Immune Checkpoint Blockade for Metastatic Uveal Melanoma: Patterns of Response and Survival According to the Presence of Hepatic and Extrahepatic Metastasis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Short Curriculum Vitae (2-Page Resume) Personal Information Family Name, First Name: Benzmüller, Christoph Ewald Title(S): Prof
Short Curriculum Vitae (2-Page Resume) Personal information Family name, First name: Benzmüller, Christoph Ewald Title(s): Prof. Dr.-Ing. habil. ORCID ID: orcid.org/0000-0002-3392-3093 Date of birth: 8 September 1968 Nationality: German Education 07/1999–07/2007 Habil., Dep. of Computer Science, Saarland University, Saarbrücken, DE 04/1995–07/1999 Dr.-Ing., Dep. of Computer Science, Saarland University, DE 10/1989–04/1995 Dipl.-Inform. Dep. of Computer Science, Saarland University, DE Current and upcoming positions 07/2018–06/2019 Professor, Mathematics and Computer Science, FU Berlin, DE 03/2017–ongoing Visiting Scholar and Scientific Collaborator, FSTC, University of Luxembourg, LU 02/2012–ongoing Privatdozent in Mathematics and Computer Science, FU Berlin, DE 08/2007–ongoing Privatdozent in Computer Science, Saarland University, DE Previous positions (selection) 2015–2016 Visiting Scholar, CSLI/Cordula Hall, Stanford University, CA, US 2012–2017 Heisenberg Fellow, FU Berlin, DE 2008–2011 Senior Researcher, DFG research grant ArticulateSoftware, Angwin, CA, US 2008–2009 Full Professor (tenured) for Formal Methods and AI, Intl. University in Germany, Bruchsal, DE 2006–2007 Senior Research Fellow, Computer Science, University of Cambridge, GB 2004–2008 Associate Prof. (C2), Dep. of Computer Science, Saarland University, DE 2001–2004 Senior Researcher (C1), Dep. of Computer Science, Saarland University, DE 2000–2001 PostDoc, The Universities of Birmingham and Edinburgh, GB Fellowships, awards and honors (selection) 2012–2017 Heisenberg Fellowship, German National Research Foundation (DFG) 2015/2016 Central teaching award of FU Berlin for lecture on Computational Metaphysics 2014 Nominated for Amalia Preis für Neues Denken, Weimar 2012–2017 Member of the Berlin Mathematical School 2010 World champion in higher-order automated theorem proving with LEO-II prover 1996–1998 Ph.D. -

9 March 2012 Biological Barriers
th 9 International Conference and Workshop on Biological Barriers – in vitro and in silico Tools for Drug Delivery and Nanosafety Research 29 February - 9 March 2012 Saarland University21 March – 1 April 2010 Saarbrücken,Saarland Germany University Saarbrücken, Germany Programme Chairs and Organisers: Prof. Dr. Claus-Michael Lehr, Prof. Dr. Ulrich F. Schäfer, Jun. Prof. Dr. Marc Schneider, Dr. Nicole Daum http://www.uni-saarland.de/biobarriers2012 Helmholtz Institute for Pharmaceutical Research Saarland 9th International Conference and Workshop on Biological Barriers – in vitro and in silico Tools for Drug Delivery and Nanosafety Research 29 February – 9 March 2012 at Saarland University, Germany Wednesday, 29 February 2012 7:30 Registration open 8:30 Relevance of in vitro studies for dermatological research Howard Maibach, University of California, USA 9:00 Welcome address Volker Linneweber, President of Saarland University Seminar 1: Skin Barrier Reaching the Immune System via the Skin: New Vaccines and Adjuvants - Challenges and Opportunities Chairs: Marc Schneider, Saarland University Steffi Hansen, Helmholtz Institute for Pharmaceutical Research Saarland 9:15 Transdermal hyposensitation Thomas Kündig, University Hospital Zurich, Switzerland 9:45 Vaccine delivery and the role of new adjuvants Carlos Guzman, Helmholtz Centre for Infection Research, Germany Thomas Ebensen, Helmholtz Centre for Infection Research, Germany 10:15 Vaccine delivery in the skin Véronique Préat, University of Leuven, Belgium 10:45 Preclinical model and clinical -

Curriculum Vitae
Curriculum Vitae Name Priv.-Doz. Dr.-Ing. Christoph Ewald Benzmuller¨ Academic Degrees Habilitation, Doctorate, Diploma Nationality German E-mail, Homepage [email protected], http://christoph-benzmueller.de Work Address Facult´edes Sciences, de la Technologie et de la Communication, 2, Avenue de l'Universit´e,L-4365 Esch-sur-Alzette, Luxembourg Education Habilitation, computer science, Theorem Proving in Classical Higher-Order Logic, Saarland University 2007 PhD (Dr.), computer science, Equality and Extensionality in Automated Higher-Order Theorem 1999 Proving (advisors: J. Siekmann, F. Pfenning, M. Kohlhase), Saarland University Diploma, computer science (and economics), Eine Fallstudie zur Spezifikation von Systemanforderungen 1995 in der Spezifikationssprache OBSCURE (advisors: J. Loeckx, K. Gersonde), Saarland University Abitur (A-levels), Auguste Victoria Gymnasium, Trier, Germany 1988 Present/Recent Affiliations University of Luxemburg, visiting scholar 3/2017{9/2017 Freie Universit¨at Berlin, Privatdozent, venia legendi in Mathematics and Computer Science 2012{ Stanford University, CSLI/Cordula Hall (Philosophy), CA, USA, visiting scholar 10/2015{06/2016 Saarland University, Privatdozent, venia legendi in Computer Science 2007{ Past Affiliations and Appointments Articulate Software, Angwin, CA, USA, senior researcher, DFG research grant 2008{2011 Intl. University in Germany, Bruchsal, full professor for Artificial Intelligence (AI) & Formal Methods 2008{2009 The University of Cambridge, UK, senior research fellow, Computer Science -

Welcome to Saarbrücken MESSAGE from the TEAM
Welcome to Saarbrücken MESSAGE FROM THE TEAM Dear student, This booklet, like everything we do, is to make you feel welcome in the beautiful small city of Saarbrücken. When we - almost all of us - did an Erasmus, we needed help from experienced students and wanted friends who felt as new as we did. When we returned to Germany, we wanted to keep up the international spirit and give back what we experienced abroad. We consist of both German and international students who help you step into the rich, new culture with people who enjoy embracing and sharing their roots. We have a wide range of goals to make your stay unforgettable: We aim to help you build a strong social network, make friends from all over the world as well as different fields of studies etc. We want to create an international environment of exchanging backgrounds by bringing together local and international students. We work together to host a wide range of events. From classy evenings discussing the problems of the world to a wild night in Saarbrooklyn which will mature over time from a bad decision to a great story. We are here to help you with all your questions. Feel free to talk to us when you run into one of us on campus. We were founded in April, 2019 as the International Student Association (ISA) Saarbrücken. Since June, 2020, we are officially an ESN section. Right now, we are a group of 30 volunteers to help the students. We are looking forward to meeting you. Your ESN Saarbrücken Team 02 ESN SAARBRÜCKEN BUCKET LIST © Herbert Frank / Flickr © EDEKA Eat Dibbelabbes -
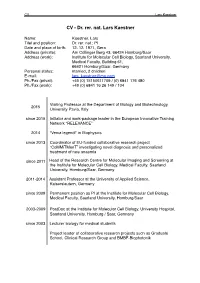
CV Lars Kaestner
CV Lars Kaestner CV - Dr. rer. nat. Lars Kaestner Name: Kaestner, Lars Titel and position: Dr. rer. nat.; PI Date and place of birth: 12. 12. 1971, Gera Address (private): Am Collinger Berg 43, 66424 Homburg/Saar Address (work): Institute for Molecular Cell Biology, Saarland University, Medical Faculty, Building 61, 66421 Homburg/Saar, Germany Personal status: married, 2 children E-mail: [email protected] Ph./Fax (privat): +49 (0) 15150611709 / (0) 6841 176 480 Ph./Fax (work): +49 (0) 6841 16 26 149 / 104 Visiting Professor at the Department of Biology and Biotechnology, 2015 University Pavia, Italy since 2015 Initiator and work-package leader in the European Innovative Training Network “RELEVANCE” 2014 “Venia legendi" in Biophysics since 2013 Coordinator of EU-funded collaborative research project “CoMMiTMenT” investigating novel diagnosis and personalized treatment of rare anaemia since 2011 Head of the Research Centre for Molecular Imaging and Screening at the Institute for Molecular Cell Biology, Medical Faculty, Saarland University, Homburg/Saar, Germany 2011-2014 Assistant Professor at the University of Applied Science, Kaiserslautern, Germany since 2009 Permanent position as PI at the Institute for Molecular Cell Biology, Medical Faculty, Saarland University, Homburg/Saar 2003-2009 PostDoc at the Institute for Molecular Cell Biology, University Hospital, Saarland University, Homburg / Saar, Germany since 2003 Lecturer biology for medical students Project leader of collaborative research projects such as Graduate School, Clinical -

Simon Ostermann
Simon Ostermann Personal Data Place and Date of Birth: Neunkirchen/Saar | 28.08.1992 Address: Building C 7.4, room 3.17, Saarland University Phone: +49 (0)681 302 70033 Mail: [email protected] Education September 2015 - present PhD Student in the Collaborative Research Center (“Sonderforschungsbereich”) SFB-1002 on Information Density and Linguistic Encoding, Project A3 Superviosr: Prof. Dr. Manfred Pinkal Saarland University, Saarbrücken October 2013 - August 2015 Master of Science in Language Science and Technology Saarland University, Saarbrücken Grade: 1.3 Thesis: “Exploring the Role of Textual Entailment for Short-Answer Scoring” Advisors: Prof. Dr. Manfred Pinkal, Dr. Michael Roth March 2015 - August 2015 Visiting Postgraduate Research Student, Exchange Semester The University of Edinburgh, Edinburgh October 2013 Bachelor of Science in Computational Linguistics Saarland University, Saarbrücken Grade: 1.2 (with distinction) Thesis: “The Applicability of Active Learning for Language-Learner Corpora” Advisors: Prof. Dr. Manfred Pinkal, Dr. Alexis M. Palmer 2010 Abitur (german A-levels) Arnold-Janssen-Gymnasium St. Wendel Grade: 1.6 Work Experience September 2015 - present Researcher at Collaborative Research Center SFB-1002 Project A3, Saarland University 2013 - 2015 Research Assistant at Computational Linguistics Department Group Pinkal, Saarland University 2011 - 2013 Research Assistant at “Allegro” Projekt Saarland University 11/2012 - 10/2013 Working Student at SemVox GmbH Saarbrücken 09/2012 - 10/2013 Internship at SemVox -

Comparing Syllable Frequencies in Corpora of Written and Spoken Language
INTERSPEECH 2011 Comparing syllable frequencies in corpora of written and spoken language Barbara Samlowski 1, Bernd Möbius 2, Petra Wagner 3 1 Division of Language and Speech Communication, University of Bonn, Germany 2 Department of Computational Linguistics and Phonetics, Saarland University, Germany 3 Faculty of Linguistics and Literary Studies, Bielefeld University, Germany [email protected], [email protected], [email protected] Abstract language. The largest database analyzed for the present study is the DEWAC corpus, a collection of texts crawled from the In this study, various German language corpora were internet containing more than 1.5 billion running word forms compared in order to discover the extent to which syllable [10]. The other written language corpus, referred to here as the frequencies remain stable across different contexts and Leipzig corpus, comprises approximately 170 million words modalities. Although considerable differences in relative from newspaper articles [11]. frequency were found among the more common syllables, All spoken-language corpora were analyzed on the basis rank numbers proved to be more robust. Variation across of orthographic representations. The Europarl corpus consists corpora was mostly due to vocabulary characteristics of of transcriptions from European Parliament proceedings [12]. particular corpus domains rather than to systematic differences With a total of nearly 40 million words, it is the largest spoken between spoken and written language. The results indicate that language corpus investigated here, although the style of syllable frequencies in written corpora can be taken as a rough speech is comparatively formal and planned. The other two estimate for their frequency in spoken language. -

Daniel Bauer, Ph.D
Daniel Bauer, Ph.D. Dept. of Computer Science, 1214 Amsterdam Ave, 450 Computer Science Building, New York, NY 10027 [email protected] http://www.cs.columbia.edu/∼bauer RESEARCH INTERESTS In the area of Natural Language Processing, my work touches on syntactic and semantic parsing, grammar formalisms, lexical and computational semantics, knowledge representation, and machine learning. My current research interests in computer science education include integrating functional programming into the CS curriculum, understanding how pre-college computing experience shapes performance and attitudes in introductory CS courses, and techniques for improving student engagement. EDUCATION 2017 Ph.D. Computer Science, Columbia University 2009 M.Sc. Language Science and Technology, Saarland University, Germany 2007 B.Sc. Cognitive Science (with distinction), University of Osnabr¨uck, Germany TEACHING EXPERIENCE 2017 - current Lecturer in Discipline (Natural Language Processing) Columbia University Taught a variety of courses on the undergraduate and graduate level, icluding introductory CS, AI, and Natural Language Processing 2014-2016 Preceptor, Columbia University. RESEARCH EXPERIENCE 2010-2016 Graduate Research Assistant, Center for Computational Learning Systems and Spoken Language Processing Group, Columbia University Projects: NSF funded project From Text to Pictures. Detecting Relations and Anomalies in Text and Speech under the DARPA DEFT program. Summer 2013 Visiting Research Assistant, Information Sciences Institute, Summer 2012 University -

Alexander Koller
ALEXANDER KOLLER Department of Computer Science [email protected] Columbia University http://www.columbia.edu/˜koller/ September 2006 RESEARCH INTERESTS Efficient algorithms and logic-based methods in computational linguistics; computational semantics; formal languages; generation; the language- robotics interface. EDUCATION 1999 – 2004 Dr. rer. nat. (Ph.D.), Computer Science, Saarland University Dissertation: Constraint-based and graph-based resolution of ambiguities in natural language Advisors: Manfred Pinkal and Gert Smolka Grade: summa cum laude (best possible grade, rarely given) 1994 – 1999 Diplom (M.Sc.) in Computational Linguistics, Saarland University Grade: 1.0 (best possible grade) 1994 – 1999 Diplom (M.Sc.) in Computer Science, Saarland University Grade: 1.0 (best possible grade) 1996 Vordiplome (≈ B.Sc. degrees) in Computational Linguistics, Computer Science, and Mathematics PROFESSIONAL EXPERIENCE 09/06 – 08/07 DFG Research Fellow, Columbia University Efficient algorithms for sentence generation 05/99 – 08/06 Researcher (Wissenschaftlicher Mitarbeiter), Saarland University Project CHORUS: Computational semantics, underspecification 04/00 – 06/00 Visiting scholar, ICCS, University of Edinburgh 05/98 – 04/99 Research assistant, Project CHORUS (Prof. Manfred Pinkal) Scope underspecification, development of a solver for context unification 1 03/98 – 04/98 Internship at SRI International, Cambridge, UK Development of a system for anaphora resolution 08/96 – 09/97 Research assistant, Project OMEGA (Prof. Jörg Siekmann) Development -

Supporting Information Baikalomycins A-C, New Aquayamycin-Type Angucyclines Isolated from Lake Baikal Derived Streptomyces Sp
Supporting Information Baikalomycins A-C, New Aquayamycin-Type Angucyclines Isolated from Lake Baikal Derived Streptomyces sp. IB201691-2A Irina Voitsekhovskaia 1,†,‡, Constanze Paulus 2,†, Charlotte Dahlem 3, Yuriy Rebets 4, Suvd Nadmid 4,§, Josef Zapp 3, Denis Axenov-Gribanov 1,5, Christian Rückert 6, Maxim Timofeyev 1,5, Jörn Kalinowski 6, Alexandra K. Kiemer 3 and Andriy Luzhetskyy 2,4,* 1 Institute of Biology, Irkutsk State University, 664003 Irkutsk, Russia; [email protected] (I.V.); [email protected] (D.A.-G.); [email protected] (M.T.) 2 Helmholtz Institute for Pharmaceutical Research Saarland, 66123 Saarbrücken, Germany; [email protected] 3 Pharmaceutical Biology, Saarland University, 66123 Saarbrücken, Germany; [email protected] (C.D.); [email protected] (J.Z.); [email protected] (A.K.K.) 4 Pharmaceutical Biotechnology, Saarland University, 66123 Saarbrücken, Germany; [email protected] (Y.R.); [email protected] (S.N.) 5 Baikal Research Centre, 664003 Irkutsk, Russia 6 Technology Platform Genomics, Center for Biotechnology (CeBiTec), Bielefeld University, 33615 Bielefeld, Germany, [email protected] (C.R.); [email protected] (J.K.) * Correspondence: [email protected]; Tel.: +49-681-302-70200 † These authors contributed equally to this work. ‡ Current address: Interfaculty Institute of Microbiology and Infection Medicine (IMIT), Microbiology/Biotechnology, Eberhard Karls University of Tübingen, 72074 Tübingen, Germany; [email protected] § Current address: School of Pharmacy, Mongolian National University of Medical Sciences, 14210 Ulaanbaatar, Mongolia Received: 7 April 2020; Accepted: 5 May 2020; Published: date Table S1. -

LANTERN 2021 Proceedings of the Third Workshop on Beyond Vision
LANTERN 2021 Proceedings of the Third Workshop on Beyond Vision and LANguage: inTEgrating Real-world kNowledge (LANTERN) April 20, 2021 Kyiv, Ukraine (Online) ©2021 The Association for Computational Linguistics Order copies of this and other ACL proceedings from: Association for Computational Linguistics (ACL) 209 N. Eighth Street Stroudsburg, PA 18360 USA Tel: +1-570-476-8006 Fax: +1-570-476-0860 [email protected] ISBN 978-1-954085-15-2 ii Introduction Welcome to LANTERN 2021, the Third Workshop Beyond Vision and Language: Integrating Real- World Knowledge, co-located with EACL 2021. Building on the successes of the first edition co-located with EMNLP-IJCNLP 2019 and the second edition co-located with COLING 2020, the third edition of LANTERN aims to again bring together and interconnect researchers focusing on natural language research from a multimodal perspective. In particular, the main goal of the workshop is to promote and foster research which uses machine- and deep-learning techniques to interconnect language with vision and other modalities by leveraging external knowledge. We encourage contributions which exploit very diverse sources of external knowledge like knowledge graphs, fixed and dynamic environments, cognitive and neuroscience data, etc. This results in the workshop being open to all research directions which acknowledge the importance of knowledge in acquiring, using, and evaluating language in real-world settings. In this third edition, we called for both long and short papers. All the accepted contributions are published in these Proceedings. LANTERN 2021 received 11 submissions, all of which were double-blindly reviewed by three highly-qualified reviewers. In total, 5 papers (4 long, 1 short) were accepted to appear in the Proceedings of the workshop, with an acceptance rate of around 55% (comparable to that of the first and second edition, which was around 53% and 57%, respectively). -

Lecture Notes in Artificial Intelligence 7006
Lecture Notes in Artificial Intelligence 7006 Subseries of Lecture Notes in Computer Science LNAI Series Editors Randy Goebel University of Alberta, Edmonton, Canada Yuzuru Tanaka Hokkaido University, Sapporo, Japan Wolfgang Wahlster DFKI and Saarland University, Saarbrücken, Germany LNAI Founding Series Editor Joerg Siekmann DFKI and Saarland University, Saarbrücken, Germany Joscha Bach Stefan Edelkamp (Eds.) KI 2011:Advances in Artificial Intelligence 34th Annual German Conference on AI Berlin, Germany, October 4-7, 2011 Proceedings 13 Series Editors Randy Goebel, University of Alberta, Edmonton, Canada Jörg Siekmann, University of Saarland, Saarbrücken, Germany Wolfgang Wahlster, DFKI and University of Saarland, Saarbrücken, Germany Volume Editors Joscha Bach Humboldt-University of Berlin Berlin School of Mind and Brain Unter den Linden 6, 10099 Berlin, Germany E-mail: [email protected] Stefan Edelkamp University of Bremen Faculty 3, Mathematics and Computer Science P.O. Box 33 04 40, 28334 Bremen, Germany E-mail: [email protected] ISSN 0302-9743 e-ISSN 1611-3349 ISBN 978-3-642-24454-4 e-ISBN 978-3-642-24455-1 DOI 10.1007/978-3-642-24455-1 Springer Heidelberg Dordrecht London New York Library of Congress Control Number: 2011936978 CR Subject Classification (1998): I.2, H.4, F.1, H.2.8, I.2.6, H.5.2 LNCS Sublibrary: SL 7 – Artificial Intelligence © Springer-Verlag Berlin Heidelberg 2011 This work is subject to copyright. All rights are reserved, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, re-use of illustrations, recitation, broadcasting, reproduction on microfilms or in any other way, and storage in data banks.