflammatory disease progression and immunotherapy development. 1 Institute of Medical Immunology, Charité – Universitätsmedizin Berlin, Freie Universität Berlin, Humboldt-Universität zu Berlin and Berlin Institute of Health, 13353 Berlin, Germany. 2 Berlin-Brandenburg Center for Regenerative Therapies (BCRT), Charité – Universitätsmedizin Berlin, 13353 Berlin, Germany. 3 Milteny Biotec GmbH, 51429 Bergisch Gladbach, Germany. -

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -
NK Cell Memory to Cytomegalovirus: Implications for Vaccine Development
Review NK Cell Memory to Cytomegalovirus: Implications for Vaccine Development Calum Forrest 1 , Ariane Gomes 1 , Matthew Reeves 1,* and Victoria Male 2,* 1 Institute of Immunity & Transplantation, UCL, Royal Free Campus, London NW3 2PF, UK; [email protected] (C.F.); [email protected] (A.G.) 2 Department of Metabolism, Digestion and Reproduction, Imperial College London, Chelsea and Westminster Campus, London SW10 9NH, UK * Correspondence: [email protected] (M.R.); [email protected] (V.M.) Received: 24 June 2020; Accepted: 15 July 2020; Published: 20 July 2020 Abstract: Natural killer (NK) cells are innate lymphoid cells that recognize and eliminate virally-infected and cancerous cells. Members of the innate immune system are not usually considered to mediate immune memory, but over the past decade evidence has emerged that NK cells can do this in several contexts. Of these, the best understood and most widely accepted is the response to cytomegaloviruses, with strong evidence for memory to murine cytomegalovirus (MCMV) and several lines of evidence suggesting that the same is likely to be true of human cytomegalovirus (HCMV). The importance of NK cells in the context of HCMV infection is underscored by the armory of NK immune evasion genes encoded by HCMV aimed at subverting the NK cell immune response. As such, ongoing studies that have utilized HCMV to investigate NK cell diversity and function have proven instructive. Here, we discuss our current understanding of NK cell memory to viral infection with a focus on the response to cytomegaloviruses. We will then discuss the implications that this will have for the development of a vaccine against HCMV with particular emphasis on how a strategy that can harness the innate immune system and NK cells could be crucial for the development of a vaccine against this high-priority pathogen. -

Genitourinary Pathology (Including Renal Tumors)
LABORATORY INVESTIGATION THE BASIC AND TRANSLATIONAL PATHOLOGY RESEARCH JOURNAL LI VOLUME 99 | SUPPLEMENT 1 | MARCH 2019 2019 ABSTRACTS GENITOURINARY PATHOLOGY (INCLUDING RENAL TUMORS) (776-992) MARCH 16-21, 2019 PLATF OR M & 2 01 9 ABSTRACTS P OSTER PRESENTATI ONS EDUCATI ON C O M MITTEE Jason L. Hornick , C h air Ja mes R. Cook R h o n d a K. Y a nti s s, Chair, Abstract Revie w Board S ar a h M. Dr y and Assign ment Co m mittee Willi a m C. F a q ui n Laura W. La mps , Chair, C ME Subco m mittee C ar ol F. F ar v er St e v e n D. Billi n g s , Interactive Microscopy Subco m mittee Y uri F e d ori w Shree G. Shar ma , Infor matics Subco m mittee Meera R. Ha meed R aj a R. S e et h al a , Short Course Coordinator Mi c h ell e S. Hir s c h Il a n W ei nr e b , Subco m mittee for Unique Live Course Offerings Laksh mi Priya Kunju D a vi d B. K a mi n s k y ( Ex- Of ici o) A n n a M ari e M ulli g a n Aleodor ( Doru) Andea Ri s h P ai Zubair Baloch Vi nita Parkas h Olca Bast urk A nil P ar w a ni Gregory R. Bean , Pat h ol o gist-i n- Trai ni n g D e e p a P atil D a ni el J. -
Platelets Impair Natural Killer Cell Reactivity and Function in Endometriosis Through Multiple Mechanisms
Human Reproduction, Vol.32, No.4 pp. 794–810, 2017 Advanced Access publication on February 9, 2017 doi:10.1093/humrep/dex014 ORIGINAL ARTICLE Gynaecology Platelets impair natural killer cell reactivity and function in endometriosis through multiple mechanisms Yanbo Du, Xishi Liu, and Sun-Wei Guo* Shanghai Obstetrics and Gynecology Hospital, Fudan University Shanghai College of Medicine, 419 Fangxie Road, Shanghai 200011, China *Correspondence Address. Shanghai Obstetrics and Gynecology Hospital, Fudan University Shanghai College of Medicine, Shanghai 200011, China. Fax: 86-21-6345-5090; E-mail: [email protected] Submitted on October 28, 2016; resubmitted on December 27, 2016; accepted on January 13, 2017 STUDY QUESTION: Do platelets have any role in the reduced cytotoxicity of natural killer (NK) cells in endometriosis? SUMMARY ANSWER: Platelets impair NK cell reactivity and function in endometriosis through multiple mechanisms. WHAT IS KNOWN ALREADY: Platelets play an important role in the development of endometriosis, and platelet-derived transforming growth factor-β1 (TGF-β1) suppresses the expression of NK Group 2, Member D (NKG2D) on NK cells, resulting in reduced cytotoxicity in women with endometriosis. STUDY DESIGN SIZE, DURATION: Experiments on mice with induced endometriosis in which either platelets, NK cells or both were depleted and controls (none depleted). In vitro experiments with NK cells, platelets and, as target cells, endometriotic epithelial cell and endo- metrial stromal cell lines. PARTICIPANTS/MATERIALS SETTING METHODS: Immunohistochemistry analysis of ectopic endometrial tissues from mice with induced endometriosis receiving either platelet depletion (PD), NK cell depletion, or both or none. Immunofluorescence, flow cytometry and gene expression analysis for major histocompatibility complex class I (MHC-I) expression in target cells. -

Deciphering the Transcriptional Switches of Innate Lymphoid Cell Programming: the Right Factors at the Right Time
Genes and Immunity (2015) 16, 177–186 © 2015 Macmillan Publishers Limited All rights reserved 1466-4879/15 www.nature.com/gene REVIEW Deciphering the transcriptional switches of innate lymphoid cell programming: the right factors at the right time AWY Lim and ANJ McKenzie Innate lymphoid cells (ILCs) are increasingly recognised as an innate immune counterpart of adaptive T-helper (TH) cells. In addition to their similar effector cytokine production, there is a strong parallel between the transcription factors that control the differentiation of TH1, TH2 and TH17 cells and ILC groups 1, 2 and 3, respectively. Here, we review the transcriptional circuit that specifies the development of a common ILC progenitor and its subsequent programming into distinct ILC groups. Notch, GATA-3 (GATA-binding protein 3), Nfil3 (nuclear factor interleukin-3) and Id2 (inhibitor of DNA-binding 2) are identified as early factors that suppress B- and T-cell potentials and are turned on in favour of ILC commitment. Natural killer cells, which are the cytotoxic ILCs, develop along a pathway distinct from the rest of the helper-like ILCs that are derived from a common progenitor to all helper-like ILCs (CHILPs). PLZF− (promyelocytic leukaemia zinc-finger) CHILPs give rise to lymphoid tissue inducer cells, while PLZF+ CHILPs have multilineage potential and could give rise to ILCs 1, 2 and 3. Such lineage specificity is dictated by the controlled expression of T-bet (T-box expressed in T cells), RORα (retinoic acid receptor-related orphan nuclear receptor-α), RORγt (retinoic acid receptor- related orphan nuclear receptor-γt) and AHR (aryl hydrocarbon receptor). -

Monoclonal Antibody to CD161 / KLRB1 - Purified
OriGene Technologies, Inc. OriGene Technologies GmbH 9620 Medical Center Drive, Ste 200 Schillerstr. 5 Rockville, MD 20850 32052 Herford UNITED STATES GERMANY Phone: +1-888-267-4436 Phone: +49-5221-34606-0 Fax: +1-301-340-8606 Fax: +49-5221-34606-11 [email protected] [email protected] SM1611PT Monoclonal Antibody to CD161 / KLRB1 - Purified Alternate names: C-type lectin domain family 5 member B, CLEC5B, HNKR-P1a, Killer cell lectin-like receptor subfamily B member 1, NKRP1A, Natural killer cell surface protein P1A Quantity: 25 µg Concentration: 1.0 mg/ml Background: Natural killer (NK) cells are lymphocytes that mediate cytotoxicity and secrete cytokines after immune stimulation. Several genes of the C-type lectin superfamily, including the rodent NKRP1 family of glycoproteins, are expressed by NK cells and may be involved in the regulation of NK cell function. The KLRB1 (CD161) protein contains an extracellular domain with several motifs characteristic of C type lectins, a transmembrane domain, and a cytoplasmic domain. The KLRB1 protein is classified as a type II membrane protein because it has an external C terminus. In mouse the NKRP1 family has three members, NKRP1A, B and C, whilst in human only one member has been identified. The human protein has received the designation CD161, and the mouse proteins have been referred to as CD161a, b and c. Engagement of CD161c has been reported to have activating function in NK cells, whilst engagement of CD161b is inhibitory. CD161 is expressed by almost all NK cells and with a small subset of CD3+ve T cells. -
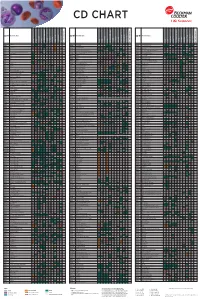
Flow Reagents Single Color Antibodies CD Chart
CD CHART CD N° Alternative Name CD N° Alternative Name CD N° Alternative Name Beckman Coulter Clone Beckman Coulter Clone Beckman Coulter Clone T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells CD1a T6, R4, HTA1 Act p n n p n n S l CD99 MIC2 gene product, E2 p p p CD223 LAG-3 (Lymphocyte activation gene 3) Act n Act p n CD1b R1 Act p n n p n n S CD99R restricted CD99 p p CD224 GGT (γ-glutamyl transferase) p p p p p p CD1c R7, M241 Act S n n p n n S l CD100 SEMA4D (semaphorin 4D) p Low p p p n n CD225 Leu13, interferon induced transmembrane protein 1 (IFITM1). p p p p p CD1d R3 Act S n n Low n n S Intest CD101 V7, P126 Act n p n p n n p CD226 DNAM-1, PTA-1 Act n Act Act Act n p n CD1e R2 n n n n S CD102 ICAM-2 (intercellular adhesion molecule-2) p p n p Folli p CD227 MUC1, mucin 1, episialin, PUM, PEM, EMA, DF3, H23 Act p CD2 T11; Tp50; sheep red blood cell (SRBC) receptor; LFA-2 p S n p n n l CD103 HML-1 (human mucosal lymphocytes antigen 1), integrin aE chain S n n n n n n n l CD228 Melanotransferrin (MT), p97 p p CD3 T3, CD3 complex p n n n n n n n n n l CD104 integrin b4 chain; TSP-1180 n n n n n n n p p CD229 Ly9, T-lymphocyte surface antigen p p n p n -

CD29 Identifies IFN-Γ–Producing Human CD8+ T Cells With
+ CD29 identifies IFN-γ–producing human CD8 T cells with an increased cytotoxic potential Benoît P. Nicoleta,b, Aurélie Guislaina,b, Floris P. J. van Alphenc, Raquel Gomez-Eerlandd, Ton N. M. Schumacherd, Maartje van den Biggelaarc,e, and Monika C. Wolkersa,b,1 aDepartment of Hematopoiesis, Sanquin Research, 1066 CX Amsterdam, The Netherlands; bLandsteiner Laboratory, Oncode Institute, Amsterdam University Medical Center, University of Amsterdam, 1105 AZ Amsterdam, The Netherlands; cDepartment of Research Facilities, Sanquin Research, 1066 CX Amsterdam, The Netherlands; dDivision of Molecular Oncology and Immunology, Oncode Institute, The Netherlands Cancer Institute, 1066 CX Amsterdam, The Netherlands; and eDepartment of Molecular and Cellular Haemostasis, Sanquin Research, 1066 CX Amsterdam, The Netherlands Edited by Anjana Rao, La Jolla Institute for Allergy and Immunology, La Jolla, CA, and approved February 12, 2020 (received for review August 12, 2019) Cytotoxic CD8+ T cells can effectively kill target cells by producing therefore developed a protocol that allowed for efficient iso- cytokines, chemokines, and granzymes. Expression of these effector lation of RNA and protein from fluorescence-activated cell molecules is however highly divergent, and tools that identify and sorting (FACS)-sorted fixed T cells after intracellular cytokine + preselect CD8 T cells with a cytotoxic expression profile are lacking. staining. With this top-down approach, we performed an un- + Human CD8 T cells can be divided into IFN-γ– and IL-2–producing biased RNA-sequencing (RNA-seq) and mass spectrometry cells. Unbiased transcriptomics and proteomics analysis on cytokine- γ– – + + (MS) analyses on IFN- and IL-2 producing primary human producing fixed CD8 T cells revealed that IL-2 cells produce helper + + + CD8 Tcells. -

A Novel CD4+ CTL Subtype Characterized by Chemotaxis and Inflammation Is Involved in the Pathogenesis of Graves’ Orbitopa
Cellular & Molecular Immunology www.nature.com/cmi ARTICLE OPEN A novel CD4+ CTL subtype characterized by chemotaxis and inflammation is involved in the pathogenesis of Graves’ orbitopathy Yue Wang1,2,3,4, Ziyi Chen 1, Tingjie Wang1,2, Hui Guo1, Yufeng Liu2,3,5, Ningxin Dang3, Shiqian Hu1, Liping Wu1, Chengsheng Zhang4,6,KaiYe2,3,7 and Bingyin Shi1 Graves’ orbitopathy (GO), the most severe manifestation of Graves’ hyperthyroidism (GH), is an autoimmune-mediated inflammatory disorder, and treatments often exhibit a low efficacy. CD4+ T cells have been reported to play vital roles in GO progression. To explore the pathogenic CD4+ T cell types that drive GO progression, we applied single-cell RNA sequencing (scRNA-Seq), T cell receptor sequencing (TCR-Seq), flow cytometry, immunofluorescence and mixed lymphocyte reaction (MLR) assays to evaluate CD4+ T cells from GO and GH patients. scRNA-Seq revealed the novel GO-specific cell type CD4+ cytotoxic T lymphocytes (CTLs), which are characterized by chemotactic and inflammatory features. The clonal expansion of this CD4+ CTL population, as demonstrated by TCR-Seq, along with their strong cytotoxic response to autoantigens, localization in orbital sites, and potential relationship with disease relapse provide strong evidence for the pathogenic roles of GZMB and IFN-γ-secreting CD4+ CTLs in GO. Therefore, cytotoxic pathways may become potential therapeutic targets for GO. 1234567890();,: Keywords: Graves’ orbitopathy; single-cell RNA sequencing; CD4+ cytotoxic T lymphocytes Cellular & Molecular Immunology -

Supplementary Material DNA Methylation in Inflammatory Pathways Modifies the Association Between BMI and Adult-Onset Non- Atopic
Supplementary Material DNA Methylation in Inflammatory Pathways Modifies the Association between BMI and Adult-Onset Non- Atopic Asthma Ayoung Jeong 1,2, Medea Imboden 1,2, Akram Ghantous 3, Alexei Novoloaca 3, Anne-Elie Carsin 4,5,6, Manolis Kogevinas 4,5,6, Christian Schindler 1,2, Gianfranco Lovison 7, Zdenko Herceg 3, Cyrille Cuenin 3, Roel Vermeulen 8, Deborah Jarvis 9, André F. S. Amaral 9, Florian Kronenberg 10, Paolo Vineis 11,12 and Nicole Probst-Hensch 1,2,* 1 Swiss Tropical and Public Health Institute, 4051 Basel, Switzerland; [email protected] (A.J.); [email protected] (M.I.); [email protected] (C.S.) 2 Department of Public Health, University of Basel, 4001 Basel, Switzerland 3 International Agency for Research on Cancer, 69372 Lyon, France; [email protected] (A.G.); [email protected] (A.N.); [email protected] (Z.H.); [email protected] (C.C.) 4 ISGlobal, Barcelona Institute for Global Health, 08003 Barcelona, Spain; [email protected] (A.-E.C.); [email protected] (M.K.) 5 Universitat Pompeu Fabra (UPF), 08002 Barcelona, Spain 6 CIBER Epidemiología y Salud Pública (CIBERESP), 08005 Barcelona, Spain 7 Department of Economics, Business and Statistics, University of Palermo, 90128 Palermo, Italy; [email protected] 8 Environmental Epidemiology Division, Utrecht University, Institute for Risk Assessment Sciences, 3584CM Utrecht, Netherlands; [email protected] 9 Population Health and Occupational Disease, National Heart and Lung Institute, Imperial College, SW3 6LR London, UK; [email protected] (D.J.); [email protected] (A.F.S.A.) 10 Division of Genetic Epidemiology, Medical University of Innsbruck, 6020 Innsbruck, Austria; [email protected] 11 MRC-PHE Centre for Environment and Health, School of Public Health, Imperial College London, W2 1PG London, UK; [email protected] 12 Italian Institute for Genomic Medicine (IIGM), 10126 Turin, Italy * Correspondence: [email protected]; Tel.: +41-61-284-8378 Int. -

Single-Cell Analysis of Crohn's Disease Lesions Identifies
bioRxiv preprint doi: https://doi.org/10.1101/503102; this version posted December 20, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Single-cell analysis of Crohn’s disease lesions identifies a pathogenic cellular module associated with resistance to anti-TNF therapy JC Martin1,2,3, G Boschetti1,2,3, C Chang1,2,3, R Ungaro4, M Giri5, LS Chuang5, S Nayar5, A Greenstein6, M. Dubinsky7, L Walker1,2,5,8, A Leader1,2,3, JS Fine9, CE Whitehurst9, L Mbow9, S Kugathasan10, L.A. Denson11, J.Hyams12, JR Friedman13, P Desai13, HM Ko14, I Laface1,2,8, Guray Akturk1,2,8, EE Schadt15,16, S Gnjatic1,2,8, A Rahman1,2,5,8, , M Merad1,2,3,8,17,18*, JH Cho5,17,*, E Kenigsberg1,15,16,17* 1 Precision Immunology Institute, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA. 2 Tisch Cancer Institute, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA. 3 Department of Oncological Sciences, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA. 4 The Dr. Henry D. Janowitz Division of Gastroenterology, Icahn School of Medicine at Mount Sinai, New York City, NY 10029, USA. 5 Charles Bronfman Institute for Personalized Medicine, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA. 6 Department of Colorectal Surgery, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA 7 Department of Pediatrics, Susan and Leonard Feinstein IBD Clinical Center, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA.