Fidaxomicin Compared with Oral Vancomycin for the Treatment of Severe Clostridium Difficile-Associated Diarrhea: a Retrospective Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Volume 35, Issue 4 (Summer 2009)
Metropolitan Detroit Medical Library Group VOLUME 35 ISSUE 4 MDMLG NEWS Summer 2009 President’s Corner with Cathy Eames MDMLG gives a scholarship to a library science student interested in medical librarianship each year. It is presented at the summer luncheon, an event that over half of the membership attends, and a time when we eat and laugh together and hear an uplifting or informational talk. It’s easy to appear positive the day the scholarship is presented, but in my mind there is an underlying current of conflict. How do we encourage students coming into www .mdmlg.org the profession when what we’re seeing around us are budget cuts, staff reductions and library closures? Christine Chastain-Warheit, chair of the MLA Hospital Library Section Inside This Issue wrote in the April National Network that she is taking inspiration from a recent Stephen Abram article in entitled “We are a Profession That 1 President’s Corner Makes a Difference.” Abram says, “Libraries matter” and “Librarians 2 Dearborn Inn change lives.” 3 Summer Luncheon In his book, Good to Great and the Social Sectors, Jim Collins writes Preview about conducting sessions with a group of healthcare executives. He asked them what needed to happen for them to build great hospitals. 4 MyDelivery The executives began talking about all the systemic problems like Medicare/Medicaid, the uninsured, fear of lawsuits, and more. Then he 5 SEMLOL asked them to come up with an example of a healthcare organization 6 Shiffman Returns that made the leap to superior results despite the systemic problems. -
DWIHN Provider Directory List 2021
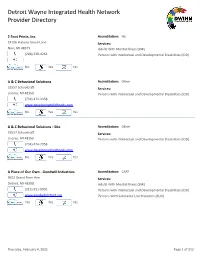
Detroit Wayne Integrated Health Network Provider Directory 2 Foot Prints, Inc. Accreditation: No 24106 Hickory Grove Lane Services: Novi, MI 48375 Adults With Mental Illness (SMI) (248) 330-4264 Persons with Intellectual and Developmental Disabilities (IDD) No Yes Yes A & C Behavioral Solutions Accreditation: Other 31557 Schoolcraft Services: Livonia, MI 48150 Persons with Intellectual and Developmental Disabilities (IDD) (734) 474-2958 www.developingchildhoods.com No Yes Yes A & C Behavioral Solutions - Site Accreditation: Other 31557 Schoolcraft Services: Livonia, MI 48150 Persons with Intellectual and Developmental Disabilities (IDD) (734) 474-2958 www.developingchildhoods.com No Yes Yes A Place of Our Own - Goodwill Industries Accreditation: CARF 9622 Grand River Ave. Services: Detroit, MI 48208 Adults With Mental Illness (SMI) (313) 931-0901 Persons with Intellectual and Developmental Disabilities (IDD) www.goodwilldetroit.org Persons With Substance Use Disorders (SUD) Yes Yes Yes Thursday, February 4, 2021 Page 1 of 252 Detroit Wayne Integrated Health Network Provider Directory Abney Home Accreditation: No 34717 Pardo Services: Westland, MI 48185 Adults With Mental Illness (SMI) (313) 274-0044 Persons with Intellectual and Developmental Disabilities (IDD) No Yes Yes Abundant Community Recovery Accreditation: CARF 16476 Bringard Services: Detroit, MI 48205 Persons With Substance Use Disorders (SUD) (313) 447-5070 No Yes Yes Abundant Community Recovery Accreditation: CARF 20267 Huntington Services: Harper Woods, MI 48225 Persons With Substance Use Disorders (SUD) (313) 447-5070 No Yes Yes Academy of Dreams Accreditation: No 18640 E. 14 Mile A4 Services: Fraser, MI 48026 Persons with Intellectual and Developmental Disabilities (IDD) (313) 401-7175 No Yes Yes Thursday, February 4, 2021 Page 2 of 252 Detroit Wayne Integrated Health Network Provider Directory Academy of Dreams Accreditation: No 18640 E. -

Employers' Deadlines for Decisions Now Loom
20120702-NEWS--0001-NAT-CCI-CD_-- 6/29/2012 6:05 PM Page 1 ©Entire contents copyright 2012 by Crain Communications Inc. All rights reserved www.crainsdetroit.com Vol. 28, No. 27 Chinese automaker setsPage up 3 headquarters in Birmingham Advanced manufacturing 3-D process takes manufacturing to new levels, Page 9 Crain’s Largest OEM parts suppliers, Page 12 Agreement may be near on Belle Isle C Aquarium YOUR reopening RAIN share your views on the Detroit River — literally. Crain’s Lists ’ D S Detroit River, photos of out-of- the-way hangouts and bars by the river or photos of ETROIT interesting spots to fish, play or stories to go with them. WANTS TO SEE relax. Be sure to include an We’re looking for views of the explanation and story with your photos. river photos and the would like you to be part of a contest for the best photo. Prizes will be given to Investing in the D the top photos, picked by submitting your favorite Crain’s Business’ Living and 20 special publication Submit photos by July 27 to of others, will be used in print and Be part of the Aug. online as part of this annual publication. Crain’s Detroit The winning photo, and many electronically, go to R detroit.com/riverviews. Deputy Managing Editor IVER PICS To submit a photo Duggan @crain.com or (313) 446-0414. For questions, contact Employers’ deadlines editors. for decisions now loom NEWSPAPER State delay on health exchange muddies waters at dduggan has ruled, employers can be ex- by pected to begin to moving forward with plans to comply with regula- tory requirements of the Patient Now that the Protection and Affordable Care Act. -

Henry Ford Hospital 1
PATIENT & GUEST SERVICES HENRY FORD HOSPITAL 1. Chapel 2. Patient Records 3. DFCU Financial Patient/Employee SHOPPING SERVICES Garage (PEG) 4. Henry Ford Health Products Employee 5. LiveWell Shoppe Parking 6. OptimEyes Lot 7. Pharmacy H KEY ENTRANCES FOOD SERVICES 8. Henry’s Express 3 ELEVATOR 9. BIGGBY COFFEE STAIRS 10. Henry’s on the Boulevard 11. Subway Guest 10 RESTROOM 12. Papa Joe’s Market Parking Lot ELEVATOR TO $2.50 Cafeteria PATIENT FLOORS RETAIL HOURS OF OPERATION* ATM LOCATIONS 11 BIGGBY Coffee ? INFORMATION Hours: 24 hours, 7 days a week Clara Ford Pavilion DESKS Atrium DFCU Financial Hours: Monday – Friday, 8:30 a.m. - 4 p.m., Payday (every other Buerki 9 M Friday), 7:30 a.m. - 4 p.m. FIRST FLOOR Auditorium Unit Henry Ford Health Products AMBULANCE 2 ENTRANCE Hours: Monday – Friday, 8:30 a.m. – 4:30 p.m. Henry Ford OptimEyes™ Emergency Hours: Monday – Thursday, 8 a.m. – 6 p.m., Friday, 8 a.m. – 5 p.m., K East Entrance Saturday, 9 a.m. – 3 p.m., Sunday, noon – 5 p.m. WC Emergency 24 Hr . Entrance Clinic 4 ? (valet available) Henry's Express West Clinic Bldg. Hours: 6 a.m. - midnight, daily Maternity 127 Henry's on the Boulevard Entrance Hours: Monday – Friday, 6:30 a.m. – 7:30 p.m. Saturday – Sunday, 6:30 a.m. - 2 p.m. Breakfast, 6:30 – 9:30 a.m. Blue Awning Lunch, 10:30 a.m. – 2 p.m. 6 12 Afternoon Break, 2 p.m. – 4:30 p.m Dinner, 4:30 – 7:30 p.m. -

7451 Woodward Avenue, Detroit, Michigan Prime Retail Space
Prime Retail Space Available 7451 Woodward Avenue, For Lease 4,086 SF Available Detroit, Michigan 0.88 Acres | Parking Available WOODWARD AVENUE RETAIL STRIP | NEW CENTER | 7451 WOODWARD AVENUE, DETROIT, MI PROPERTY FEATURES • 10,.730 SF Total Building Square Footage • Large 1.32 Parcel With Over 50 Parking Spaces • Woodward Avenue Frontage & Signage Available • Located In the Immediate Proximity of the New Center, Cadillac Place, Fisher Theater, Henry Ford Hospital Campus, College for Creative Studies, Shinola Headquarters, & More. • Over 194 Feet of Lot Frontage On Woodward Avenue Prime Retail Space Available 7451 Woodward Avenue, For Lease 4,086 SF Available Detroit, Michigan 0.88 Acres | Parking Available WOODWARD AVENUE RETAIL STRIP | NEW CENTER | 7451 WOODWARD AVENUE, DETROIT, MI NEW CENTER DEVELOPMENTS 1. Lee Plaza - 2240 W Grand Blvd - $50 Million redevelopment of a15-story vacant building into a 180-unit apartment building, done by Roxbury Group 2. Motown Museum - 2658 W Grand Blvd - $50 Million, 50,000 square foot expansion with a new theatre, recording studios, interactive exhibits, and meeting spaces 3. Henry Ford Brigitte Harris Cancer Pavilion - 6499 Trumbull Avenue - Situated directly across from its 2M SF Hospital, Henry Ford is currently constructing the pavilion with a skyway connecting the site with the larger hospital. The building is part of a 300-acre ex- pansion in the area. 4. The Boulevard - 7301 3rd Ave - Rising near the Fisher Building is new construction in the form of 231 apartments and 17,500 square feet of retail space. Construction is close to complete, and the developer, The Platform has already secured several commercial ten- ants. -

Congestive Cardiomyopathy As an End Stage of Toxoplasma Myocarditis Mohsin Alam
Henry Ford Hospital Medical Journal Volume 23 | Number 3 Article 6 9-1975 Congestive Cardiomyopathy as an End Stage of Toxoplasma Myocarditis Mohsin Alam Wolf F. C. Duvernoy Edward L. Quinn Evelyn J. Fisher Follow this and additional works at: https://scholarlycommons.henryford.com/hfhmedjournal Part of the Life Sciences Commons, Medical Specialties Commons, and the Public Health Commons Recommended Citation Alam, Mohsin; Duvernoy, Wolf F. C.; Quinn, Edward L.; and Fisher, Evelyn J. (1975) "Congestive Cardiomyopathy as an End Stage of Toxoplasma Myocarditis," Henry Ford Hospital Medical Journal : Vol. 23 : No. 3 , 141-144. Available at: https://scholarlycommons.henryford.com/hfhmedjournal/vol23/iss3/6 This Article is brought to you for free and open access by Henry Ford Health System Scholarly Commons. It has been accepted for inclusion in Henry Ford Hospital Medical Journal by an authorized editor of Henry Ford Health System Scholarly Commons. Henry Ford Hosp. Med. Journal Vol. 23, No. 3, 1975 Congestive Cardiomyopathy as an End Stage of Toxoplasma Myocarditis /Vtohsin Alam, iVlD*; Wolf F.C. Duvernoy, IVtD*, Edward L. Quinn, IVlD** and Evelyn J. Fisher, MD** Ackcquire d toxoplasma myocarditis and pericarditis have been well described in literature, '^'^ but congestive cardiomyo pathy as a consequence of a clinically well documented toxoplasma myocarditis has been rarely documented during life.' We are presenting a case of cardiomyo Congestive cardiomyopathy is a clinical pathy feft to be due to toxoplasmosis where entity which may be due to many different the titers of Sabin-Feldman dye tests and etiologies in addition to the primary type. indirect fluorescent antibody tests rose dur The case presented defines the etiology in a ingthe acute illness and returned to normal 30-year-old patient as previous acute tox wfth clinical improvement after specific oplasma myocarditis. -

7300 Woodward 7300 WOODWARD AVENUE, DETROIT
7300 Woodward 7300 WOODWARD AVENUE, DETROIT RETAIL SPACE AVAILABLE FOR LEASE PLATFORM LEASING & BROKERAGE 2 7300 WOODWARD PLATFORM LEASING & BROKERAGE 3 At the intersection of Woodward and 7300 Woodward Grand Blvd. - where four prominent Detroit 7300 WOODWARD AVENUE, DETROIT neighborhoods converge - is an Albert Kahn 7300 Woodward sits at the prominent intersection of Woodward Avenue and Grand Boulevard where treasure. A dramatic new facade and major the New Center, Milwaukee Junction, Tech Town and North End neighborhoods meet. renovation will make this historic gem a Less than one mile from I-75, I-94 and M-10, 7300 Woodward is easily accessed by area expressways and features ample on-site parking. Additionally, the first QLine streetcar is just steps from the notable landmark at the gateway to Detroit. building, providing convenient transportation to and from Midtown and the CBD. Significant capital investment is underway, modernizing and repositioning the building to attract Peter D. Cummings new office and retail tenants. Improvements include updating the facade, entries, HVAC system and elevators. Executive Chairman & CEO + Access to freeways + public transit + Albert Kahn interior design + Abundant on-site and nearby parking + Marble, brass and art deco finishes 3 04.xx.20 + Value of greater New Center + Walkable retail and F&B Stage of Development NEIGHBORHOOD PROJECT TYPE TOTAL OFFICE North End Office, Retail 210,000 SF ADDRESS TOTAL SIZE TOTAL RETAIL 7300 Woodward Ave. 240,000 SF 30,000 SF ORIGINAL DATE BUILT PARKING AVAILABLE -

House Staff Manual 2020-2021
House Staff Manual 2020-2021 Henry Ford Macomb Hospitals 1 Contents KEY CONTACTS ......................................................................................................................................................... 4 KEY RESOURCES & SERVICES ............................................................................................................................... 4 KEY LINKS .................................................................................................................................................................. 4 Henry Ford Health System ............................................................................................................................................ 5 HFHS Mission Statement ........................................................................................................................................ 5 HFHS Vision Statement ........................................................................................................................................... 5 HFHS Value Statement ............................................................................................................................................ 5 Henry Ford Health System Medical Education ............................................................................................................. 5 HFHS Medical Education Mission Statement ......................................................................................................... 6 HFHS Medical Education Vision Statement -

Neeme Järvi Detroit Symphony Orchestra Ida Kavafian
NEEME JÄRVI MOTORCITY TRIPTYCH DETROIT SYMPHONY ORCHESTRA RAISE THE ROOF IDA KAVAFIAN, VIOLIN 559372 bk Daugherty US 5/27/09 2:05 PM Page 2 Michael Daugherty (b. 1954) Detroit Symphony Orchestra Fire and Blood • MotorCity Triptych • Raise the Roof The internationally acclaimed Detroit Symphony Orchestra traces its history back to 1887. Today the orchestra Fire and Blood (2003), for violin and orchestra, was II. River Rouge performs for more than 400,000 people annually in classical, Pops, jazz, World music, special, holiday, young commissioned by the Detroit Symphony Orchestra. The At the Ford River Rouge Automobile Complex, located people’s, community and summer concerts. Its 8 Days in June festival presents works from the symphonic world première was given by the Detroit Symphony next to the Detroit River, Rivera spent many months repertoireMichael in a modernDaugherty context, as well as contemporary pieces that take orchestral and chamber music in new Orchestra under the direction of Neeme Järvi, with Ida creating sketches of workers and machinery in action. directions. The Detroit Symphony Orchestra performs in historic Orchestra Hall at the Max M. Fisher Music Center, Kavafian, solo violin, at Orchestra Hall, Detroit, He was accompanied by his young wife, the remarkable as well as inFire other and Michigan Blood venues such as Meadow Brook Music Festival in the summertime. In the 2008-09 Michigan on 3rd May, 2003. In 1932, Edsel Ford Mexican painter Frida Kahlo (1906-1954). She lived in season, world-renowned8.559372 conductor Leonard Slatkin became Music Director of the orchestra. The Detroit Symphony commissioned the Mexican modernist artist Diego constant pain as a result of polio in childhood and a Orchestra’s distinguished history includes many award-winning recordings, tours and residencies in the United Rivera (1886-1957) to paint a mural representing the serious bus accident at the age of eighteen in Mexico States, Europe and Japan, and national and international radio broadcasts. -

Renters Help Book Cadillac Get to Half Full
20100510-NEWS--0001-NAT-CCI-CD_-- 5/7/2010 6:25 PM Page 1 ® www.crainsdetroit.com Vol. 26, No. 19 MAY 10 – 16, 2010 $2 a copy; $59 a year ©Entire contents copyright 2010 by Crain Communications Inc. All rights reserved Renters Page 3 Masco finding its way in First Michigan eyes smaller construction market help Book Lending Cadillac get a hand to banking’s big leagues young Jewish professionals to half full Financier Condo sales Inside Ross backs expected to pick Companies get help growth plan up with economy landing first-time BY TOM HENDERSON BY DANIEL DUGGAN CRAIN’S DETROIT BUSINESS government contracts, CRAIN’S DETROIT BUSINESS Page 8 At one point during the pre- The once-tiny First Michigan Bank sale period for the 63 condomini- of Troy is tiny no more, thanks to ums atop the Health Care Extra the acquisition on April 30 of $1.1 Book Cadillac billion in assets from CF Bancorp of building, all New residency programs Port Huron and its 22 Citizens First but four units come with big expectations Bank branch- were sold. SHUTDOWNS es, including But after the at St. Mary Mercy, Page 9 six in South- irrational exu- Troubled banks: east Michigan. DAVID DALTON berance of 2006 Expect trail of Not satis- A new First Michigan sign signals the Troy-based bank’s acquisition of CF takeovers to became more This Just In fied by in- Bancorp of Port Huron — part of a growth strategy outlined by First Michigan rational, deals continue, Page 22 CEO and Chairman David Provost. -

OPHTHALMOLOGY NEWS Department of Ophthalmology Newsletter - Summer 2018
OPHTHALMOLOGY NEWS Department of Ophthalmology Newsletter - Summer 2018 CHAIRMAN’S UPDATE The Henry Ford Department We continue to have an excellent residency program of Ophthalmology is pleased that is recognized by top schools in the country as is to provide news and updates evidenced by the successful match of our residents on department activities into fellowships this year. See listing on page 7. in this newsletter. First, a reminder about our “Updates The recent health system announcement of a new in Ophthalmology” Alumni medical center in the Village of Bloomfield Hills Education Day to be held June including Eye Care facilities is very exciting. In addition 16, 2018 at Henry Ford Hospital to this site, there are other locations in the Metro in the Buerki Auditorium. If you Detroit Area that we are looking into expanding our Paul Edwards, M.D. have not already done so, please eye care services. take a moment to register. We are looking forward to a weekend packed with lots of activities. This is the first In closing, I would like to express my deepest time we are holding Alumni Day in conjunction with the appreciation to alumni donors and friends of the EyesOn Design Car Show events. See page 11 for more department. We are thankful to you for our successes details on registration and tickets. in the past and present. Your continued support will help us for future successes in the training of the next Next up will be our Annual Jack S. Guyton Alumni generation of physicians, providing our patients with Reunion in Chicago scheduled for 6:00 to 9:00 p.m. -

Download the Program Book
Hilton Miami Airport Miami, FL March 10-13, 2016 www.amwa-doc.org A Mighty Woman with a Torch (Oil, Acrylic on canvas 2016) Kathryn Ko, MD, MFA AMWA 101st Anniversary Meeting Charting the Next Century of Women in Medicine 1 2 3 AMWA PRESIDENT Dear AMWA Members, the launch of Studio AMWA which demonstrates the beauty of art and its influence on our lives in medicine. This year much has been accomplished and your dedication to the AMWA mission is AMWA is strong, AMWA is vibrant, AMWA is alive and it is be- commendable. We started new task forces: cause of you! Thank you for the work you have done and for your The Confidential Interview, Emotional Dis- perseverance. I have heard from many of you as you recognize your tress and Prevention of Physician Suicide, colleagues for their good work, when you call to let us know about Paid Maternity Leave and Gun Violence Prevention. We have wrongs that need to be righted, and when you donate your time, reinforced our work in many areas as our committees are active, talent and treasure to AMWA which allows us to continue. involved, and making things happen. We combined forces with Health and Human Services for a summit on Human Trafficking AMWA’s history is long and varied and I have learned from those and this first interprofessional work drew representatives from or- that have gone before me how to be strong, passionate, and effec- ganizations across the country. The Sex and Gender Summit, held tive. From those that come after me, let us maintain our enthusi- in the fall, really put us back on the map for leadership in women’s asm, look out for each other and parlay our work into your vision health and our goal to include sex and gender into all aspects of of the future.