Community Outbreak Investigation of SARS-Cov-2 Transmission Among Bus Riders in Eastern China
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

18 F, China Life Tower, No. 777 Lingqiao Road, Haishu District, Ningbo
18 F, China Life Tower, No. 777 Lingqiao Road, Haishu District, Ningbo View this office online at: https://www.newofficeasia.com/details/serviced-offices-18-f-china-life-tower-n o-777-lingqiao-road-haishu-district China Life Tower is an iconic and highly visible building which dominates the skyline and boasts LEED gold rating and 360 degree unobstructed views of the surrounding rivers. The serviced offices reside on the 18th floor and offer a quiet yet professional working environment which is equipped with the latest technology to help your business thrive. Stylish kitchen/diner facilities are available alongside executive meeting rooms, all of which can be accessed day or night and are protected by 24-hour security personnel for your safety. Transport links Nearest airport: Key features 24 hour access 24-hour security Car parking spaces Comfortable lounge Disabled facilities (DDA/ADA compliant) High-speed internet Lift Meeting rooms Suspended Ceilings Voicemail Location Located adjacent to the Fenghua River, your company can enjoy stunning riverside views and easy access to a plethora of local amenities. There is a popular shopping district nearby which is home to a diverse range of retailers, restaurants, banks and hotels. The street is well-served by bus routes and the metro line resides within easy walking distance while Ningbo Lishe International Airport can be reached within a 25 minute drive. Points of interest within 1000 metres China Everbright Bank (bank) - 150m from business centre Citic Hotel (hotel) - 366m from business centre Shangri-la -

Vertical Metal F'ile Cabinets
Barcode:3827074-03 C-570-111 INV - Investigation - CHINESE EXPORTERS AND PRODUCERS OF VERTICAL METAL F'ILE CABINETS Best Beaufy Furniture Co., Ltd. Feel Life Co., Ltd. Lianping Industry Zone, Dalingshan Town Room 202, Deweisen Building Dongguan, Guangdon g, 523809 Nanshan District, Shenzhen Tel: +86 769-85623639 1sf ¡ +86 7 55-66867080-8096 Fax: +86 769-85628609 Fax: +86 755-86146992 Email: N/A Email : [email protected] Website: Website : www. feellife. com www. d gbestbeauty. company. weiku. com/ Fujian lvyer Industrial Co., Ltd. Chung \ilah Steel Furniture Factory Co., Yangxia Village, Guhuai Town Lrd. Changle, Fujian, 350207 Block A,7lF Chinaweal Centre Tel: +86 59128881270 414-424 Jaffe Road, Wanchai Fax: +86 59128881315 Hong Kong Email : nancy @flivyer. com Tel: +85 228930378 Website : www. ivyer.net. cnl Fax: +85 228387626 Email: N/A Fuzhou Nu Deco Crafts Co., Ltd. Website : http ://chungwah. com.hk/ 1306 Xinxing Building No. 41, Bayiqi Mid. Road Concept Furniture (Anhui) Co.' Ltd. Fuzhou, Fujian, 350000 Guangde Economic and Technical Tel: +86 591-87814422 Developm ent Zone, Guangde County P¿¡; +86 591-87814424 Anhui, Xuancheng, 242200 Email: [email protected] Tel: 865-636-0131 Website : http :/inu-deco.cnl Fax: 865-636-9882 Email: N/A Fuzhou Yibang Furniture Co., Ltd. Website: N/A No. 85-86 Building Changle Airport Industrial Zone Dong Guan Shing Fai X'urniture Hunan Town, Changle 2nd Industrial Area Fujian, Fuzhou, 350212 Shang Dong Administrative Dist. fsf; +86 591-28637056 Qishi, Dongguan, Guangdong, 523000 Fax: +86 591-22816378 Tel: +86 867592751816 Email: N/A Fax: N/A V/ebsite : htþs ://fi yb. -
Nbo Apr Schedule 3月24, 2021
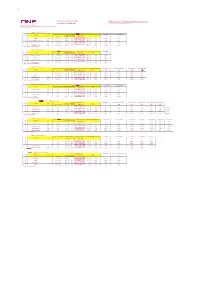
TP Remarks: 2021 Apr Vessel Schdule Export 1. Attention To China Customs Advance Manifest (CCAM) Regulation : Please submit CCAM to China Customs 24 hours prior to cargo loading on vessels sailing to/from China mainland ports. Last Updated at: 23-Mar-2021 2. Schedules are subject to change without prior notice. Ocean Network Express (China) Ltd. Room 1103-1106, 11F,China life Building,NO.777,Lingqiao Road, Haishu District, Ningbo City,Zhejiang Province 北美航线 PS6(Direct Service) Ningbo 二期(NBCT) ETA USLAX ETA OAKLAND WK VSL NAME VOY CY Cutoff AMS Cutoff VGM Cutoff ETD CY Open 08:00 AM 12:00 AM 15天 21天 ETB - 24 Hours(ETB 14 CZECH 101E Per terminal SUN SAT 时间以港区网站为准) Wed. 7-Apr 22-Apr 28-Apr ETB - 24 Hours(ETB 15 KUALA LUMPUR EXPRESS 089E Per terminal SUN SAT 时间以港区网站为准) Wed. 14-Apr 29-Apr 5-May ETB - 24 Hours(ETB 16 MOL CELEBRATION 082E Per terminal SUN SAT 时间以港区网站为准) Wed. 21-Apr 6-May 12-May ETB - 24 Hours(ETB 17 SEASPAN ADONIS 062E Per terminal SUN SAT 时间以港区网站为准) Wed. 28-Apr 13-May 19-May 船代 : 兴港 (Ningbo Xinggang) 北美航线 PS5(Direct Service) Ningbo 三期(NINGBO ZHOUSHAN PORT CO.LTD BEILUN SECOND CONTAINER TERMINAL BRANCH) ETA USLAX WK VSL NAME VOY CY Cutoff AMS Cutoff VGM Cutoff ETD CY Open 16:00 PM 17:00 PM 13天 ETB - 24 Hours(ETB 14 HYUNDAI SPLENDOR 082E Per terminal FRI THU 时间以港区网站为准) Mon. 5-Apr 18-Apr ETB - 24 Hours(ETB 15 VMS Per terminal FRI THU 时间以港区网站为准) Mon. 12-Apr 25-Apr ETB - 24 Hours(ETB 16 MOL PRESTIGE 066E Per terminal FRI THU 时间以港区网站为准) Mon. -

Barcode:3844251-01 A-570-112 INV - Investigation
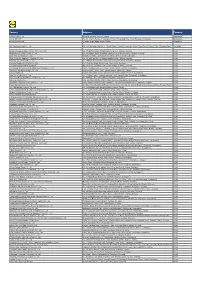
Barcode:3844251-01 A-570-112 INV - Investigation - PRODUCERS AND EXPORTERS FROM THE PRC Producer/Exporter Name Mailing Address A-Jax International Co., Ltd. 43th Fei Yue Road, Zhongshan City, Guandong Province, China Anhui Amigo Imp.&Exp. Co., Ltd. Private Economic Zone, Chaohu, 238000, Anhui, China Anhui Sunshine Stationery Co., Ltd. 17th Floor, Anhui International Business Center, 162, Jinzhai Road, Hefei, Anhui, China Anping Ying Hang Yuan Metal Wire Mesh Co., Ltd. No. 268 of Xutuan Industry District of Anping County, Hebei Province, 053600, China APEX MFG. CO., LTD. 68, Kuang-Chen Road, Tali District, Taichung City, 41278, Taiwan Beijing Kang Jie Kong 9-2 Nanfaxin Sector, Shunping Rd, Shunyi District, Beijing, 101316, China Changzhou Kya Fasteners Co., Ltd. Room 606, 3rd Building, Rongsheng Manhattan Piaza, Hengshan Road, Xinbei District, Changzhou City, Jiangsu, China Changzhou Kya Trading Co., Ltd. Room 606, 3rd Building, Rongsheng Manhattan Piaza, Hengshan Road, Xinbei District, Changzhou City, Jiangsu, China China Staple #8 Shu Hai Dao, New District, Economic Development Zone, Jinghai, Tianjin Chongqing Lishun Fujie Trading Co., Ltd. 2-63, G Zone, Perpetual Motor Market, No. 96, Torch Avenue, Erlang Technology New City, Jiulongpo District, Chongqing, China Chongqing Liyufujie Trading Co., Ltd. No. 2-63, Electrical Market, Torch Road, Jiulongpo District, Chongqing 400000, China Dongyang Nail Manufacturer Co.,Ltd. Floor-2, Jiaotong Building, Ruian, Wenzhou, Zhejiang, China Fastco (Shanghai) Trading Co., Ltd. Tong Da Chuang Ye, Tian -

'Yongjin', 'Xiaguang' and 'Yuhuang': Three Ornamental Cultivars Of
HORTSCIENCE 50(5):762–764. 2015. and Forestry University. These cultivars exhibit yellow or red leaves that stay on the branch for a longer period. These characteristics provide ‘Yongjin’, ‘Xiaguang’ and ‘Yuhuang’: higher ornamental value to the cultivars com- Three Ornamental Cultivars of pared with common camphor trees. Cinnamomum camphora Origin In Nov. 1998, we conducted a survey on Jianjun Wang the leaf color of roadside camphor trees in Center of Seeding Breeding, Forestry Bureau of Ningbo, Ningbo 315012, Haishu District, Ningbo, Zhejiang Province. Zhejiang, China; and Nurturing Station for the State Key Laboratory of Seeds from two superior trees were collected Subtropical Silviculture, Institute of Biotechnology, College of Forestry and to raise seedlings in the following year. In May Biotechnology, Zhejiang Agriculture and Forestry University, Lin’an, 1999, colors of the leaf, branch, and trunk were checked against the Pantone interna- Hangzhou 311300, Zhejiang, China tional color card C (Pantone Inc., 2008). A Wangshu Zhang seedling was found obviously different from the others for its golden yellow (Pantone Center of Seeding Breeding, Forestry Bureau of Ningbo, Ningbo 315012, 101C) leaves and red (Pantone 192C) Zhejiang, China branches and trunk, and asexual propagation 1 was then conducted. It has been found that Huahong Huang these color traits are stable on the basis of Nurturing Station for the State Key Laboratory of Subtropical Silviculture, 9-year observation. In addition, a special elec- Institute of Biotechnology, College of Forestry and Biotechnology, Zhejiang trophoresis band was discovered through an Agriculture and Forestry University, Lin’an, Hangzhou 311300, Zhejiang, intersimple sequence repeat (ISSR) analysis, China suggesting that the clone was different from the others in genomic DNA (Wang et al., Additional index words. -
Factory Address Country
Factory Address Country Durable Plastic Ltd. Mulgaon, Kaligonj, Gazipur, Dhaka Bangladesh Lhotse (BD) Ltd. Plot No. 60&61, Sector -3, Karnaphuli Export Processing Zone, North Potenga, Chittagong Bangladesh Bengal Plastics Ltd. Yearpur, Zirabo Bazar, Savar, Dhaka Bangladesh ASF Sporting Goods Co., Ltd. Km 38.5, National Road No. 3, Thlork Village, Chonrok Commune, Korng Pisey District, Konrrg Pisey, Kampong Speu Cambodia Ningbo Zhongyuan Alljoy Fishing Tackle Co., Ltd. No. 416 Binhai Road, Hangzhou Bay New Zone, Ningbo, Zhejiang China Ningbo Energy Power Tools Co., Ltd. No. 50 Dongbei Road, Dongqiao Industrial Zone, Haishu District, Ningbo, Zhejiang China Junhe Pumps Holding Co., Ltd. Wanzhong Villiage, Jishigang Town, Haishu District, Ningbo, Zhejiang China Skybest Electric Appliance (Suzhou) Co., Ltd. No. 18 Hua Hong Street, Suzhou Industrial Park, Suzhou, Jiangsu China Zhejiang Safun Industrial Co., Ltd. No. 7 Mingyuannan Road, Economic Development Zone, Yongkang, Zhejiang China Zhejiang Dingxin Arts&Crafts Co., Ltd. No. 21 Linxian Road, Baishuiyang Town, Linhai, Zhejiang China Zhejiang Natural Outdoor Goods Inc. Xiacao Village, Pingqiao Town, Tiantai County, Taizhou, Zhejiang China Guangdong Xinbao Electrical Appliances Holdings Co., Ltd. South Zhenghe Road, Leliu Town, Shunde District, Foshan, Guangdong China Yangzhou Juli Sports Articles Co., Ltd. Fudong Village, Xiaoji Town, Jiangdu District, Yangzhou, Jiangsu China Eyarn Lighting Ltd. Yaying Gang, Shixi Village, Shishan Town, Nanhai District, Foshan, Guangdong China Lipan Gift & Lighting Co., Ltd. No. 2 Guliao Road 3, Science Industrial Zone, Tangxia Town, Dongguan, Guangdong China Zhan Jiang Kang Nian Rubber Product Co., Ltd. No. 85 Middle Shen Chuan Road, Zhanjiang, Guangdong China Ansen Electronics Co. Ning Tau Administrative District, Qiao Tau Zhen, Dongguan, Guangdong China Changshu Tongrun Auto Accessory Co., Ltd. -

Spatial Distribution Pattern of Minshuku in the Urban Agglomeration of Yangtze River Delta
The Frontiers of Society, Science and Technology ISSN 2616-7433 Vol. 3, Issue 1: 23-35, DOI: 10.25236/FSST.2021.030106 Spatial Distribution Pattern of Minshuku in the Urban Agglomeration of Yangtze River Delta Yuxin Chen, Yuegang Chen Shanghai University, Shanghai 200444, China Abstract: The city cluster in Yangtze River Delta is the core area of China's modernization and economic development. The industry of Bed and Breakfast (B&B) in this area is relatively developed, and the distribution and spatial pattern of Minshuku will also get much attention. Earlier literature tried more to explore the influence of individual characteristics of Minshuku (such as the design style of Minshuku, etc.) on Minshuku. However, the development of Minshuku has a cluster effect, and the distribution of domestic B&Bs is very unbalanced. Analyzing the differences in the distribution of Minshuku and their causes can help the development of the backward areas and maintain the advantages of the developed areas in the industry of Minshuku. This article finds that the distribution of Minshuku is clustered in certain areas by presenting the overall spatial distribution of Minshuku and cultural attractions in Yangtze River Delta and the respective distribution of 27 cities. For example, Minshuku in the central and eastern parts of Yangtze River Delta are more concentrated, so are the scenic spots in these areas. There are also several concentrated Minshuku areas in other parts of Yangtze River Delta, but the number is significantly less than that of the central and eastern regions. Keywords: Minshuku, Yangtze River Delta, Spatial distribution, Concentrated distribution 1. -
![Directors and Parties Involved in the [Redacted]](https://docslib.b-cdn.net/cover/0380/directors-and-parties-involved-in-the-redacted-1580380.webp)
Directors and Parties Involved in the [Redacted]
THIS DOCUMENT IS IN DRAFT FORM, INCOMPLETE AND SUBJECT TO CHANGE. THE INFORMATION IN THIS DOCUMENT SHOULD BE READ IN CONJUNCTION WITH THE SECTION HEADED “WARNING” ON THE COVER OF THIS DOCUMENT DIRECTORS AND PARTIES INVOLVED IN THE [REDACTED] DIRECTORS Name Address Nationality Executive Directors Mr. He Binfeng (何斌鋒) Room 201, No. 28, Block 12 Chinese Lanyuan Residential Community Yening Street Fuming Sub-district Yinzhou District, Ningbo Zhejiang, PRC Mr. Zhang Qinghai (張青海) Room 501, No. 38 Donghai Garden Chinese 625 Lane Minan Road Donghai Garden Community Dongliu Sub-district Yinzhou District, Ningbo Zhejiang, PRC Mr. Huang Yu (黃宇) Room 31-11, No. 17 Chinese Block 1, Hemeicheng Square Yangmuqi Road, Xinming Sub-district National Hi-Tech Zone, Ningbo Zhejiang, PRC Mr. Wu Bin (吳濱) Room 612, No. 13, Kaiming Alley Chinese Haishu District, Ningbo Zhejiang, PRC Mr.LiDa(李達) Room 401, Unit 34, Block 6 Chinese Ge Lan Chun Chen Residential Community Chunhua Community, Jishigang Town Haishu District, Ningbo Zhejiang, PRC Mr. Chen Xiaodong (陳曉冬) Room 603, Block 45, Lane 98 Chinese North Huan Cheng Xi Road Shengfeng Community Ximen Sub-district Haishu District, Ningbo Zhejiang, PRC –65– THIS DOCUMENT IS IN DRAFT FORM, INCOMPLETE AND SUBJECT TO CHANGE. THE INFORMATION IN THIS DOCUMENT SHOULD BE READ IN CONJUNCTION WITH THE SECTION HEADED “WARNING” ON THE COVER OF THIS DOCUMENT DIRECTORS AND PARTIES INVOLVED IN THE [REDACTED] Name Address Nationality Independent Non-executive Directors Mr. Li Huamin (李華敏) Room 3204, Unit 190 Chinese Building 57, Phase III Yong Cheng Shi Jia Residential Community Xueshi Road, Nanyu Community Shounan Sub-district Yinzhou District, Ningbo Zhejiang, PRC Mr. -

K-Citymarket Factory List Updated August 20Th2018
K-Citymarket Factory list Updated August 20 th 2018 Factory name Address City Province Country Hop Yick (Bangladesh) Ltd Plot #44-46, Depz (West Zone), Ganokbari, Ashuliasavar Dhaka Bangladesh Mondol Fabrics Ltd. Nayapara, Kashimpur Gazipur Dhaka Bangladesh Parkstar Apparel Ltd Kunia, Kb Bazar,Gazipur Sador, Gazipur Dhaka Bangladesh Shangu Tex Ltd - 2 Dusaid, Ashulia, Savar, Dhaka Dhaka Dhaka Bangladesh Z&Z Intimates Ltd Plot # 1, 2, 3, Road # 02, (Factory Bay Area), Cepz, Chittagong, Chittagong Chittagong Bangladesh Tianyan International (Cambodia)Fashion Co.,Ltd Phum Khva, Sangkat Dongkor, Khan Dongkor, Phnom Penh Phnom Penh Cambodia Municipal Shang Xuan Leather Products Factory No. 6 Li He Street, Li Heng Village, Qingxi Town Dongguan Guangdong China Beijing Joywin Fashion Textile Co. Ltd. No. 3, Ying Quan Street, Yan Qing County Beijing Beijing China Kahung Luggage (Zhangzhou) Co., Ltd Jinmin Road, Beidou Industrial Zone, Jinfeng Economic Development Zone, Zhangzhou Fujian China Bole Shoes Co., Ltd No. 18, Xinya Road, Sanxi Industry Park, Ouhai, Wenzhou Zhejiang China Wenzhou Jiediya Shoes Co.Ltd Dongshou 2nd Floor, No.140, Daluoshan Road, Economic Development Wenzhou Zhejiang China Zone Wenzhou Lihui Shoes Industrial Co., Ltd Yunzhou Industrial Area, Feiyun Town, Ruian Zhejiang China Changzhou Hepu Garments Co.,Ltd No.58 Zhongxing Road,Jintan, Changzhou Jiangsu China Rugao Dingfeng Knitting Textiles Co.,Ltd No 186,Taoli Road,Xiayuan Town,Rugao, Nantong Jiangsu China Taicang Jiebin Garment And Accessory Factory 58 Gangkou Rd, Liuhe -

SUPPLIER LIST AUGUST 2019 Cotton on Group - Supplier List 2
SUPPLIER LIST AUGUST 2019 Cotton On Group - Supplier List _2 COUNTRY FACTORY NAME SUPPLIER ADDRESS STAGE TOTAL % OF % OF % OF TEMP WORKERS FEMALE MIGRANT WORKER WORKERS WORKER CHINA NINGBO FORTUNE INTERNATIONAL TRADE CO LTD RM 805-8078 728 LANE SONGJIANG EAST ROAD SUP YINZHOU NINGBO, ZHEJIANG CHINA NINGBO QIANZHEN CLOTHES CO LTD OUCHI VILLAGE CMT 104 64% 75% 6% GULIN TOWN, HAISHU DISTRICT NINGBO, ZHEJIANG CHINA XIANGSHAN YUFA KNITTING LTD NO.35 ZHENYIN RD, JUEXI STREET CMT 57 60% 88% 12% XIANGSHAN COUNTY NINGBO CITY, ZHEJIANG CHINA SUNROSE INTERNATIONAL CO LTD ROOM 22/2 227 JINMEI BUILDING NO 58 LANE 136 SUP SHUNDE ROAD, HAISHU DISTRICT NINGBO, ZHEJIANG CHINA NINGBO HAISHU WANQIANYAO TEXTILE CO LTD NO 197 SAN SAN ROAD CMT 26 62% 85% 0% WANGCHAN INDUSTRIAL ZONE NINGBO, ZHEJIANG CHINA ZHUJI JUNHANG SOCKS FACTORY DAMO VILLAGE LUXI NEW VILLAGE CMT 73 38% 66% 0% ZHUJI CITY ZHEJIANG CHINA SKYLEAD INDUSTRY CO LIMITED LAIMEI INDUSTRIAL PARK SUP CHENGHAI DISTRICT, SHANTOU CITY GUANGDONG CHINA CHUANGXIANG TOYS LIMITED LAIMEI INDUSTRIAL PARK CMT 49 33% 90% 0% CHENGHAI DISTRICT SHANTOU, GUANGDONG CHINA NINGBO ODESUN STATIONERY & GIFT CO LTD TONGJIA VILLAGE, PANHUO INDUSTRIAL ZONE SUP YINZHOU DISTRICT NINGBO CITY, ZHEJIANG CHINA NINGBO ODESUN STATIONERY & GIFT CO LTD TONGJIA VILLAGE, PANHUO INDUSTRIAL ZONE CMT YINZHOU DISTRICT NINGBO CITY, ZHEJIANG CHINA NINGBO WORTH INTERNATIONAL TRADE CO LTD RM. 1902 BUILDING B, CROWN WORLD TRADE PLAZA SUP NO. 1 LANE 28 BAIZHANG EAST ROAD NINGBO ZHEJIANG CHINA NINGHAI YUEMING METAL PRODUCT CO LTD NO. 5 HONGTA ROAD -

Brand Supplier/Agent Name COO Factory Name Factory Address
Brand Collective Overseas Supplier List - Version 4, 07 DECEMBER 2017 © Brand Collective Pty Ltd Supplier Brand Supplier/Agent name COO Factory name Factory Address Type CLARKS SHUCRAFT KAILICHENG SHOES LTD CHINA QIANG XING FOOTWEAR LTD NO.3 OF FIRST LANE LONGZHU ROAD,NANQU SHANG TANG INDUSTRIAL ZONE ,ZHONGSHAN CITY ,GUANGDONG PROVINCE AGENT CLARKS MACRO WAY INTERNATIONAL CORP. INDONESIA PT. SHOU FONG LASTINDO PANGMIAO, GANGPING TOWN, HUAJI, ZHAOQING AGENT CLARKS LINK-HO (JINJIANG) IMP. & EXP. CO., LTD. CHINA JIANJIANG JIEFU SHOES CO LTD。 CHIDIAN INDUSTRIAL ZONE, CHIDIAN TOWN JINJIANG AGENT CLARKS LINK-HO (JINJIANG) IMP. & EXP. CO., LTD. CHINA FUJIAN HONGPENG SHOES CO.,LTD YANGGUAN EAST RD. ,HUATINGKOU ,CHENDAI TOWN,JINJIANG CITY AGENT CLARKS JIALIANG INTERNATIONAL CO., LTD CHINA FUYANG FUYUAN SHOES CO.,LTD CHANGLING VILLAGE,YONGCHANG TOWN,FUYANG DISTRIC,HANGZHOU CITY,ZHEJIANG PROVINCE,CHINA AGENT CLARKS KARINDO PUTRA JAYA INDONESIA KARINDO PUTRA JAYA BYPASS KRIAN,DESA BALONG BENDO KM. 17 SIDOARJO,INDONESIA DIRECT CLARKS EVER SMART INTERNATIONAL ENTERPRISE LTD. CHINA WENZHOU JIETU(AOLUN) SHOES FACTORY NO.8 SHUANGBAO WEST ROAD, OUHAI ECONOMIC DEVELOPM P.C. 325014, WENZHOU, CHINA AGENT CLARKS EVER SMART INTERNATIONAL ENTERPRISE LTD. CHINA STRONG MAN 3515 SHOE CO LTD。 NO.197 RENMIN DONG ROAD. LUOHE HENAN,CHINA AGENT CLARKS JINJIANG XINYU SHOES CO., LTD CHINA JINJIANG XINYU SHOES CO., LTD NO.17 YONGJUN ROAD XINBIN TOWN JINJIANG CITY FUJIAN PROVINCE ,CHINA DIRECT CLARKS CORTINA CHINA LTD CHINA CORTINA CHINA LTD NIU DUN INDUSTRIAL ESTATE,HENGLI, WANG NIU DUN, DONGGUAN 523216,GUANGDONG PROVINCE,CHINA AGENT CLARKS HOME FUN SHOES CO., LTD MYANMAR MYANMAR SOE SAN WIN MANUFACTURING CO., LTD. -

Exhibitors for the 2019 International Home + Housewares Show
Exhibitors for the 2019 International Home + Housewares Show Company Name Address Category Phone, Booth # 2652 E 45th St PH 323-588-3026 26 California Bazar Wholesale Vernon, CA 90058 clean + contain Booth N6240 United States 29783 Spruce Rd PH 847-477-9093 6 Ideas, Inc. Evergreen, CO 80439 clean + contain Booth N6004 United States 14832 Arrow Hwy. PH 626-962-2990 Above All Co. Forearm Forklift Inc. Baldwin Park, CA 91706 clean + contain Booth N6061 United States 1 Mira Street, Sosnovy Bor, Leningrad Region, Russia, 188540 PH +78136973000 Abrasive Technologies, LLC clean + contain Sosnovy Bor, Leningrad Region, 188540 Booth N6565 Russian Federation Zone 3, Waterton Point Brocastle Avenue PH 44-0-1656-66 Addis Housewares, Ltd. Bridgend, CF31 3US clean + contain Booth N7143 United Kingdom 1821 N Highway CC PO Box 2310 PH 417-725-2691 Aire-Master of America, Inc. Nixa, MO 65714 clean + contain Booth N6918 United States ISTOC 9 ADA NO 1 BAGCILAR PH 90-212-659-4 AKYUZ PLASTIK A. S. ISTANBUL, 34217 clean + contain Booth N6844 Turkey Partida La Marjal, N 61 PH 34-965567319 Alberto Forte Composite, S.L. Banyeres De Mariola, Alicante, 03450 clean + contain Booth N6938 Spain PO Box 4695 PH 480-361-1573 Alliance Consumer Products SCOTTSDALE, AZ 85261 clean + contain Booth N6003 United States 210 Carpenter Dam Rd PH 501-262-2700 Alliance Rubber Company Hot Springs, AR 71903-0950 clean + contain Booth N8159 United States 3241 Winpark Dr PH 763-545-0700 AMC Sales Inc. Minneapolis, MN 55427-2023 clean + contain Booth N6859 United States PO Box 611 PH 248-669-2100 Armaly Brands Walled Lake, MI 48390-0611 clean + contain Booth N6508 United States 141 W 36th St Ste 901 PH 212-631-0300 Azzure Home NEW YORK, NY 10018 clean + contain Booth N6530 United States 8 Bellows Falls Rd PO Box 710 PH 802-387-5509 Basketville Putney, VT 05346-0710 clean + contain Booth N6106 United States 1250 E Sanborn Street PH 507-454-4664 Behrens Manufacturing Winona, MN 55987 clean + contain Booth N6453 United States No.