Oregon's Medicaid
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
(12) Patent Application Publication (10) Pub. No.: US 2005/0070488A1 Coelingh Bennik Et Al
US 2005.0070488A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2005/0070488A1 Coelingh Bennik et al. (43) Pub. Date: Mar. 31, 2005 (54) ESTROGENIC COMPOUNDS IN prises the oral administration of an estrogenic component COMBINATION WITH PROGESTOGENIC and a progestogenic component to a mammal in an effective COMPOUNDS IN amount to prevent or treat Symptoms of hypoestrogenism, HORMONE-REPLACEMENT THERAPY wherein the estrogenic component is Selected from the group (76) Inventors: Herman Jan Tijmen Coelingh Bennik, consisting of Substances represented by the above formula in Driebergen (NL); Evert Johannes which formula R, R2, R, R independently are a hydrogen Bunschoten, Heesch (NL); Christian atom, a hydroxyl group or an alkoxy group with 1-5 carbon Franz Holinka, New York, NY (US) atoms; each of Rs, R, R-7 is a hydroxyl group; and no more than 3 of R, R2, R, R are hydrogen atoms; precursors Correspondence Address: capable of liberating a Substance according to the aforemen William Logsdon tioned formula when used in the present method; and Webb Ziesenheim Logsdon Orkin & Hanson mixtures of one or more of the aforementioned Substances 700 Koppers Building and/or precursors. Another aspect of the invention concerns 436 Seventh Avenue a pharmaceutical kit comprising oral dosage units that Pittsburgh, PA 15219-1818 (US) contain the aforementioned estrogenic component and a (21) Appl. No.: 10/495,707 progestogenic component as well as an androgenic compo nent. (22) PCT Filed: May 23, 2002 (86) PCT No.: PCT/NL02/00332 (30) Foreign Application Priority Data Nov. 15, 2001 (EP)........................................ O1204377.4 Feb. -

Oregon Health Plan Changes Effective January 1, 2017
HEALTH SYSTEMS DIVISION Kate Brown, Governor 500 Summer St NE E44 Salem, OR, 97301 Date: December 8, 2016 Voice: 1-800-336-6016 FAX: 503-945-6873 To: Oregon Health Plan providers TTY: 711 www.oregon.gov/OHA/healthplan From: Don Ross, Physical and Oral Health Programs manager Integrated Health Programs, Health Systems Division Subject: Oregon Health Plan changes effective January 1, 2017 To meet federal health plan requirements, the Oregon Health Authority (OHA) is making the following changes to Oregon Health Plan (OHP) benefits and copayment requirements, subject to approval by the federal Centers for Medicare & Medicaid Services. The changes apply to services covered by OHA and all coordinated care organizations on and after January 1, 2017. OHP Plus benefit changes OHA will update the Prioritized List of Health Services and related administrative rules to add these benefits effective January 1, 2017: A wig benefit of at least $150 per year for patients with hair loss related to chemotherapy or radiation therapy. Separate limits for habilitative and rehabilitative services under Guideline Note 6, which covers physical, occupational and speech therapy for adults with physical health conditions. Guideline Note 106 on Preventive Services has been modified to reflect that OHP coverage will continue to follow federal requirements for coverage of preventive services including: Services with A and B recommendations from the United States Preventive Services Task Force, Immunizations recommended by the Advisory Committee on Immunization Practices, The Health Resources & Services Administration’s Women’s Preventive Services guidelines, and The American Academy of Pediatrics Bright Futures Guidelines. Removal of OHP copayments Copays will be removed from all OHP services, including pharmacy, professional, and outpatient hospital services. -

Journal Pre-Proof
Journal Pre-proof Steroid hormones in the aquatic environment J.O. Ojoghoro, M.D. Scrimshaw, J.P. Sumpter PII: S0048-9697(21)03377-5 DOI: https://doi.org/10.1016/j.scitotenv.2021.148306 Reference: STOTEN 148306 To appear in: Science of the Total Environment Received date: 19 April 2021 Revised date: 3 June 2021 Accepted date: 3 June 2021 Please cite this article as: J.O. Ojoghoro, M.D. Scrimshaw and J.P. Sumpter, Steroid hormones in the aquatic environment, Science of the Total Environment (2018), https://doi.org/10.1016/j.scitotenv.2021.148306 This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. © 2018 © 2021 Published by Elsevier B.V. Journal Pre-proof Steroid Hormones in the Aquatic Environment Ojoghoro, J.O.a, Scrimshaw, M.D.b* and Sumpter, J.P.b a Department of Botany, Faculty of Science, Delta State University Abraka, Delta State, Nigeria b Division of Environmental Science, Department of Life Sciences, Brunel University London, Uxbridge, Middlesex, UB8 3PH, United Kingdom Abstract Steroid hormones are extremely important natural hormones in all vertebrates. -

Fee-For-Service Preferred Drug List
Prescription Drug Program Apple Health Medicaid: Fee-for-Service Preferred Drug List What is new in this version of the preferred drug list? Effective for dates of service on and after October 1, 2018, the Health Care Authority will make the following changes: Change Due to the implementation of the Apple Health Preferred Drug List (PDL), a PDL that applies to fee-for-service (FFS) clients as well as Apple Health managed care enrollees, the following changes have occurred: On the Fee-For-Service only Preferred Drug List • Drug classes that are currently on the Apple Health PDL have been removed. These classes and the drug statuses can be found on the Apple Health Preferred Drug List. On the Apple Health Preferred Drug List • New drug classes have been added. This means drugs not previously on the PDL have been added with preferred and nonpreferred statuses. Some drugs may also have additional prior authorization (PA) requirements. • For existing drug classes, preferred statuses may have changed. Some drugs may have additional PA requirements that did not previously require PA. October 25, 2018 Correction • Two drug classes were erroneously removed and have been added back to the list: Asthma – Leukotriene Modifiers Skeletal Muscle Relaxants (Rev. 10/24/2018) (Eff. 10/1/2018) – 1 – Apple Health Medicaid PDL Prescription Drug Program What is the preferred drug list? The Health Care Authority (the agency) has developed a list of preferred drugs within a chosen therapeutic class that are selected based on clinical evidence of safety, efficacy, and effectiveness. The drugs within a chosen therapeutic class are evaluated by the Drug Use Review Board, which makes recommendations to the agency regarding the selection of the preferred drugs. -
Prioritization of Health Services
PRIORITIZATION OF HEALTH SERVICES A Report to the Governor and the 72nd Oregon Legislative Assembly Oregon Health Services Commission Office for Oregon Health Policy and Research Department of Administrative Services 2003 TABLE OF CONTENTS List of Tables . iii Health Services Commission and Staff . .v Acknowledgments . .vii Executive Summary . xi CHAPTER ONE: HISTORY OF THE OREGON HEALTH PLAN Legislative Framework . 3 Implementation of the Medicaid Demonstration . .. 5 Accomplishments . 7 CHAPTER TWO: PRIORITIZATION OF HEALTH SERVICES Charge to the Health Services Commission . .. 21 Prioritization Methodology . 22 Biennial Review . 23 Interim Modifications . 31 Technical Changes . 32 Advancements in Medical Technology . .33 Solid Organ Transplantation . 34 Intrathecal Baclofen Therapy . 36 CHAPTER THREE: CLARIFICATIONS TO THE PRIORITIZED LIST OF HEALTH SERVICES Practice Guidelines . 39 Hysterectomy for Benign Conditions . 40 Adenomyosis . 42 Comfort Care . 44 Spinal Deformities . 45 Cancer of the Esophagus, Liver, Pancreas, and Gallbladder . 45 Intrathecal Baclofen Therapy . 46 Prevention Guidelines . 47 Coding Specifications . 48 Seminoma . 48 Breast Reconstruction Post-Mastectomy for Breast Cancer . 49 Statements of Intent . 49 Medical Codes Not Appearing on the Prioritized List . 50 CHAPTER FOUR: SUBCOMMITTEES, TASK FORCES, AND WORKGROUPS Health Outcomes Subcommittee . 55 Mental Health Care and Chemical Dependency Subcommittee . 56 Workgroup on Public Outreach . 57 Oncology Task Force . 58 CHAPTER FIVE: RECOMMENDATIONS . .61 i TABLE -
Progesterone 7K77 49-3265/R3 B7K770 Read Highlighted Changes Revised April, 2010 Progesterone
en system Progesterone 7K77 49-3265/R3 B7K770 Read Highlighted Changes Revised April, 2010 Progesterone Customer Service: Contact your local representative or find country specific contact information on www.abbottdiagnostics.com Package insert instructions must be carefully followed. Reliability of assay results cannot be guaranteed if there are any deviations from the instructions in this package insert. Key to symbols used List Number Calibrator (1,2) In Vitro Diagnostic Medical Control Low, Medium, High Device (L, M, H) Lot Number Reagent Lot Expiration Date Reaction Vessels Serial Number Sample Cups Septum Store at 2-8°C Replacement Caps Consult instructions for use Warning: May cause an allergic reaction Contains sodium azide. Contact Manufacturer with acids liberates very toxic gas. See REAGENTS section for a full explanation of symbols used in reagent component naming. 1 NAME REAGENTS ARCHITECT Progesterone Reagent Kit, 100 Tests INTENDED USE NOTE: Some kit sizes are not available in all countries or for use on all ARCHITECT i Systems. Please contact your local distributor. The ARCHITECT Progesterone assay is a Chemiluminescent Microparticle Immunoassay (CMIA) for the quantitative determination of progesterone in ARCHITECT Progesterone Reagent Kit (7K77) human serum and plasma. • 1 or 4 Bottle(s) (6.6 mL) Anti-fluorescein (mouse, monoclonal) fluorescein progesterone complex coated Microparticles SUMMARY AND EXPLANATION OF TEST in TRIS buffer with protein (bovine and murine) and surfactant Progesterone is produced primarily by the corpus luteum of the ovary stabilizers. Concentration: 0.1% solids. Preservatives: sodium azide in normally menstruating women and to a lesser extent by the adrenal and ProClin. cortex.1 At approximately the 6th week of pregnancy, the placenta 2-5 • 1 or 4 Bottle(s) (17.0 mL) Anti-progesterone (sheep, becomes the major producer of progesterone. -

Not for Publication United States District Court For
Case 3:10-cv-00603-PGS-DEA Document 289 Filed 06/29/12 Page 1 of 47 PageID: <pageID> NOT FOR PUBLICATION UNITED STATES DISTRICT COURT FOR THE DISTRICT OF NEW JERSEY TEVA WOMEN’S HEALTH, INC., Civil Action No.: Plaintiff, 10-603 (PGS) v. OPINION LUPIN, LTD. et al., Defendants. SHERIDAN, U.S.D.J. This case is a patent infringement action arising under the Hatch-Waxman Act involving Teva Women’s Health, Inc.’s (Teva) oral contraceptive (OC) Seasonique.1 Teva owns the patent-in-suit, U.S. Patent No. 7,320,969 (“the ’969 patent”). The ’969 patent, entitled “Oral contraceptives to prevent pregnancy and diminish premenstrual symptomology,” was issued on January 22, 2008. Teva’s predecessors-in-interest to the ’969 patent include Duramed and Barr.2 Teva alleges that defendants Lupin Ltd. and Lupin Pharmaceuticals, Inc. (collectively, “Lupin”) and defendants Mylan Inc., Mylan Pharmaceuticals, Inc., and Famy Care Ltd. (collectively, “Mylan”) infringed on Claim 19 of the ’969 patent. Claim 19 of the ’969 patent discloses an extended OC regimen that administers unopposed estrogen during the traditionally hormone free 1 While Seasonique and similar FDA-approved products are trademarked, in this opinion the Court refrains from using such marks for the sake convenience. 2 There is a lawsuit captioned Duramed Pharmaceuticals v. Watson Laboratories, Case No. 08-116 (D. Nev.) which involves the same patent and remains pending in Nevada. Although the parties knew of this other case, none of the parties sought to consolidate matters. Case 3:10-cv-00603-PGS-DEA Document 289 Filed 06/29/12 Page 2 of 47 PageID: <pageID> interval (HFI). -

Oregon Health Plan
Background Brief on… Oregon Health Plan Prepared by: Rick Berkobien May 2004 Background Volume 2, Issue 1 From 1989 to 1999, the Oregon Legislature passed a series of laws collectively known as the Oregon Health Plan (OHP). OHP expanded access to health care using a combi- Inside this Brief nation of public and private insurance plans and a prioritized list of health care services. Currently, more than 450,000 • Background Oregonians have access to health care under the OHP. The Department of Human Services (DHS), Office of Medi- • OHP Plus cal Assistance Programs (OMAP) administers the public insurance components of OHP, including Medicaid and the State Children’s Health Insurance Program (SCHIP). SCHIP • OHP Standard is a separate federal/state funded program to provide health care services to certain low-income children. • Family Health Insurance The Family Health Insurance Assistance Program (FHIAP), Assistance Program created by the 1997 Legislature, provides subsidies for the purchase of private health insurance by low-income workers. As part of OHP, FHIAP is currently funded solely with state • Proof for OHP Eligibility dollars—about $20 million in tobacco settlement funds—and the number of people served is capped at around 4,000. FHIAP currently provides services to people with incomes • The Insurance Pool up to 170 percent of the federal poverty level (FPL). Subsi- Governing Board dies range from 70 percent up to 95 percent of the premium costs depending on family size and income. • Staff and Agency Contacts House Bill 2519 (2001) modified the program to provide coverage to more uninsured Oregonians, have more flexibil- ity in the program’s benefits, secure more federal dollars, and help control the program’s rising medical costs. -

Application for Oregon Health Plan and Healthy Kids
Application for Oregon Health Plan and Healthy Kids Read this before you start. You can get this application in other formats. • This is for the Oregon Health Plan and Healthy Kids. You • This document can be provided upon request in alternative can apply for one or both programs with this application. formats for individuals with disabilities. Other formats may • Please answer all questions so we have the information include (but are not limited to) large print, Braille, audio we need to see if you qualify. recordings, Web-based communications and other electronic formats. Email [email protected], or call • Read the Green Booklet by clicking here. 1-800-699-9075 (voice) or TTY 711 to arrange for the It includes more information about the questions asked. alternative format that will work best for you. When you see this arrow, it means you may have to • You can get this application in another language or you send documents that show us the information you gave can get an interpreter. Call 1-800-699-9075 or TTY 711. is correct. Please mail copies of these documents along with your application to: For more information about: OHP Processing Center, • Healthy Kids or to find local application assistance, PO Box 14520, Salem, OR 97309-5044 click here: www.oregonhealthykids.gov or fax to 503-373-7493 • Oregon Health Plan, click here: www.oregon.gov/OHA/healthplan 1 About you. Please tell us about yourself, even if you are only applying for benefits for your children. You may need to send proof of immigration status or tribal affiliation if you are applying for yourself (see the checklist on page 16). -
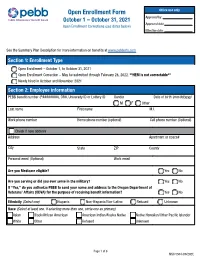
MSC 5504 PEBB Open Enrollment and Correction Form
Open Enrollment Form Office use only October 1 – October 31, 2021 Approved by: Approved date: Open Enrollment Corrections (see dates below) Effective date: See the Summary Plan Description for more information on benefits at www.pebbinfo.com Section 1: Enrollment Type F Open Enrollment – October 1, to October 31, 2021 F Open Enrollment Correction – May be submitted through February 28, 2022. **HEM is not correctable** F Newly hired in October and November 2021 Section 2: Employee information PEBB benefit number (P########), OR#, University ID or Lottery ID Gender Date of birth (mm/dd/yyyy) F M F F F Other Last name First name M.I. Work phone number Home phone number (optional) Cell phone number (Optional) F Check if new address Address Apartment or space# City State ZIP County Personal email (Optional) Work email Are you Medicare eligible? F Yes F No Are you serving or did you ever serve in the military? F Yes F No If “Yes,” do you authorize PEBB to send your name and address to the Oregon Department of Veterans’ Affairs (ODVA) for the purpose of receiving benefit information? F Yes F No Ethnicity (Select one): F Hispanic F Non-Hispanic/Non-Latino F Refused F Unknown Race (Select at least one. If selecting more than one, circle one as primary): F Asian F Black/African American F American Indian/Alaska Native F Native Hawaiian/Other Pacific Islander F White F Other F Refused F Unknown Page 1 of 8 MSC 5504 (09/2021) Section 3: Dependent information 1. List all eligible family members you want to provide coverage for. -
Oregon Health Plan (OHP) Is a State Program That Provides Health Care Coverage to Eligible Clients
Oregon Health Plan Client Handbook Department of Human Services October 2004 ii Accessible Services Communicating with Us Do you have a disability that makes it hard for you to read printed material? Do you speak a language other than English? We can give you information in one of several ways: Large print Audio tape Braille Computer disk Oral presentation (face-to-face or on the phone) Sign language interpreter Translations in other languages Let us know what you need. Tell your worker or, if you have no case worker, call 503-373-0333 x 393 or TTY 503-373-7800. Is Access a Problem? Do barriers in buildings or transportation make it hard for you to a� end meetings? To get state services? We can move our services to a more accessible place. We can provide the type of transportation that works for you. iii You Have a Right to Complain You can complain if: You keep ge� ing DHS printed forms and notices, but you need them some other way. Our programs aren’t accessible. You have 60 days to make your complaint. Send your complaint to: The Governor's Advocacy Offi ce 500 Summer St NE, E17 Salem, OR 97301 1-800-442-5238 1-800-945-6214 TTY 503-378-6532 Fax -or- US Dept of Health & Human Services Offi ce for Civil Rights 2201 Sixth Avenue, Mail Stop RX-11 Sea� le, WA 98121 1-800-362-1710 1-206-615-2296 TTY 1-206-615-2297 Fax [email protected] iv Contents Welcome to the Oregon Health Plan ............................................1 Prioritized List of Health Services ..........................................2 OHP Terms and Defi nitions -

FAQ: Hereditary Breast and Ovarian Cancer Syndrome (HBOC)
Patient FREQUENTLY ASKED QUESTIONS Hereditary Breast and Ovarian Cancer Syndrome February 2018 PUBLIC HEALTH Screenwise Table of Contents What is hereditary breast and ovarian cancer (HBOC) syndrome? .......3 Why is it important to know if my cancer was hereditary? ...................3 How do I find out if I have a hereditary cancer syndrome? ...................4 Personal and family history of cancer can be a sign of HBOC. ..............5 Where can I find a board-certified cancer genetic specialist? .............6 Will my health coverage pay for genetic counseling and testing? .......8 What are the BRCA genes? .....................................................................8 What if I don’t have coverage to pay for genetic counseling and testing? ..........................................................................9 Genetic privacy and anti-discrimination laws. .......................................9 What can I do to lower my risk for getting breast cancer and other cancers? ...............................................................................10 What is hereditary breast and ovarian cancer (HBOC) syndrome? HBOC stands for hereditary breast and ovarian cancer syndrome. Having HBOC does not mean that you have cancer, or that you will get cancer. Having HBOC means that you may have an increased risk for certain types of cancer. It also means that some of these cancers may run in your family, passing from generation to generation. • Women with HBOC are more likely to develop cancers, such as breast and ovarian cancer, than women without HBOC. • Men with HBOC are more likely to develop cancers, such as breast and prostate cancer, than men without HBOC. NOTE: HBOC can pass from either parent. Therefore, it is important to know as much as you can about your family health history on both sides.