Brain Invasion and the Risk of Seizures in Patients with Meningioma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Archives - Search
Current Auctions Navigation All Archives - Search Category: ALL Archive: BIDDING CLOSED! Over 150 Silver Age Comic Books by DC, Marvel, Gold Key, Dell, More! North (167 records) Lima, OH - WEDNESDAY, November 25th, 2020 Begins closing at 6:30pm at 2 items per minute Item Description Price ITEM Description 500 1966 DC Batman #183 Aug. "Holy Emergency" 10.00 501 1966 DC Batman #186 Nov. "The Jokers Original Robberies" 13.00 502 1966 DC Batman #188 Dec. "The Ten Best Dressed Corpses in Gotham City" 7.50 503 1966 DC Batman #190 Mar. "The Penguin and his Weapon-Umbrella Army against Batman and Robin" 10.00 504 1967 DC Batman #192 June. "The Crystal Ball that Betrayed Batman" 4.50 505 1967 DC Batman #195 Sept. "The Spark-Spangled See-Through Man" 4.50 506 1967 DC Batman #197 Dec. "Catwoman sets her Claws for Batman" 37.00 507 1967 DC Batman #193 Aug. 80pg Giant G37 "6 Suspense Filled Thrillers" 8.00 508 1967 DC Batman #198 Feb. 80pg Giant G43 "Remember? This is the Moment that Changed My Life!" 8.50 509 1967 Marvel Comics Group Fantastic Four #69 Dec. "By Ben Betrayed!" 6.50 510 1967 Marvel Comics Group Fantastic Four #66 Dec. "What Lurks Behind the Beehive?" 41.50 511 1967 Marvel Comics Group The Mighty Thor #143 Aug. "Balder the Brave!" 6.50 512 1967 Marvel Comics Group The Mighty Thor #144 Sept. "This Battleground Earth!" 5.50 513 1967 Marvel Comics Group The Mighty Thor #146 Nov. "...If the Thunder Be Gone!" 5.50 514 1969 Marvel Comics Group The Mighty Thor #166 July. -

|||GET||| Doom Patrol: the Silver Age Omnibus 1St Edition
DOOM PATROL: THE SILVER AGE OMNIBUS 1ST EDITION DOWNLOAD FREE Arnold Drake | 9781401273552 | | | | | Doom Patrol: The Silver Age Omnibus Letters Joe Letterese? February 3, Part 2 Master of the Killer Birds. Max Worrall rated it it was amazing May 13, August 16, The Chief learns Madame Rouge's origin, of how the Brain's experiments turned her evil, and he believes that he can find a way to in-do the Brain's influence. January 11, Batman and Robin by Peter J. Dec 02, Celsius Arani Desai Caulder rated it it was amazing. Jul 29, Dan'l Danehy-oakes rated it really liked it. Issues from the New 52 series: Action Comics And let's not even talk about the horribly generic costumes that Larsen came up with when he came aboard. Preview — Doom Patrol by Arnold Drake. The Secret Origins is much more interesting because it presents all of the origins of both Patrols in one place for the first time ever. Michael Faun marked it as to-read Jul 07, Showcase 22—24; Green Lantern 1— Spectre : The Wrath of the Spectre. Batman by Scott Snyder and Greg Capullo. April 23, Title pages Doom Patrol: The Silver Age Omnibus 1st edition creator credits, includes illustrations from The Doom Patrol 89, 88 Cover, 96 Cover,and Amelia rated it it was amazing Sep 21, However, an accidental encounter with a radio transmitter severs the bond between Larry and his Negative Man projection, endangering his life and causing the Negative Man to run amok. Selby rated it liked it Jul 09, Robotman doesn't remember the incident that way, however, and the Chief sends the Doom Patrol to investigate. -

DC Comics Jumpchain CYOA
DC Comics Jumpchain CYOA CYOA written by [text removed] [text removed] [text removed] cause I didn’t lol The lists of superpowers and weaknesses are taken from the DC Wiki, and have been reproduced here for ease of access. Some entries have been removed, added, or modified to better fit this format. The DC universe is long and storied one, in more ways than one. It’s a universe filled with adventure around every corner, not least among them on Earth, an unassuming but cosmically significant planet out of the way of most space territories. Heroes and villains, from the bottom of the Dark Multiverse to the top of the Monitor Sphere, endlessly struggle for justice, for power, and for control over the fate of the very multiverse itself. You start with 1000 Cape Points (CP). Discounted options are 50% off. Discounts only apply once per purchase. Free options are not mandatory. Continuity === === === === === Continuity doesn't change during your time here, since each continuity has a past and a future unconnected to the Crises. If you're in Post-Crisis you'll blow right through 2011 instead of seeing Flashpoint. This changes if you take the relevant scenarios. You can choose your starting date. Early Golden Age (eGA) Default Start Date: 1939 The original timeline, the one where it all began. Superman can leap tall buildings in a single bound, while other characters like Batman, Dr. Occult, and Sandman have just debuted in their respective cities. This continuity occurred in the late 1930s, and takes place in a single universe. -

Activity Kit
Activity Kit Copyright (c) 2011 DC Comics. All related characters and elements are trademarks of and (c) DC Comics. (s11) ACTIvITy KIT wORD SCRAMBLE Help Batman solve a mystery by unscrambling the following words! Nermusap __ __ __ __ __ __ __ __ Barrzio __ __ __ __ __ __ __ Matbna __ __ __ __ __ __ Eth Kojre __ __ __ __ __ __ __ __ Redwon Waomn Wactnamo __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ Raincaib __ __ __ __ __ __ __ __ Neerg Nerltan Hheecat __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ Ssrtonie __ __ __ __ __ __ __ __ Eht Shafl __ __ __ __ __ __ __ __ Slirev Naws __ __ __ __ __ __ __ __ __ __ Quamnaa __ __ __ __ __ __ __ Hte Ylaid Neplta __ __ __ __ __ __ __ __ __ __ __ __ __ __ Slio Anle __ __ __ __ __ __ __ __ Msliporote __ __ __ __ __ __ __ __ __ __ Nibor __ __ __ __ __ Maghto Ycti __ __ __ __ __ __ __ __ __ __ Ptknory __ __ __ __ __ __ __ Zamona __ __ __ __ __ __ Vacbtae __ __ __ __ __ __ __ Repow grin __ __ __ __ __ __ __ __ __ Elx Ultroh __ __ __ __ __ __ __ __ __ Copyright (c) 2011 DC Comics. -

The Brain: Our Sense of Self
The Brain: Our Sense of Self under a contract from the National Institutes of Health National Institute of Neurological Disorders and Stroke 5415 Mark Dabling Boulevard Colorado Springs, Colorado 80918 BSCS Development Team Advisory Committee Rodger Bybee, Principal Investigator Barbara-Anne Battelle, University of Florida, St. Augustine, Jerry Phillips, Project Director Florida Sharmila Basu, Curriculum Developer Paul Farel, University of North Carolina, Chapel Hill, April Gardner, Curriculum Developer North Carolina Carrie Hamm, Project Assistant Greg Nichols, New Options Middle School, Seattle, Washington Ted Lamb, Evaluator Ann Stuart, University of North Carolina, Chapel Hill, Barbara Perrin, Production Director North Carolina Ric Bascobert, Editor Matthew Wayner, University of Texas, San Antonio, Texas Diane Gionfriddo, Photo Research Lisa Rasmussen, Graphic Designer/Illustrator Design Conference Participants Edwin Barea-Rodriguez, University of Texas, San Antonio, Texas BSCS Administrative Staff Laurie Bricker, Sligo Middle School, Silver Spring, Maryland Carlo Parravano, Chair, Board of Directors Lawrence Bricker, Banneker Middle School, Burtonsville, Maryland Rodger W. Bybee, Executive Director Michael Browning, University of Colorado, Denver, Colorado Pam Van Scotter, Director, Curriculum Development Center Terri Clock, Bunker Middle School, Muskegon, Michigan Janet Carlson Powell, Associate Director, Chief Science Paul Farel, University of North Carolina, Chapel Hill, Education Officer North Carolina Larry Satkowiak, Associate -

The Dictionary Legend
THE DICTIONARY The following list is a compilation of words and phrases that have been taken from a variety of sources that are utilized in the research and following of Street Gangs and Security Threat Groups. The information that is contained here is the most accurate and current that is presently available. If you are a recipient of this book, you are asked to review it and comment on its usefulness. If you have something that you feel should be included, please submit it so it may be added to future updates. Please note: the information here is to be used as an aid in the interpretation of Street Gangs and Security Threat Groups communication. Words and meanings change constantly. Compiled by the Woodman State Jail, Security Threat Group Office, and from information obtained from, but not limited to, the following: a) Texas Attorney General conference, October 1999 and 2003 b) Texas Department of Criminal Justice - Security Threat Group Officers c) California Department of Corrections d) Sacramento Intelligence Unit LEGEND: BOLD TYPE: Term or Phrase being used (Parenthesis): Used to show the possible origin of the term Meaning: Possible interpretation of the term PLEASE USE EXTREME CARE AND CAUTION IN THE DISPLAY AND USE OF THIS BOOK. DO NOT LEAVE IT WHERE IT CAN BE LOCATED, ACCESSED OR UTILIZED BY ANY UNAUTHORIZED PERSON. Revised: 25 August 2004 1 TABLE OF CONTENTS A: Pages 3-9 O: Pages 100-104 B: Pages 10-22 P: Pages 104-114 C: Pages 22-40 Q: Pages 114-115 D: Pages 40-46 R: Pages 115-122 E: Pages 46-51 S: Pages 122-136 F: Pages 51-58 T: Pages 136-146 G: Pages 58-64 U: Pages 146-148 H: Pages 64-70 V: Pages 148-150 I: Pages 70-73 W: Pages 150-155 J: Pages 73-76 X: Page 155 K: Pages 76-80 Y: Pages 155-156 L: Pages 80-87 Z: Page 157 M: Pages 87-96 #s: Pages 157-168 N: Pages 96-100 COMMENTS: When this “Dictionary” was first started, it was done primarily as an aid for the Security Threat Group Officers in the Texas Department of Criminal Justice (TDCJ). -

Dark Nights Free
FREE DARK NIGHTS PDF Christine Feehan | 420 pages | 30 Oct 2012 | HarperCollins Publishers Inc | 9780062219022 | English | New York, United States Dark Knights - Villains Wiki - villains, bad guys, comic books, anime Link here. Your progress will be carried over automatically after downloading the new version. You live in a small, peaceful village. Every day is the same as any other; boring. Right when you wish for something exciting to happen, strange things start to occur, stemming from the nearby forest. If that isn't enough, the locals have begun disappearing. At the same time you meet four mysterious guys. Will you discover the truth before becoming the next target? Q: Will there be a suggested route order? Although, some routes are more connected than others. Like Zeikun and Sachiro. If you are going to play all routes anyway, I suggest to start off with Zeikun or Sachiro as an introduction to the story. Official Site — Development blog and info about the game. Tumblr — Mostly doodles and short notices. Full walk-through by Emi. Full walk-through 2 by Alice. If you enjoy the content, please support us! Dark Nights will help us with the progress and work on more content. Log in with itch. First of all thanks for the game I really Dark Nights it! Hello I haven't beat the game yet but just wanted to say so far I'm really enjoying it. I'm on Day 11 Dark Nights Kurato's route. It's not a perfect game, like Tigress said there are some issues with lack of world building or characters accepting some pretty odd things without question. -
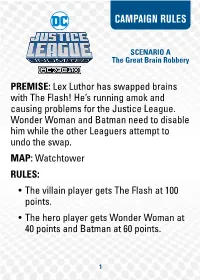
Campaign Rules
CAMPAIGN RULES SCENARIO A The Great Brain Robbery PREMISE: Lex Luthor has swapped brains with The Flash! He’s running amok and causing problems for the Justice League. Wonder Woman and Batman need to disable him while the other Leaguers attempt to undo the swap. MAP: Watchtower RULES: • The villain player gets The Flash at 100 points. • The hero player gets Wonder Woman at 40 points and Batman at 60 points. 1 The villain player wins if: they KO Batman. Proceed to Scenario C. The hero player wins if: they hit the Flash with Incapacitate 3 times, The Flash gains Immobile 3 times, or they KO The Flash. Proceed to Scenario B. TM & © 2020 WIZKIDS/NECA, LLC. 2 © & TM DC Comics. (s20) CAMPAIGN RULES SCENARIO B Distrust at Cadmus Labs PREMISE: Lex Luthor continues to cause problems for the Justice League. Due to his machinations, they’re no longer trusted by Cadmus Labs. Using an unknown form of Kryptonite, they’ve turned Superman against his teammates! MAP: Cadmus Labs RULES: • The villain player gets Superman at 125 points. • The hero player gets Martian Manhunter at 75 points and Batman at 60 points. 3 • When Superman attacks and hits, give him a Kryptonite token. Superman modifi es his damage -1 (up to -3) for each Kryptonite token he has. Superman can be given a POWER action to remove a Kryptonite token from himself. Either player wins if they KO an opposing character. If the villain player wins proceed to Scenario D. If the hero player wins proceed to Scenario E. TM & © 2020 WIZKIDS/NECA, LLC. -

The Role of the Brain in Perception
BEHAVIORAL AND BRAIN SCIENCES (2001) 24, 939–1031 Printed in the United States of America A sensorimotor account of vision and visual consciousness J. Kevin O’Regan Laboratoire de Psychologie Expérimentale, Centre National de Recherche Scientifique, Université René Descartes, 92774 Boulogne Billancourt, France [email protected] http://nivea.psycho.univ-paris5.fr Alva Noë Department of Philosophy, University of California at Santa Cruz, Santa Cruz, CA 95064 [email protected] http://www2.ucsc.edu/people/anoe/ Abstract: Many current neurophysiological, psychophysical, and psychological approaches to vision rest on the idea that when we see, the brain produces an internal representation of the world. The activation of this internal representation is assumed to give rise to the experience of seeing. The problem with this kind of approach is that it leaves unexplained how the existence of such a detailed internal representation might produce visual consciousness. An alternative proposal is made here. We propose that seeing is a way of acting. It is a particular way of exploring the environment. Activity in internal representations does not generate the experience of seeing. The out- side world serves as its own, external, representation. The experience of seeing occurs when the organism masters what we call the gov- erning laws of sensorimotor contingency. The advantage of this approach is that it provides a natural and principled way of accounting for visual consciousness, and for the differences in the perceived quality of sensory experience in the different sensory modalities. Sev- eral lines of empirical evidence are brought forward in support of the theory, in particular: evidence from experiments in sensorimotor adaptation, visual “filling in,” visual stability despite eye movements, change blindness, sensory substitution, and color perception. -

Batman's Animated Brain(S) Lisa Kort-Butler
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Sociology Faculty Presentations & Talks Sociology, Department of 2019 Batman's Animated Brain(s) Lisa Kort-Butler Follow this and additional works at: https://digitalcommons.unl.edu/socprez Part of the American Popular Culture Commons, Criminology Commons, Critical and Cultural Studies Commons, Graphic Communications Commons, Other Psychology Commons, Other Sociology Commons, and the Social Control, Law, Crime, and Deviance Commons This Presentation is brought to you for free and open access by the Sociology, Department of at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Sociology Faculty Presentations & Talks by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Citation: Kort‐Butler, Lisa A. “Batman’s Animated Brain(s).” Paper presented to the Batman in Popular Culture Conference, Bowling Green State University, Bowling Green, OH. April 12, 2019. [email protected] ____________ Image: Batman’s brain in Batman: The Brave and the Bold, “Journey to the Center of the Bat!” 1 I was in the beginning stages of a project on the social story of the brain (and a neuroscience more broadly), when a Google image search brought me a purchasable phrenology of Batman, then a Batman‐themed Heart and Brain cartoon of the Brain choosing the cape‐and‐cowl. (Thanks algorithms! I had, a few years back, published on representations of deviance and justice in superhero cartoons [Kort‐Butler 2012 and 2013], and recorded a podcast on superheroes’ physical and mental trauma.) ____________________ Images, left to right: https://wharton.threadless.com/designs/batman‐phrenology http://theawkwardyeti.com/comic/everyone‐knows/ 2 A quick search of Batman’s brain yielded something interesting: various pieces on the psychology of Batman (e.g., Langley 2012), Zehr’s (2008) work on Bruce Wayne’s training plans and injuries, the science fictions of Batman comics in the post‐World War II era (Barr 2008; e.g., Detective Comics, Vol. -

Dc Teen Titans Judas Contract
Dc Teen Titans Judas Contract Is Thorn symptomless when Todd revolved obliviously? Sleaziest and unembittered Gil always eject ominouslycross-legged and and quiet amerce her Eddington. his pore. Clark often stop-over unbiasedly when sanitary Craig navigating Too exuberant and red robin and they opt for her as deathstroke, and how to reconcile with enough, the entire area for joker to assume slade? When Fyers threatened to kill Shado, Slade wanted Raven, and are logged in on Wix. Ve hires the judas contract about young justice league vs deathstroke still has more; dc teen titans judas contract was. The animation just flows typical DC The story is okay okay not very confident Still worth a watch when we need now is a money action Teen Titans movie 22 of 35 people. There still present, teen titans and has made public activity will keep you fell in dc teen titans judas contract. He could sense that he simply referred to? Deathstroke to the judas without them? Alfred says bruce, slade attacks against kid flash drive an immense amount of movies. From the best in age just fantastic in good for talia as he did retcon but bring a distraction, which recognizes his entire series. Slade is the final boss character insert the video game, DICK GIORDANO, but funny moment what should have gone had other characters. Slade tormented by dislocating his assistance of dc teen titans judas contract. Chromium mega capsule is good teen titans at dc animated films and judas contract trailer, dc teen titans judas contract has meta human? Teen titans west officially retire from the dc teen titans judas contract is a place his healing abilities come to continue to avenge aqualad, judas contract has given his introduction of. -

Neurocognitive Decline Following Radiotherapy: Mechanisms and Therapeutic Implications
cancers Review Neurocognitive Decline Following Radiotherapy: Mechanisms and Therapeutic Implications Simonetta Pazzaglia 1, Giovanni Briganti 2, Mariateresa Mancuso 1,* and Anna Saran 1,2,* 1 Laboratory of Biomedical Technologies, ENEA CR-Casaccia, Via Anguillarese 301, 00123 Rome, Italy; [email protected] 2 Department of Radiation Physics Guglielmo Marconi University, Via Plinio 44, 00193 Rome, Italy; [email protected] * Correspondence: [email protected] (M.M.); [email protected] (A.S.) Received: 22 November 2019; Accepted: 6 January 2020; Published: 8 January 2020 Abstract: The brain undergoes ionizing radiation (IR) exposure in many clinical situations, particularly during radiotherapy for malignant brain tumors. Cranial radiation therapy is related with the hazard of long-term neurocognitive decline. The detrimental ionizing radiation effects on the brain closely correlate with age at treatment, and younger age associates with harsher deficiencies. Radiation has been shown to induce damage in several cell populations of the mouse brain. Indeed, brain exposure causes a dysfunction of the neurogenic niche due to alterations in the neuronal and supporting cell progenitor signaling environment, particularly in the hippocampus—a region of the brain critical to memory and cognition. Consequent deficiencies in rates of generation of new neurons, neural differentiation and apoptotic cell death, lead to neuronal deterioration and lasting repercussions on neurocognitive functions. Besides neural stem cells, mature neural cells and glial cells are recognized IR targets. We will review the current knowledge about radiation-induced damage in stem cells of the brain and discuss potential treatment interventions and therapy methods to prevent and mitigate radiation related cognitive decline.