Apraclonidine Hydrochloride Ophthalmic Solution) 1% As Base Sterile
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Brimonidine Tartrate; Brinzolamide
Contains Nonbinding Recommendations Draft Guidance on Brimonidine Tartrate ; Brinzolamide This draft guidance, when finalized, will represent the current thinking of the Food and Drug Administration (FDA, or the Agency) on this topic. It does not establish any rights for any person and is not binding on FDA or the public. You can use an alternative approach if it satisfies the requirements of the applicable statutes and regulations. To discuss an alternative approach, contact the Office of Generic Drugs. Active Ingredient: Brimonidine tartrate; Brinzolamide Dosage Form; Route: Suspension/drops; ophthalmic Strength: 0.2%; 1% Recommended Studies: One study Type of study: Bioequivalence (BE) study with clinical endpoint Design: Randomized (1:1), double-masked, parallel, two-arm, in vivo Strength: 0.2%; 1% Subjects: Males and females with chronic open angle glaucoma or ocular hypertension in both eyes. Additional comments: Specific recommendations are provided below. ______________________________________________________________________________ Analytes to measure (in appropriate biological fluid): Not applicable Bioequivalence based on (95% CI): Clinical endpoint Additional comments regarding the BE study with clinical endpoint: 1. The Office of Generic Drugs (OGD) recommends conducting a BE study with a clinical endpoint in the treatment of open angle glaucoma and ocular hypertension comparing the test product to the reference listed drug (RLD), each applied as one drop in both eyes three times daily at approximately 8:00 a.m., 4:00 p.m., and 10:00 p.m. for 42 days (6 weeks). 2. Inclusion criteria (the sponsor may add additional criteria): a. Male or nonpregnant females aged at least 18 years with chronic open angle glaucoma or ocular hypertension in both eyes b. -
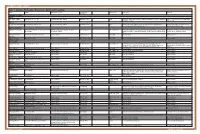
Table 1. Glaucoma Medications: Mechanisms, Dosing and Precautions Brand Generic Mechanism of Action Dosage/Avg
OPTOMETRIC STUDY CENTER Table 1. Glaucoma Medications: Mechanisms, Dosing and Precautions Brand Generic Mechanism of Action Dosage/Avg. % Product Sizes Side Effects Warnings Reduction CHOLINERGIC AGENTS Direct Pilocarpine (generic) Pilocarpine 1%, 2%, 4% Increases trabecular outflow BID-QID/15-25% 15ml Headache, blurred vision, myopia, retinal detachment, bronchiole constriction, Angle closure, shortness of breath, retinal narrowing of angle detachment Indirect Phospholine Iodide (Pfizer) Echothiophate iodide 0.125% Increases trabecular outflow QD-BID/15-25% 5ml Same as above plus cataractogenic iris cysts in children, pupillary block, Same as above, plus avoid prior to any increased paralysis with succinylcholine general anesthetic procedure ALPHA-2 AGONISTS Alphagan P (Allergan) Brimonidine tartrate 0.1%, 0.15% with Purite Decreases aqueous production, increases BID-TID/up to 26% 5ml, 10ml, 15ml Dry mouth, hypotension, bradycardia, follicular conjunctivitis, ocular irritation, Monitor for shortness of breath, dizziness, preservative uveoscleral outflow pruritus, dermatitis, conjunctival blanching, eyelid retraction, mydriasis, drug ocular redness and itching, fatigue allergy Brimonidine tartrate Brimonidine tartrate 0.15%, 0.2% Same as above Same as above 5ml, 10ml Same as above Same as above (generic) Iopidine (Novartis) Apraclonidine 0.5% Decreases aqueous production BID-TID/up to 25% 5ml, 10ml Same as above but higher drug allergy (40%) Same as above BETA-BLOCKERS Non-selective Betagan (Allergan) Levobunolol 0.25%, 0.5% Decreases -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -

NEW ZEALAND DATA SHEET 1. PRODUCT NAME IOPIDINE® (Apraclonidine Hydrochloride) Eye Drops 0.5%
NEW ZEALAND DATA SHEET 1. PRODUCT NAME IOPIDINE® (apraclonidine hydrochloride) Eye Drops 0.5%. 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each mL of Iopidine Eye Drops 0.5% contains apraclonidine hydrochloride 5.75 mg, equivalent to apraclonidine base 5 mg. Excipient with known effect Benzalkonium chloride 0.1 mg per 1 mL as a preservative. For the full list of excipients, see section 6.1. 2. PHARMACEUTICAL FORM Eye drops, solution, sterile, isotonic. 4. CLINICAL PARTICULARS 4.1. Therapeutic indications Iopidine Eye Drops 0.5% are indicated for short-term adjunctive therapy in patients on maximally tolerated medical therapy who require additional IOP reduction. Patients on maximally tolerated medical therapy who are treated with Iopidine Eye Drops 0.5% to delay surgery should have frequent follow up examinations and treatment should be discontinued if the intraocular pressure rises significantly. The addition of Iopidine Eye Drops 0.5% to patients already using two aqueous suppressing drugs (i.e. beta-blocker plus carbonic anhydrase inhibitor) as part of their maximally tolerated medical therapy may not provide additional benefit. This is because apraclonidine is an aqueous-suppressing drug and the addition of a third aqueous suppressant may not significantly reduce IOP. The IOP-lowering efficacy of Iopidine Eye Drops 0.5% diminishes over time in some patients. This loss of effect, or tachyphylaxis, appears to be an individual occurrence with a variable time of onset and should be closely monitored. The benefit for most patients is less than one month. 4.2. Dose and method of administration Dose One drop of Iopidine Eye Drops 0.5% should be instilled into the affected eye(s) three times per day. -

Drug List (SORTED by TRADE with GENERIC EQUIVALENT)
NBEO Drug List (SORTED BY TRADE WITH GENERIC EQUIVALENT) Trade Generic Trade Generic Abilify aripiprazole Avandia rosiglitazone Accolate zafirlukast Avastin bevacizumab Accupril quinapril Azasan azathioprine Achromycin tetracycline AzaSite azithromycin Aciphex rabeprazole Avodart dutasteride Actos pioglitazone Azopt brinzolamide Acular ketorolac Bactrim trimethoprim-sulfamethoxazole Acuvail ketorolac Bactrim DS trimethoprim-sulfamethoxazole Advair fluticasone propionate Baquacil polyhexamethylene biguanide Advil ibuprofen Beconase AQ beclomethasone AeroBid flunisolide Benadryl diphenhydramine Afrin oxymetazoline Bepreve Bepotastine besilate Aggrenox aspirin and dipyridamole Besivance besifloxacin Alamast pemirolast Betadine povidone-iodine Alaway ketotifen Betagan levobunolol Aldactone spironolactone Betasept chlorhexidine topical Aleve naproxen sodium Betaseron interferon beta-1b Allegra fexofenadine Betimol timolol Allegra-D fexofenadine-pseudoephedrine Betoptic S betaxolol Alluvia lopinavir Biopatch chlorhexidine topical Alocril nedocromil Blephamide sulfacetamide-prednisolone Alomide lodoxamide Botox onabotulinum toxinA Alphagan P brimonidine Brolene propamidine isethionate Alrex loteprednol 0.2% Bromday bromfenac Ambien zolpidem Calamine zinc oxide and iron oxide Amicar aminocaproic acid Calan verapamil Amoxil amoxicillin Calgon Vesta chlorhexidine topical Amphocin amphotericin B Capoten captopril Anectine succinylcholine Carafate sucralfate Ansaid flurbiprofen Carbocaine mepivacaine HCl injection Antivert meclizine Cardizem diltiazem -

IOPIDINE® 0.5% (Apraclonidine Ophthalmic Solution) 0.5% As Base
IOPIDINE® 0.5% (apraclonidine ophthalmic solution) 0.5% As Base DESCRIPTION: IOPIDINE® 0.5% Ophthalmic Solution contains apraclonidine hydrochloride, an alpha adrenergic agonist, in a sterile isotonic solution for topical application to the eye. Apraclonidine hydrochloride is a white to off-white powder and is highly soluble in water. Its chemical name is 2-[(4-amino-2,6 dichlorophenyl) imino]imidazolidine monohydrochloride with an empirical formula of C9H11Cl3N4 and a molecular weight of 281.57. The chemical structure of apraclonidine hydrochloride is: Each mL of IOPIDINE 0.5% Ophthalmic Solution contains: Active: apraclonidine hydrochloride 5.75 mg equivalent to apraclonidine base 5 mg; . Inactives: sodium chloride, sodium acetate, sodium hydroxide and/or hydrochloric acid (pH 4.4-7.8), purified water and benzalkonium chloride 0.01% (preservative) CLINICAL PHARMACOLOGY: Apraclonidine hydrochloride is a relatively selective alpha- 2-adrenergic agonist. When instilled in the eye, IOPIDINE 0.5% Ophthalmic Solution, has the action of reducing elevated, as well as normal, intraocular pressure (IOP), whether or not accompanied by glaucoma. Ophthalmic apraclonidine has minimal effect on cardiovascular parameters. Elevated IOP presents a major risk factor in glaucomatous field loss. The higher the level of IOP, the greater the likelihood of optic nerve damage and visual field loss. IOPIDINE 0.5% Ophthalmic Solution has the action of reducing IOP. The onset of action of apraclonidine can usually be noted within one hour, and maximum IOP reduction occurs about three hours after instillation. Aqueous fluorophotometry studies demonstrate that apraclonidine's predominant mechanism of action is reduction of aqueous flow via stimulation of the alpha-adrenergic system. -

Glaucoma Medical Treatment: Philosophy, Principles and Practice
Glaucoma medical CLIVE MIGDAL treatment: philosophy, principles and practice Abstract assessment of these parameters. Indeed There have been numerous recent advances in compounds are under evaluation that affect the the management of glaucoma, not least the function of the optic nerve (via improved blood development of new drugs to help manage supply or improved neuronal cell physiology) raised intraocular pressure. In addition, the but may or may not lower lOP. It may even be concepts of improving blood flow to the optic possible in the future to therapeutically alter the nerve head and neuroprotection are currently human genome, genetically deliver provoking considerable interest. This article neuroprotective substances or aid regeneration considers the aims and philosophy of of the optic nerve axons. glaucoma drug therapy, summarises some of The main aim of glaucoma therapy must still the basic facts and principles of modem be the preservation of visual function. At the glaucoma medications, and suggests a same time, the therapy should not have adverse practical approach to the choice of therapy. side effects and should not affect the quality of life of the patient (by causing either side effects Key words Blood flow, Intraocular pressure, or inconvenience and disruption of daily Neuroprotection, Primary open angle glaucoma, Topical medications lifestyle). The cost of the therapy, both direct and indirect, must also be taken into consideration.s Currently, typical glaucoma management Philosophy consists of lowering the lOP to a satisfactory Primary open-angle glaucoma is a complex and safe target leve1.6 To determine the success disease for which a number of risk factors have of this treatment, the patient must be followed been identified, including intraocular pressure, long-term with routine assessment of lOP, discs age, race and family history.l,2 Due to our and fields to exclude progressive damage. -

REMEDY for GLAUCOMA COMPRISING Rho KINASE INHIBITOR and -BLOCKER
Europäisches Patentamt *EP001568382A1* (19) European Patent Office Office européen des brevets (11) EP 1 568 382 A1 (12) EUROPEAN PATENT APPLICATION published in accordance with Art. 158(3) EPC (43) Date of publication: (51) Int Cl.7: A61K 45/06, A61K 31/138, 31.08.2005 Bulletin 2005/35 A61K 31/343, A61K 31/353, A61K 31/437, A61K 31/4409, (21) Application number: 03772800.3 A61K 31/4412, A61K 31/496, (22) Date of filing: 17.11.2003 A61K 31/5377, A61K 31/551, A61P 27/06, A61P 43/00 (86) International application number: PCT/JP2003/014559 (87) International publication number: WO 2004/045644 (03.06.2004 Gazette 2004/23) (84) Designated Contracting States: • NAKAJIMA, Tadashi AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Ikoma-shi, Nara 630-0101 (JP) HU IE IT LI LU MC NL PT RO SE SI SK TR • MATSUGI, Takeshi Designated Extension States: Ikoma-shi, Nara 630-0101 (JP) AL LT LV MK • HARA, Hideaki Ikoma-shi, Nara 630-0101 (JP) (30) Priority: 18.11.2002 JP 2002333213 (74) Representative: Peaucelle, Chantal et al (71) Applicant: SANTEN PHARMACEUTICAL CO., Cabinet Armengaud Ainé LTD. 3, avenue Bugeaud Osaka 533-8651 (JP) 75116 Paris (FR) (72) Inventors: • HATANO, Masakazu Ikoma-shi, Nara 630-0101 (JP) (54) REMEDY FOR GLAUCOMA COMPRISING Rho KINASE INHIBITOR AND &bgr;-BLOCKER (57) A subject of the present invention is to find utility of a co mbination of a Rho kinase inhibitor having a novel action and a β-blocker as a therapeutic agent for glau- coma. -

2021 Formulary List of Covered Prescription Drugs
2021 Formulary List of covered prescription drugs This drug list applies to all Individual HMO products and the following Small Group HMO products: Sharp Platinum 90 Performance HMO, Sharp Platinum 90 Performance HMO AI-AN, Sharp Platinum 90 Premier HMO, Sharp Platinum 90 Premier HMO AI-AN, Sharp Gold 80 Performance HMO, Sharp Gold 80 Performance HMO AI-AN, Sharp Gold 80 Premier HMO, Sharp Gold 80 Premier HMO AI-AN, Sharp Silver 70 Performance HMO, Sharp Silver 70 Performance HMO AI-AN, Sharp Silver 70 Premier HMO, Sharp Silver 70 Premier HMO AI-AN, Sharp Silver 73 Performance HMO, Sharp Silver 73 Premier HMO, Sharp Silver 87 Performance HMO, Sharp Silver 87 Premier HMO, Sharp Silver 94 Performance HMO, Sharp Silver 94 Premier HMO, Sharp Bronze 60 Performance HMO, Sharp Bronze 60 Performance HMO AI-AN, Sharp Bronze 60 Premier HDHP HMO, Sharp Bronze 60 Premier HDHP HMO AI-AN, Sharp Minimum Coverage Performance HMO, Sharp $0 Cost Share Performance HMO AI-AN, Sharp $0 Cost Share Premier HMO AI-AN, Sharp Silver 70 Off Exchange Performance HMO, Sharp Silver 70 Off Exchange Premier HMO, Sharp Performance Platinum 90 HMO 0/15 + Child Dental, Sharp Premier Platinum 90 HMO 0/20 + Child Dental, Sharp Performance Gold 80 HMO 350 /25 + Child Dental, Sharp Premier Gold 80 HMO 250/35 + Child Dental, Sharp Performance Silver 70 HMO 2250/50 + Child Dental, Sharp Premier Silver 70 HMO 2250/55 + Child Dental, Sharp Premier Silver 70 HDHP HMO 2500/20% + Child Dental, Sharp Performance Bronze 60 HMO 6300/65 + Child Dental, Sharp Premier Bronze 60 HDHP HMO -

Penetration Enhancers in Ocular Drug Delivery
pharmaceutics Review Penetration Enhancers in Ocular Drug Delivery Roman V. Moiseev 1 , Peter W. J. Morrison 1 , Fraser Steele 2 and Vitaliy V. Khutoryanskiy 1,* 1 Reading School of Pharmacy, University of Reading, Whiteknights, P.O. Box 224, Reading RG66AD, UK 2 MC2 Therapeutics, James House, Emlyn Lane, Leatherhead KT22 7EP, UK * Correspondence: [email protected]; Tel.: +44-(0)-118-378-6119 Received: 30 May 2019; Accepted: 3 July 2019; Published: 9 July 2019 Abstract: There are more than 100 recognized disorders of the eye. This makes the development of advanced ocular formulations an important topic in pharmaceutical science. One of the ways to improve drug delivery to the eye is the use of penetration enhancers. These are defined as compounds capable of enhancing drug permeability across ocular membranes. This review paper provides an overview of anatomical and physiological features of the eye and discusses some common ophthalmological conditions and permeability of ocular membranes. The review also presents the analysis of literature on the use of penetration-enhancing compounds (cyclodextrins, chelating agents, crown ethers, bile acids and bile salts, cell-penetrating peptides, and other amphiphilic compounds) in ocular drug delivery, describing their properties and modes of action. Keywords: ocular drug delivery; cornea; penetration enhancers; ocular conditions; ophthalmology 1. Introduction According to the World Health Organization, the number of people who live with some form of distance or near vision impairment is about 1.3 billion worldwide [1]. This problem is very important because approximately 80% of external input of information delivered to the brain is processed by the visual pathway [2]. -

Short-Term Effect of Topical Antiglaucoma Medication on Tear-Film Stability, Tear Secretion, and Corneal Sensitivity in Healthy Subjects
Clinical Ophthalmology Dovepress open access to scientific and medical research Open Access Full Text Article ORIGINAL RESEARCH Short-term effect of topical antiglaucoma medication on tear-film stability, tear secretion, and corneal sensitivity in healthy subjects Naim Terai Background: The purpose of this study was to investigate the short-term effect of topical Matthias Müller-Holz antiglaucoma medication on tear-film stability, tear secretion, and corneal sensitivity in healthy Eberhard Spoerl subjects. Lutz E Pillunat Methods: In this prospective, double-blind crossover trial, break-up time and basal secretion (Jones test) were measured 60 minutes before, and 30, 60, and 90 minutes after topical Department of Ophthalmology, Carl Gustav Carus University Hospital, antiglaucoma drop application in 30 healthy subjects. Corneal sensitivity was measured Dresden, Germany 60 minutes before, and five, 10, and 15 minutes after drop application using a Cochet–Bonnet esthesiometer. Results: Reduction of break-up time in the latanoprost group was -23.8% after 30 minutes (P = 0.21), -26.7% after 60 minutes (P = 0.03) and -51.4% after 90 minutes (P # 0.003), which was statistically significant. Reduction of break-up time in all other treatment groups was not statistically significant. The Jones test revealed a significant reduction of basal secretion after application of brimonidine (-17.8%, P = 0.002; -22.5%, P , 0.001; -30.5%, P , 0.001), fol- lowed by apraclonidine (-10%, P = 0.06; -20.1%, P = 0.02; -22.1%, P = 0.002), latanoprost (-2.4%, P = 0.64; -18.6%, P = 0.001; -20.1%, P = 0.001) and dorzolamide (-0.5%, P = 0.9; 14.3%, P = 0.018; -17.3%, P = 0.004) at 30, 60, and 90 minutes after drop application. -

Sympatholytic Drugs
SYMPATHOLYTIC DRUGS ADRENERGIC ADRENERGIC NEURON RECEPTOR BLOCKERS BLOCKERS ADRENALINE REVERSAL Sir Henry Dale, awarded the Nobel prize in 1936 §ILOS Outline the mechanisms of action of adrenergic neuron blockers Classify a-receptor blockers into selective & non- selective §Study in detail the pharmacokinetic aspects & pharmacodynamic effects of a adrenergic blockers MECHANISMS OF ADRENERGIC BLOCKERS §1-Formation of False Transmitters a-Methyl dopa MECHANISMS OF ADRENERGIC BLOCKERS §2-Depletion of Storage sites Reserpine MECHANISMS OF ADRENERGIC BLOCKERS §3-Inhibition of release Guanethidine MECHANISMS OF ADRENERGIC BLOCKERS §4-Stimulation of presynaptic a2 receptors Clonidine and a-Methyldopa a-Methyldopa §Forms false transmitter that is released instead of NE §Acts centrally as a2 receptor agonist to inhibit NE release Drug of choice in the treatment of hypertension in pregnancy (pre- eclampsia - gestational hypertension) Clonidine §Apraclonidine §Acts directly as a2 receptor is used in open agonist to inhibit NE release angle glaucoma as eye drops. Suppresses sympathetic acts by outflow activity from the brain decreasing aqueous humor Little Used as Antihypertensive agent due to formation rebound hypertension upon abrupt withdrawal Adrenergic SYNOPSIS neuron blockers Stimulation of False Depletion of Inhibition of neurotransmit stores release presynaptic α- ter formation receptors Clonidine α-Methyldopa Reserpine Guanethidine α-Methyldopa ADRENERGIC RECEPTOR BLOCKERS They block sympathetic actions by antagonizing:- §a-receptor §β-receptor