Performance Audit Union Government Reproductive and Child
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

DISTRICT : Champaran-W
District District District District District Sl. No. Name of Husband's/Father,s AddressDate of Catego Full Marks Percent Choice-1 Choice-2 Choice-3 Choice-4 Choice-5 Candidate Name Birth ry Marks Obtained age (With Rank) (With Rank) (With Rank) (With Rank) (With Rank) DISTRICT : Champaran-W 1 PUSHPASRI NARENDRA w/o- narendra kumar 06-Feb-72 BC 900 675 75 Nawada (21) Saharsa (6) Champaran-W Patna (35) Purnia (6) KUMAR vill- jagatpur (1) post- harnaut dist- nalanda pin code- 803110 2 RENU KUMARISRI SURENDRA c/o sri surendra prasad 05-Feb-69 BC 900 672 74.67 Nalanda (32) Kaimur (3) Jahanabad (25) Gaya (24) Champaran-W (2) PRASAD SINGH singh, village+post khaddi lodipur, via- akanger sarai, district- nalanda, bihar pin 801301 3 KUMARI APARNA ASHOK KUMAR vill- bhojit pur, post- 16-Apr-83 BC 700 511 73 Champaran-E (7) Champaran-W Madhubani (2) Darbhanga (13) Muzaffarpur (23) PRIYA ekangar sarai, dist- (3) nalanda. 4RINA KUMARISRI KUMAR MAHTO d/o sri kumar mahto, 08-Dec-83 SC 500 365 73 Champaran-E (6) Champaran-W Sitamarahi (8) Madhubani (4) Patna (69) village- sakhuanwan, (4) post- gounoli, p.s. walmiki nagar, district- pachim champaran, bihar pin 845107 5RINA KUMARIMANOJ KUMAR vill- muzaffarpur, post- 28-Oct-88 BC 700 508 72.57 Champaran-E (8) Champaran-W Madhubani (5) Darbhanga (16) Samastipur (29) kathoule, disst- nalanda. (5) 6 SUCHITRA VIKASH PRASAD w/o- vikash prasad, 08-Feb-83 BC 700 507 72.43 Champaran-W Champaran-E (9) Madhubani (8) Darbhanga (18) Samastipur (32) KUMARI vill+post- ajnaura, (6) nalanda 7KUMARI SRI AMRESH musahari nagin -

The RTE Is on the Verge of Celebrating Seven Years of Completion, Its Performance and Implementation Has Been Poor
ISSN (Online) - 2349-8846 Has the Right to Education Been Realised in Jharkhand? SUJIT KUMAR CHOUDHARY Sujit Kumar Choudhary ([email protected]) is at the School of Humanities and Social Sciences, Central University of Jharkhand, Ranchi. This article is based on a Research Study sponsored by National Institute of Educational Planning and Administration (NIEPA), New Delhi. Vol. 53, Issue No. 5, 03 Feb, 2018 This article focuses on the status of implementation of various provisions of the Right of Children to Free and Compulsory Education Act in six tribal-dominated districts in Jharkhand. The state of Jharkhand was formed on 15 November 2000. According to the 2011 census, the population of the state was 3.29 crores and the literacy rate was 67.63%. There are 44,835 schools in the state—40,343 are government schools and 4,492 are private schools. Jharkhand adopted the Right of Children to Free and Compulsory Education (RTE) Act in 2011 by specifying its own rules and regulations extracted from the original version of the act passed by the parliament. Although the RTE is on the verge of celebrating seven years of completion, its performance and implementation has been poor. Many studies and reports have confirmed the poor performance of the act at all levels of schooling. Children belonging to disadvantaged groups—Scheduled Castes (SCs), Scheduled Tribes (STs), and those below poverty line (BPL)—face problems and do not get admission in private unaided schools, despite 25 per cent of seats being reserved for them. It is thus important to analyse the District Information System for Education (DISE) data on the ISSN (Online) - 2349-8846 performance of the RTE indicators in different schools located in six tribal-dominated districts of Jharkhand and compare them. -

Annual Report 2009-2010
Annual Report 2009-2010 CENTRAL GROUND WATER BOARD MINISTRY OF WATER RESOURCES GOVERNMENT OF INDIA FARIDABAD CENTRAL GROUND WATER BOARD Ministry of Water Resources Govt. of India ANNUAL REPORT 2009-10 FARIDABAD ANNUAL REPORT 2009 - 2010 CONTENTS Sl. CHAPTERS Page No. No. Executive Summary I - VI 1. Introduction 1 - 4 2. Ground Water Management Studies 5 - 51 3. Ground Water Exploration 52 - 78 4. Development and Testing of Exploratory Wells 79 5. Taking Over of Wells by States 80 - 81 6. Water Supply Investigations 82 - 83 7. Hydrological and Hydrometereological Studies 84 - 92 8. Ground Water Level Scenario 93 - 99 (Monitoring of Ground Water Observation Wells) 9. Geophysical Studies 100- 122 10. Hydrochemical Studies 123 - 132 11. High Yielding Wells Drilled 133 - 136 12. Hydrology Project 137 13. Studies on Artificial Recharge of Ground Water 138 - 140 14. Mathematical Modeling Studies 141 - 151 15. Central Ground Water Authority 152 16. Ground Water Studies in Drought Prone Areas 153 - 154 17. Ground Water Studies in Tribal Areas 155 18. Estimation of Ground Water Resources 156 - 158 based on GEC-1997 Methodology 19. Technical Examination of Major/Medium Irrigation Schemes 159 Sl. CHAPTERS Page No. No. 20. Remote Sensing Studies 160 - 161 21. Human Resource Development 162 - 163 22. Special Studies 164 - 170 23. Technical Documentation and Publication 171 - 173 24. Visits by secretary, Chairman CGWB , delegations and important meetings 174 - 179 25. Construction/Acquisition of Office Buildings 180 26. Dissemination and Sharing of technical know-how (Participation in Seminars, 181 - 198 Symposia and Workshops) 27. Research and Development Studies/Schemes 199 28. -

Ranchi from East Singhbhum, the 14.07 Lakh of Them
" !"#$%&' ()$#$%&'% $%&%$&' $()*+ $(,-. .!&0$ -76 - 63- -15 - 39 9 - 1 23 43 414 - 3093 33 673 03 8 9 1-35 - 9 1 5 1 6 4 7 8 6 *( ( + ,+ * -.)( ''! ! " #$%!&'&'()&* Q (-! $ !$ '$ !' $' '! !+ " ! "# $$% &'!( '') $ * + + $ ** % $ more crucial responsibility... members too will send out a just like the faith with which message in unanimous voice, ith nearly 30 MPs testing they (soldiers) are standing, spirit and resolve that the coun- harkhand reported a higher Wpositive, dozens of others determined to protect moth- try stands in support of them”, Jnumber of Covid-19 recov- staying out for fear of catching erland, Parliament and all its Modi said. eries than fresh cases for the coronavirus, visitors barred, fifth consecutive day on the number of media persons Monday, taking the Covid restricted, and strict social dis- recovery rate in the state fur- tancing norms in place, the ther up to 76.68 per cent, fig- Monsoon Session of ures released by the health Parliament began on a subdued department on Monday late note on Monday. night highlighted. However, there is hope of As per figures with the action on Tuesday, as ! health department, as many as Government sources said 1263 people were found infect- Defence Minister Rajnath Parliament test for Covid and ed by the virus across Singh may address Parliament genome test it’s confirmed that Jharkhand on Monday, while on the India-China border row n the mandatory test con- I have tested positive for the 1529 Covid patients recovered +$ ) & ,-. on Tuesday. The Opposition Iducted by Parliament as virus. I am currently in good from the infection and were $)/01 $ % $ % 2 has been raising this issue for Parliament will send out a an hour, shortly after it met, fol- many 30 MPs have been found health & spirits. -

Friday 23 January 2015 Issued By
Friday 23rd January 2015 (For the period 23rd to 27th January 2015) Issued by National Agrometeorological Advisory Service Centre, Agricultural Meteorology Division, India Meteorological Department, Shivajinagar, Pune. Standardised Precipitation Index Four Weekly for the Period 25th December 2014 to 21st January 2015 Extremely/severely wet conditions in few districts of Madhya Pradesh; Satna district of Bihar; Ratnagiri, Mumbai Suburban, Akola, Amravati and Buldhana districts of Maharastra and Bangalore rural district of Karnataka. Extremely/ moderately/ severely dry conditions experienced in Udhampur, Kupwara and Rajouri districts of Jammu & Kashmir; Champa district of Himachal Pradesh; Gumla district of Jharkhand; Lakhimpur district of Assam; Papumpara, Upper Subansiri and East Kameng districts of Arunachal Pradesh and Lakshadweep. Rest of the country experienced moderately wet/ mild wet/dry conditions. Contour maps for Mean Maximum and Minimum Temperature and their anomaly for the week ending on 21.01.2015 Actual Mean Maximum Temperature (oC) in India for the Mean Maximum Temperature (oC) Anomaly in India for week ending 21.01.2015 the week ending 21.01.2015 32 to 360C over Lakshadweep Islands and many 4 to 60C over isolated parts of Arunachal Pradesh, places over Kerala and isolated places over Tamil Assam and Jammu & Kashmir. Nadu. 2 to 40C over many parts of Arunachal Pradesh, 28 to 320C over Konkan & Goa, Coastal & North Nagaland, few parts of Jammu & Kashmir, Interior Karnataka, many parts of Madhya Himachal Pradesh, Assam and isolated parts of Maharashtra, Marathwada, Andhra Pradesh, South Manipur. Interior Karnataka, Tamil Nadu, few parts of Gujarat, 0 to 20C over Telangana, Mizoram, Lakshadweep Vidarbha, Chhattisgarh and Kerala. -

East Singhbhum District, Jharkhand State
भजू ल सचू ना पस्ु तिका डﴂभूम जिला, झारख ﴂपूर्बी स घ Ground Water Information Booklet East Singhbhum District, Jharkhand State AUTO FLOW BORE WELL LOCATED AT VILLAGE KUDADA के न्द्रीय भूमिजल बो셍 ड Central Ground water Board जल संसाधन िंत्रालय Ministry of Water Resources (भारि सरकार) रा煍य एकक कायाडलय, रााँची (Govt. of India) िध्य-पर्वू ी क्षेत्र State Unit Office,Ranchi पटना Mid-Eastern Region Patna मसिंबर 2013 September 2013 1 भूजल सूचना पुस्तिका डﴂभूम जिला, झारख ﴂपूर्बी स घ Ground Water Information Booklet East Singhbhum District, Jharkhand State Prepared By ुनिल टोꥍपो (वैज्ञानिक ख ) Sunil Toppo (Scientist B) रा煍य एकक कायाडलय, रााँची िध्य-पूर्वी क्षेत्र,पटना State Unit Office, Ranchi Mid Eastern Region, Patna 2 GROUND WATER INFORMATION OF EAST SINGHBHUM DISTRICT, JHARKHAND STATE Contents Sr. Chapter Pages No. 1.0 Introduction 8 1.1 Introduction 8 1.2 Demography 9 1.3 Physiography and Drainage 9 1.4 Irrigation 10 1.5 Previous Studies 10 2.0 2.0 Climate and rainfall 11 3.0 3.0 Soil 11 4.0 4.0 Geology 11 5.0 Ground Water Scenario 13 5.1 Hydrogeology 13 5.1.1 Depth to water level 13 5.1.2 Seasonal fluctuation 14 5.1.3 Exploratory wells 14 5.1.4 Long term water level trend 14 5.2 Ground water resource 15 5.3 Ground Water Quality 15 5.4 Status of ground water development 15 6.0 Ground water management strategy 16 6.1 Ground water development 16 6.2 Water conservation and artificial recharge 16 7.0 Ground water related issue and problems 17 8.0 Awareness and training activity 17 8.1 The mass awareness programme (MAP) 17 8.2 Participation in exhibition, mela, fair etc. -

One Page.Cdr
if=dk Quarterly publication of Central TB Division Issue 1: Jul-Sep 2018 Volume: 03 Dear Readers, HIGHTLIGHTS OF THIS ISSUE: One of the most important objectives of “Nikshay Patrika” is to A. Editorial have a platform to showcase ------------------------------------------ efforts of health workers and also B. Patient’s Corner ------------------------------------------ the nameless TB Champions in the Editorial C. Logistics Management community who are working Through Portal shoulder to shoulder with us with ------------------------------------------ complete commitment and passion D. Strengthening Diagnosis to eradicate this menace of TB. Through CBNAAT ------------------------------------------ Community engagement is a force E. New TB Drug: Delanamid to reckon with which if tapped can ------------------------------------------ increase the local response to TB F. TB Awareness and Screening prevention and control manifolds. Camp, Telangana. ------------------------------------------ I would take this opportunity to G. Elected Representatives in Yadadri, District to end tb by express my gratitude to all those 2025 community volunteers whose ------------------------------------------ endless dedication and efforts have H. Social Media Campaign made a big impact in our fight ------------------------------------------ against tuberculosis. I. TB Eliminator B. PATIENT CORNER I. “TB-MUKT VAHINI”: TB SURVIVORS' NETWORK of BIHAR TB Champions of the growing TB Mukt Vahini network in Bihar undertook many activities in different districts of state -

Area(S) of Specialization: Biodiversity, Conservation and Ethnobotany
PROFILE Name: Sanjeev Kumar Address: Sanjeev Kumar, IFS Conservator of Forests Working Plan Circle Van Bhawan Jamshedpur-831011, Jharkhand Mobile: 09431120165 Phone (o): 0657-2222643 Email id- [email protected] Qualification : M.Sc. in Botany, year-1992, from University of Allahabad. Occupation/Designation/Service: Indian Forest Service: 1992 batch. Cadre: Jharkhand Area(s) of Specialization : Biodiversity, Conservation and Ethnobotany Postings : Valmiki Tiger Project, W. Champaran, Bihar (as probationer), served in Jamui (Bihar), Gumla, Ranchi, Dhanbad, Bokaro, E. Singhbhum (Jamshedpur) as Divisional Forest Officer; C.F. Afforestation and Social Forestry Circle, Jamshedpur. Presently posted as Conservator of Forests, Working Plan, and Jamshedpur. Publications I. Books Ethnobotanical Studies in India (2014, foreword by Dr. S.K.Jain) II. Booklets Published: i) On Cultivation of Lac- 1. RANGINI LAH KI KHETI, Ek Margdarshika-( year2010) 2. Lah Ki Kheti, Kyon? Kaise?-(year2011) ii) On Wealth from Waste (Fly Ash) Industrial Waste and Livelihood (Year 2011) III. List of Papers / Abstracts Published- 1. ETHNOBOTANICAL STUDIES IN GAYA DISTRICT, (BIHAR) - A REPORT ON HERBAL MEDICINES. (Paper presented and published in the proceedings of Indian Science Congress Association-1989) 2. CYTOGENETICS IN SANSKRIT LITERATURE (Paper presented and published in the proceedings of Indian Science Congress Association-1991, Botany Section.) 3. A STUDY ON METHANOGENS (Paper presented and published in the proceeding of Indian Science Congress Association-1992, Botany Section.) 4. TREE WORSHIP IN SANSKRIT LITERATURE (Paper presented and published in the proceedings of Indian Science Congress Association-1999) 5. ETHNOBOTANICAL STUDIES IN VALMIKI TIGER RESERVE, WEST CHAMPARAN, BIHAR (Paper presented and published in the proceedings of Indian Science Congress Association-1999) 6. -

District Environment Plan of Gumla District
District Environment Plan of Gumla District Gumla Let’s make Green Gumla DISTRICT ADMINSTRATION 1 | P a g e District Environment Plan, Gumla. 2 | P a g e District Environment Plan, Gumla. INTRODUCTION Hon‘ble National Green Tribunal in O.A. No. 360/2018 dated: 26/09/2019 ordered regarding constitution of District Committee (as a part of District Planning Committee under Articles 243 ZD) under Articles 243 G, 243 W, 243 ZD read with Schedules 11 and 12 and Rule 15 of the Solid Waste Management Rules, 2016. In the above said order, it is stated that among others ‘Chief Secretaries may personally monitor compliance of environmental norms (including BMW Rules) with the District Magistrate once every month. The District Magistrates may conduct such monitoring twice every month. We find it necessary to add that in view of Constitutional provisions under Articles 243 G, 243 W, 243 ZD read with Schedules 11 and 12 and Rule 15 of the Solid Waste Management Rules, 2016 it is necessary to have a District Environment Plan to be operated by a District committee (as a part of District Planning Committee under Article 243 ZD) In this regard, Principal Secretary to Government Forest, Environment & Climate Change department vide letter no. 487 dated 07.02.2020, Special Secretary to Government Forest, Environment & Climate Change department vide letter no. 4869 dated 26.12.2019 and Deputy Secretary to Government Forest, Environment & Climate Change department vide letter no. 4871 dated 26.12.2019 and letter no. 1660 dated 24.06.2020 requested Member secretary of the District Environment committee to prepare District Environmental Plans. -

Map Profile 2001 India States and Union Territories
CENSUS OF INDIA 2001 MAP PROFILE 2001 INDIA STATES AND UNION TERRITORIES Technical Direction Dr. R.P. Singh Deputy Registrar General (Map) General Direction REGISTRAR GENERAL & CENSUS COMMISSIONER, INDIA Data Product Number 00-120-2001 (Map Profile) The maps included in this publication are based upon Survey of India map with the permission of the Surveyor General of India. The territorial waters of India extend into the sea to a distance of twelve nautical miles measured from the appropriate base line. The interstate boundaries between Arunachal Pradesh, Assam and Meghalaya shown in this publication are as interpreted from the North-Eastern Areas (Reorganisation) Act, 1971 but have yet to be verified. © Government of India, Copyright 2004 (ii) PREFACE here are a number of publications undertaken during the Census of India 2001, some of which T are based on 'Census Tabulation Plan', whereas others are special monograph. The present publication is one of the 'Map Product' undertaken during the C'e~'sus of I~dia 2001. The idea for publication of such a volume was conceived while interacting with data users. Many of.them expressed the need of a reference census volume containing maps along with basic census data and administrative units information required for ready consultation purposes in one compendium. This work is an effort in that direction. The present volume covers the basic census data of the State and Union territories and associated maps for Census of India 2001. The first map shows India with the State and Union territories and subsequent maps relate with 35 States and Union territories depicting the boundaries at district and s.ub-district level. -
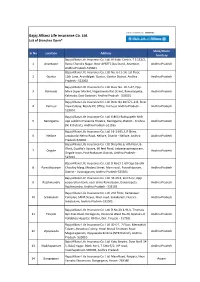
Bajaj Allianz Life Insurance Co. Ltd. List of Branches Open*
Bajaj Allianz Life Insurance Co. Ltd. List of Branches Open* State/Union Sr No Location Address Territory Bajaj Allianz Life Insurance Co. Ltd. Al-Kabir Center, T.S.151/2, 1 Anantapur Rama Chandra Nagar, Near APSRTC Bus Stand, Anantpur, Andhra Pradesh Andhra Pradesh-515001 Bajaj Allianz Life Insurance Co. Ltd. No. 6-11-14, 1st Floor, 2 Guntur 11th Lane, Arundalpet, Guntur, Guntur District, Andhra Andhra Pradesh Pradesh - 522002 Bajaj Allianz Life Insurance Co. Ltd. Door No. 10-5-47, Opp. 3 Kakinada More Super Market, Nageshwara Rao Street, Ramaraopeta, Andhra Pradesh Kakinada, East Godavari, Andhra Pradesh - 533001 Bajaj Allianz Life Insurance Co. Ltd. Door No.40/37,L-2-B, River 4 Kurnool View Colony, Beside LIC Office, Kurnool, Andhra Pradesh - Andhra Pradesh 518004. Bajaj Allianz Life Insurance Co. Ltd. 6-86/1 Ruthyupeth NH9, 5 Nandigama opp Lakshmi Prasanna Theatre, Nandigama, District - Krishna Andhra Pradesh (NTR District), Andhra Pradesh-521185 Bajaj Allianz Life Insurance Co. Ltd. 16-1-655, L R Shine, 6 Nellore Jawaharlal Nehru Road, Nellore, District - Nellore, Andhra Andhra Pradesh Pradesh-524001 Bajaj Allianz Life Insurance Co. Ltd. Shop No.6, 4th Floor, B- Block, Guptha's Square, 60 feet Road, Satyanarayanapuram, 7 Ongole Andhra Pradesh OngoleTown, Post Prakasam District, Andhra Pradesh - 523001 Bajaj Allianz Life Insurance Co. Ltd. D No13-1-69 Opp Gandhi 8 Parvathipuram Choultry Marg, Medara Street, Main road , Parvathipuram, Andhra Pradesh District - Vizianagaram, Andhra Pradesh-535501 Bajaj Allianz Life Insurance Co. Ltd. 46-20-2, 2nd floor, Opp 9 Rajahmundry corporation bank, near china Ramalayam, Danavaipeta. Andhra Pradesh Rajahmundry, Andhra Pradesh - 533103 Bajaj Allianz Life Insurance Co. -

Ranchi, Khunti and Lohardagga Districts, Jharkhand
Draft Report कᴂ द्रीय भूमम जल बो셍 ड जऱ संसाधन, नदी विकास और गंगा संरक्षण मंत्राऱय भारत सरकार Central Ground Water Board Ministry of Water Resources, River Development and Ganga Rejuvenation Government of India Report on NATIONAL AQUIFER MAPPING AND MANAGEMENT PLAN Parts of Ranchi, Khunti and Lohardagga Districts, Jharkhand रा煍य एकक कायााऱय रांची State Unit Office, Ranchi CENTRAL GROUND WATER BOARD Ministry of Water Resources, River Development & Ganga Rejuvenation Government of India REPORT ON NATIONAL AQUIFER MAPPING AND MANAGEMENT PLAN FOR JHARKHAND STATE PHASE - I CENTRAL GROUND WATER BOARD SUO, RANCHI July, 2016 Central Ground Water Board Ministry of Water Resources, River Development & Ganga Rejuvenation Government of India REPORT ON NATIONAL AQUIFER MAPPING AND MANAGEMENT PLAN FOR JHARKHAND STATE PHASE - I Data processing & preparation by T.B.N SINGH,Scientist “D” B.K. ORAON Sc -“D” Geophysicist SUNIL TOPPO Scientist-“B” Dr. ANUKARAN KUJUR, AHG ATUL BECK, AHG SUO RANCHI July, 2016 Contents NATIONAL AQUIFER MAPPING AND MANAGEMENT PLAN FOR PHASE-I JHARKHAND STATE Chapter Title Page No. No 1.1 Objectives, Scope of the study, Approach & 1 Methodology 1.2 Area details & Demography 3 1.3 Data availability, Data Gap analysis & Data 4 Generation 1.4 Rainfall 6 1.5 Geomorphology 6 1. Introduction 1.6 Land use 7 1.7 Soil 8 1.8 Hydrology 8 1.9 Drainage 8 1.10 Irrigation 10 1.11 Cropping Pattern 11 2.0 Data Collection & Generation 12 2.1 Hydrogeological Studies 12 2.2 Depth to water level 12 Data Collection & 2.