The Illawarra Shoalhaven Health Care System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

S125 Bus Time Schedule & Line Route
S125 bus time schedule & line map S125 Shellharbour Rd opp Barrack Av to Tongara View In Website Mode College The S125 bus line (Shellharbour Rd opp Barrack Av to Tongara College) has 2 routes. For regular weekdays, their operation hours are: (1) Calderwood Cc: 8:10 AM (2) Shellharbour PS: 3:30 PM Use the Moovit App to ƒnd the closest S125 bus station near you and ƒnd out when is the next S125 bus arriving. Direction: Calderwood Cc S125 bus Time Schedule 51 stops Calderwood Cc Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday Not Operational Shellharbour Rd opp Barrack Av 324 Shellharbour Road, Barrack Heights Tuesday 8:10 AM Shellharbour Rd after Roberts Av Wednesday 8:10 AM 288 Shellharbour Road, Barrack Point Thursday Not Operational Shellharbour Rd opp Jason Av Friday Not Operational 264 Shellharbour Road, Barrack Point Saturday Not Operational Shellharbour Rd at Sunset Av 238 Shellharbour Road, Barrack Point Shellharbour Rd at William Av 210 Shellharbour Road, Warilla S125 bus Info Direction: Calderwood Cc Shellharbour Rd opp Terry Av Stops: 51 186 Shellharbour Road, Warilla Trip Duration: 38 min Line Summary: Shellharbour Rd opp Barrack Av, Shellharbour Rd after Lake Entrance Rd Shellharbour Rd after Roberts Av, Shellharbour Rd Shellharbour Road, Warilla opp Jason Av, Shellharbour Rd at Sunset Av, Shellharbour Rd at William Av, Shellharbour Rd opp Shellharbour Rd after Barnes St Terry Av, Shellharbour Rd after Lake Entrance Rd, 128 Shellharbour Road, Warilla Shellharbour Rd after Barnes St, Shellharbour Rd opp Warilla -
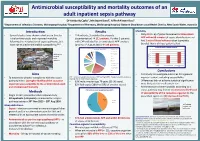
Introduction Aims Methods Results Conclusions
Antimicrobial susceptibility and mortality outcomes of an adult inpatient sepsis pathway Dr Kimberly Cipko1, Mr Stuart Bond2, A/Prof Alistair Reid1 1Department of Infectious Diseases, Wollongong Hospital; 2Department of Pharmacy, Wollongong Hospital, Illawarra Shoalhaven Local Health District, New South Wales, Australia Introduction Results Mortality • Several studies have shown reductions in time to • 114 patients, 3 excluded (inadequate • Only 6% (n=6) of patients received antimicrobials initial antimicrobials and improved mortality documentation) 111 patients. Further 5 patients APP within 60 minutes of sepsis identification and following the introduction of sepsis pathways, but with CAP excluded for ‘antimicrobials APP’ analysis had 2 sets of blood cultures taken (complete have not studied antimicrobial susceptibility.1,2,3 (prior to 1st August 2016) 106 patients. bundle). None of those patients died. 30-day all-cause in hospital mortality Source of sepsis (%) Unkown origin 35 HAP low MRO 30 4 111 25 Wollongong 6 HAP high MRO 20 Hospital 5 CAP 33 15 NSW, Urine % mortality % mortality 10 Australia 9 Biliary/GI 5 Skin/surgical site 0 5 Diabetic foot Overall Antimicrobials APP Antimicrobials not APP Peri/postpartum 13 Other 23 Conclusions Neuro Aims • First study to investigate outcomes for a general CAP – community acquired pneumonia; HAP low/high MRO – Hospital acquired pneumonia inpatient cohort, including susceptibility. • To determine whether compliance with the sepsis low/high risk of multi-resistant organisms pathway led to: (1) Higher likelihood the causative • 63% male; median age 76 years (21-96 years). • Differences did not achieve statistical significance – organism was susceptible to the antimicrobials used • 82% had sepsis (18% had SIRS of another cause). -

Masterplan LAND ESTATE W
EDUCATION 1 The Little School Pre School 2 min 1km 2 Dapto Public School 8 min 7km 3 Mount Kembla Public School 15 min 12.6km 4 Kanahooka High School 7 min 5.8km 5 Illawarra Sports High School 10 min 9.2km 6 Dapto High School 9 min 6.3km 7 Five Islands Secondary College 18 min 4.6km 8 University of Wollongong 13 min 15.1km 9 TAFE Illawarra Wollongong Campus 14 min 15.7km RETAIL 1 Wollongong Central 15 min 14.9km 2 Figtree Grove Shopping Centre 11 min 10.1km 3 Dapto Mall 5 min 4.9km 4 Shellharbour Village 22 min 21.3km 5 Shellharbour Square Shopping Centre 22 min 18.5km 6 Shell Cove 20 min 20km (with Marina under construction) HEALTH 1 Wollongong Hospital 13 min 14km 2 Wollongong Private Hospital 13 min 13.7km 3 Dapto Medical Centre 5 min 4.9km 4 Illawarra HealthCare Centre 4 min 3.8km 5 Illawarra Medical Services 9 min 8.4km 6 Illawarra Area Health Service 15 min 15.4km 7 Lotus Wellbeing Centre 18 min 16.6km RECREATION 1 Kembla Grange Racecourse 5 min 4.5km 2 Fox Karting Centre 5 min 4.9km 3 The Grange Golf Club 6 min 5.3km 4 Ian McLennan Park 5 min 4.8km 5 Berkeley Youth & Recreation Centre 9 min 7.8km 6 Wollongong Surf Leisure Resort 16 min 19.5km 7 Windang Bowling Club 19 min 18.1km 8 Lake Illawarra Yacht Club 11 min 10.5km 9 Port Kembla Beach 16 min 16km 10 WIN Stadium 16 min 16km 11 WIN Entertainment Centre 17 min 16.9km 12 Jamberoo Action Park 22 min 20.7km 13 Wollongong Golf Club 18 min 17km 14 Killalea State Park 23 min 21.7km TRANSPORT 1 Kembla Grange Train Station 4 min 4.2km 2 Dapto Train Station 6 min 5.1km 3 Unanderra Train Station 9 min 8km 4 Coniston Train Station 14 min 15.1km 5 Wollongong Train Station 16 min 16.5km Stockland Shellharbour Shopping Centre University of Wollongong Nan Tien Temple City of Wollongong Proudly marketed by: Simon Hagarty - Sales Manager REGISTER HERE: C 0405 175 416 BRAND NEW E [email protected] Masterplan LAND ESTATE www.KemblaGrangeEstate.com.au W www.ulh.com.au Disclaimer: This is a sales plan only. -

Illawarra & Shoalhaven Sexual Health & Blood Borne Infections Directory
Illawarra & Shoalhaven Sexual Health & Blood Borne Infections Directory Intention of the directory: What is sexual health? According to the World Health Organisation sexual health is not merely the absence of disease, dysfunction or infirmity, but rather, sexual health includes a holistic state of physical, emotional, mental and social well-being. As such, sexual health requires a respectful approach to sexuality and relationships, free of coercion, discrimination and violence. Who is HARP? The HARP Health promotion team promote prevention, early intervention, treatment and management of HIV/AIDS, Hepatitis C and Sexually Transmitted Infections. The HIV and Related Programmes Unit (HARP) activity is guided by National, State and Local Health District strategies that aims to improve sexual health and reduce the harm associated with Sexually Transmissible Infections (STIs), HIV and Hepatitis C. The HARP team partner with community organisations who engage and represent people from culturally and linguistically diverse backgrounds (CALD), young people, Aboriginal people, sex workers, gay men, men who have sex with men (MSM), people living with HIV, people who inject drugs, and heterosexuals with a recent change in partner. HARP provide a range of free resources, work in collaboration with partner organisations on projects and develop awareness raising and capacity building training sessions. What is the intention of HARP? Our intention is to create a positive environment in which the community feel comfortable to approach the issues of HIV, STIs and Blood Borne Infections (BBIs) and acknowledge the realities of their impact both within our own communities and globally. We work towards creating an environment where HIV, STIs and BBIs can be discussed, accepted and ultimately prevented without fear, myth, stigma or discrimination. -
Guide to Cycling in the Illawarra
The Illawarra Bicycle Users Group’s Guide to cycling in the Illawarra Compiled by Werner Steyer First edition September 2006 4th revision August 2011 Copyright Notice: © W. Steyer 2010 You are welcome to reproduce the material that appears in the Tour De Illawarra cycling guide for personal, in-house or non-commercial use without formal permission or charge. All other rights are reserved. If you wish to reproduce, alter, store or transmit material appearing in the Tour De Illawarra cycling guide for any other purpose, request for formal permission should be directed to W. Steyer 68 Lake Entrance Road Oak Flats NSW 2529 Introduction This cycling ride guide and associated maps have been produced by the Illawarra Bicycle Users Group incorporated (iBUG) to promote cycling in the Illawarra. The ride guides and associated maps are intended to assist cyclists in planning self- guided outings in the Illawarra area. All persons using this guide accept sole responsibility for any losses or injuries uncured as a result of misinterpretations or errors within this guide Cyclist and users of this Guide are responsible for their own actions and no warranty or liability is implied. Should you require any further information, find any errors or have suggestions for additional rides please contact us at www.ibug,org.com Updated ride information is available form the iBUG website at www.ibug.org.au As the conditions may change due to road and cycleway alteration by Councils and the RTA and weather conditions cyclists must be prepared to change their plans and riding style to suit the conditions encountered. -
Feasibility of a Multi-Generational Birth Cohort Study Michelle L
Townsend et al. Pilot and Feasibility Studies (2019) 5:32 https://doi.org/10.1186/s40814-019-0418-5 STUDY PROTOCOL Open Access Illawarra Born cross-generational health study: feasibility of a multi-generational birth cohort study Michelle L. Townsend1,2, Megan A. Kelly1,7, Judy A. Pickard1,2, Theresa A. Larkin1,3, Victoria M. Flood5,6, Peter Caputi1,2, Ian M. Wright1,3,4, Alison Jones1,3 and Brin F. S. Grenyer1,2* Abstract Background: There is a strong interest in the concept of developmental origins of health and disease and their influence on various factors “from cradle to grave”. Despite the increasing appreciation of this lifelong legacy across the human life course, many gaps remain in the scientific understanding of mechanisms influencing these formative phases. Cross-generational susceptibility to health problems is emerging as a focus of research in the context of birth cohort studies. The primary aim of the Illawarra Born study is to make scientific discoveries associated with improving health and wellbeing across the lifespan, with a particular focus on preventable chronic diseases, especially mental health. This birth cohort study will follow and collect data from three cohorts representing different stages across the lifespan: infants, adults (parents) and older adults (grandparents). The multi-generational, cross-sectional and longitudinal design of this birth cohort study supports a focus on the contributions of genetics, environment and lifestyle on health and wellbeing. The feasibility of conducting a multi-generational longitudinal birth cohort project was conducted through a small pilot study. Methods/design: The purpose of this paper is to report on the feasibility and acceptability of the research protocol for a collaborative cross-generation health study in the community and test recruitment and outcome measures for the main study. -

Wollongong Hospital Nurses' Home
Wollongong Hospital Nurses’ Home Heritage Significance Assessment Final Report Report prepared for NSW Health Infrastructure September 2011 Report Register The following report register documents the development and issue of the report entitled Wollongong Hospital Nurses’ Home—Heritage Significance Assessment, undertaken by Godden Mackay Logan Pty Ltd in accordance with its quality management system. Godden Mackay Logan operates under a quality management system which has been certified as complying with the Australian/New Zealand Standard for quality management systems AS/NZS ISO 9001:2008. Job No. Issue No. Notes/Description Issue Date 10-0466 1 Draft Report June 2011 10-0466 2 Final Report September 2011 Copyright Historical sources and reference material used in the preparation of this report are acknowledged and referenced at the end of each section and/or in figure captions. Reasonable effort has been made to identify, contact, acknowledge and obtain permission to use material from the relevant copyright owners. Unless otherwise specified or agreed, copyright in this report vests in Godden Mackay Logan Pty Ltd (‘GML’) and in the owners of any pre-existing historic source or reference material. Moral Rights GML asserts its Moral Rights in this work, unless otherwise acknowledged, in accordance with the (Commonwealth) Copyright (Moral Rights) Amendment Act 2000. GML’s moral rights include the attribution of authorship, the right not to have the work falsely attributed and the right to integrity of authorship. Right to Use GML grants to the client for this project (and the client’s successors in title) an irrevocable royalty-free right to reproduce or use the material from this report, except where such use infringes the copyright and/or Moral Rights of GML or third parties. -

Free Gong Shuttle Saved! Thanks to You Wollongong, Together We Have Saved the Gong Shuttle
JULY 2018 JULY PAUL SCULLY’S WOLLONGONG WRAP UP Office & Mail: Suite 2S, Rear Ground Floor, 111 Crown Street, Wollongong, NSW 2500 Phone: (02) 4226 5700 Fax: (02) 4226 9963 Web: paulscullymp.com.au paulscullymp Email: [email protected] PaulScullyWollongong Free Gong Shuttle saved! Thanks to you Wollongong, together we have saved the Gong Shuttle. We signed petitions and held a public rally in the Wollongong Mall, to tell the Berejiklian Government just what we all thought of its plan to introduce Opal fares on the free Gong Shuttle service. After months of hard work and negotiations, an agreement has finally been reached where the Gong Shuttle will remain free and continue to operate 7 days a week on its existing routes, which includes stops at the University of Wollongong, Innovation Campus, Wollongong CBD and Wollongong Hospital. There will be minor changes to the timetable on Sundays and public holidays. On these days, Gong Shuttle services will run between 9.40am and 5.20pm, instead of starting at 8am and finishing at 6pm. Buses will continue to run every 20 minutes. The agreement between Transport for NSW, the University of Wollongong and Wollongong City Council makes sure that the Gong Shuttle service remains free. Does the NSW Government have some of your money? There’s more than $380 million of your money, waiting to be claimed from deceased estates, dividends, bonds and overpayments, according to Revenue NSW. So what are you waiting for? Go to www.revenue.nsw.gov.au/ucm/search to see if any of the unclaimed money is yours. -
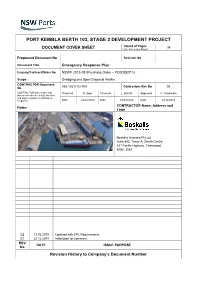
Port Kembla Berth 103, Stage 2 Development Project
PORT KEMBLA BERTH 103, STAGE 2 DEVELOPMENT PROJECT Total # of Pages 34 DOCUMENT COVER SHEET (incl. Doc Cover Sheet) Proponent Document No Revision No Document Title Emergency Response Plan Enquiry/Contract/Order No NSWP 2013-05 (Purchase Order – PO000527-1) Scope Dredging and Spoil Disposal Works CONTRACTOR Document 036-10211-02-004 Contractors Rev No 02 No CONTRACTOR shall ensure that Prepared D. Inger Checked L. Barratt Approved C. Tombolato documents have been fully checked and approved prior to submittal to Proponent. Date 22/12/2014 Date 23/12/2014 Date 23/12/2014 CONTRACTOR Name, Address and Notes: Logo Boskalis Australia Pty Ltd Suite 802, Tower A, Zenith Centre 821 Pacific Highway, Chatswood NSW, 2067 02 13.06.2015 Updated with EPL Requirements 01 22.12.2014 Initial plan for comment REV DATE ISSUE PURPOSE No Revision History to Company’s Document Number Berth 103 Stage 2 Extension - Dredging and Spoil Disposal Works Emergency Response Plan TABLE OF CONTENTS 1. DEFINITIONS & ABBREVIATIONS 4 1.1 Definitions 4 1.2 Abbreviations 5 2. PROJECT INTRODUCTION 6 2.1 General 6 2.2 Project Overview 6 2.3 Purpose and Applicability 8 3. REFERENCES 9 3.1 Controlled Legislation 9 3.2 Codes of Practice and Standards 9 3.3 PROPONENT Documents 9 3.4 CONTRACTOR Documents 10 3.5 PROJECT Documents 11 4. EMERGENCY RESPONSE - OBJECTIVES AND TARGETS 12 4.1 Management Objectives 12 4.2 Targets 12 5. EMERGENCY RESPONSE ORGANISATION AND RESPONSIBILITIES 13 5.1 Crisis Manager (CM) 13 5.2 Incident Controller (IC) 13 5.3 Emergency Response Team (ERT) 14 5.3.1 Emergency Drills 14 6. -

Checklist for SSA Submissions to The
Checklist for Site Specific Assessment submissions to the Research Governance Officer Site Specific Assessments (SSA) can be submitted before or after receiving Ethics approval, however both submissions are encouraged to be done in parallel. Please include 1 copy of each of the documents submitted for Research Ethics Approval and 1 original of the following documents: Cover Letter: Outline if study has been or is being considered by the Human Research Ethics Committee (HREC) Identify if HREC approval has been granted (include date) or is pending If available, include the HREC reference number List all documents enclosed Site Specific Assessment Form (SSA) – www.ethicsform.org/au Signed and dated by ALL investigators named in the SSA Signed by the relevant ISLHD Head(s) of Department(s) – Principal Investigators who are Heads of Department must not sign their own SSA applications but must obtain the signature of their direct manager. Signed by relevant ISLHD Head(s) of Supporting Department(s) (eg. Pharmacy if dispensing drugs) (if applicable) Signed by Data Provision (if applicable) Documents to be included with the SSA submission: Short CV for all Investigators (Principal and Associate) named in the SSA form Site Specific Participant Information Sheet and Consent Form (must include the ISLHD logo and each page must have the date and version number in the footer) Letter of approval from the HREC HREC Amendment Approval Letters (if applicable) National Ethics Application Form (NEAF) or Low/Negligible Risk Ethics Application -

Design and Implementation of a Novel Web-Based E-Learning Tool for Education of Health Professionals on the Antibiotic Vancomycin
JOURNAL OF MEDICAL INTERNET RESEARCH Bond et al Original Paper Design and Implementation of a Novel Web-Based E-Learning Tool for Education of Health Professionals on the Antibiotic Vancomycin Stuart Evan Bond1,2,3, B Pharm, Dip Pharm Prac; Shelley P Crowther1, B Pharm, M Public Health; Suman Adhikari4,5, B Pharm; Adriana J Chubaty6, BSc (Pharm); Ping Yu7, PhD; Jay P Borchard8, BSc (Hons); Craig Steven Boutlis9, MBBS, PhD; Wilfred Winston Yeo2,3,10, MD; Spiros Miyakis2,3,9, MD, PhD 1Wollongong Hospital, Department of Pharmacy, Illawarra Shoalhaven Local Health District, Wollongong, Australia 2School of Medicine, Faculty of Science, Medicine and Health, University of Wollongong, Wollongong, Australia 3Illawarra Health and Medical Research Institute, University of Wollongong, Wollongong, Australia 4St George Hospital, Department of Pharmacy, South Eastern Sydney Local Health District, Kogarah, Australia 5St George Clinical School, Faculty of Medicine, University of New South Wales, Kogarah, Australia 6Prince of Wales Hospital, Department of Pharmacy, South Eastern Sydney Local Health District, Randwick, Australia 7School of Computing and Information Technology, Faculty of Engineering and Information Sciences, University of Wollongong, Wollongong, Australia 8Research Central, Wollongong Hospital, Illawarra Shoalhaven Local Health District, Wollongong, Australia 9Wollongong Hospital, Department of Infectious Diseases, Illawarra Shoalhaven Local Health District, Wollongong, Australia 10Wollongong Hospital, Division of Medicine, Illawarra Shoalhaven Local Health District, Wollongong, Australia Corresponding Author: Stuart Evan Bond, B Pharm, Dip Pharm Prac Wollongong Hospital Department of Pharmacy Illawarra Shoalhaven Local Health District Loftus St Wollongong, 2500 Australia Phone: 61 4255 1530 Fax: 61 4222 5430 Email: [email protected] Abstract Background: Traditional approaches to health professional education are being challenged by increased clinical demands and decreased available time. -

Illawarra Shoalhaven LHD
Illawarra Shoalhaven LHD The Illawarra Shoalhaven Local Health District was formed in 2011. The district has 250 kilometres of coastline and a population of around 369,000. The culturally diverse population is 25% rural with the rest living in cities and towns. The Local Health District is embarking on a significant capital works program, improving surgical services in the region’s tertiary referral hospital, strengthening the provision of cancer services, providing a teaching and training facility and a Sub Acute Adult Mental Health Unit. Nowra Shellharbour Nowra has a bustling commercial centre and is situated on Shellharbour is just over an hours drive from Sydney, with the beautiful Shoalhaven River, which offers fishing, river a regional airport offering connections across Australia. cruises and water sports. There are local cinemas, theatres, The city is situated between the ocean and the forest- art galleries and many community festivals and events. covered Illawarra Escarpment with Lake Illawarra and Nowra has public and private primary schools, three public the Minnamurra River in close proximity. The town offers high schools, several non-goverment schools and a campus museums and galleries, shopping and theatre as well of the University of Wollongong. Combined with it’s twin as many outdoor activities on the lake and five golden city, Bomaderry, the population is around 34,000. beaches; surfing, kayaking, diving and fishing. Shoalhaven Hospital Shellharbour Hospital Number of beds: 100-200 Number of beds: 164 Hospital type: Acute Care Facility Hospital type: District Hospital Same day admissions approx.: 12,600 Same day admissions approx.: 10,900 Overnight admissions approx.: 10,700 Overnight admissions approx.: 7,400 The Shoalhaven District Memorial Hospital is a busy acute Shellharbour Hospital has a busy acute care facility which care facility providing emergency care, medical, surgical and provides emergency services averaging around 24,000 orthopaedic services to around 22,000 patients per year.