COVID-19 Inpatients with Gastrointestinal Onset
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Azienda Usl Di Ferrara
Ferrara, 5 ottobre 2020 BOLLETTINO AGGIORNAMENTO SITUAZIONE CORONAVIRUS NELLA PROVINCIA DI FERRARA (dati riferiti al 4 ottobre 2020) I dati comunicati (raccolti dal Dipartimento di Sanità Pubblica dell’Azienda Usl e dalla Direzione Medica dell’Azienda Ospedaliero-Universitaria di Ferrara) si riferiscono alla fotografia scattata nell’arco delle 24 ore antecedenti questo comunicato (laddove non è indicato diversamente). I decessi di persone positive al coronavirus (elencati in questo bollettino) saranno comunicati all’Unità di Crisi della Provincia di Ferrara e ai mass media il più tempestivamente possibile e sono aggiornati in tempo reale. 1. TOTALE PAZIENTI COVID+ DECEDUTI Numero di persone positive al COVID decedute negli ospedali e territorio della provincia -- 2. TOTALE RICOVERI ALL’OSPEDALE DI CONA -- 3. TOTALE TAMPONI RISULTATI POSITIVI Numero di casi COVID POSITIVI refertati nell’ultimo giorno per l’intera provincia di Ferrara -- (dato relativo alla giornata di ieri) 4. TOTALE CASI ENTRATI IN ISOLAMENTO DOMICILIARE NELLE ULTIME 24 ORE Persone che sono state a contatto con una persona COVID positiva (o che rientrano 44 dall’estero) ma non hanno ancora fatto il tampone e non hanno sintomi 5. TOTALE CASI ENTRATI IN SORVEGLIANZA DOMICILIARE NELLE ULTIME 24 ORE Persone che hanno avuto un “contatto di un contatto”, asintomatici, monitorate dal -- Dipartimento di Sanità Pubblica Usl, tutti i giorni per 14 giorni, con una telefonata quotidiana al fine di sincerarsi sulle loro condizioni di salute 6. TOTALE PAZIENTI USCITI DALL’ISOLAMENTO DOM. O DALLA SORVEGLIANZA ATTIVA 43 (dato relativo alla giornata di ieri) 7. TOTALE PAZIENTI COVID DIMESSI/GUARITI Numero complessivo di persone COVID positive guarite o dimesse dall’ospedale di Cona -- 8. -

Abano Terme Acerra Aci Castello Acqualagna Acquanegra
Abano Terme Alzano Scrivia Azzano San Paolo Belvedere Marittimo Acerra Amelia Azzate Benevento Aci Castello Anagni Bagnaria Benna Acqualagna Ancarano Bagnatica Bentivoglio Acquanegra Cremonese Ancona Bagno A Ripoli Berchidda Adro Andezeno Bagnoli Di Sopra Beregazzo Con Figliaro Affi Angiari Bagnolo Cremasco Bereguardo Afragola Anguillara Veneta Bagnolo Di Po Bergamo Agliana Annicco Bairo Bernareggio Agliano Annone Di Brianza Baone Bertinoro Agliè Antrodoco Baranzate Besana in Brianza Agna Anzola D’Ossola Barasso Besenello Agordo Aosta Barbarano Vicentino Besnate Agrate Brianza Appiano Gentile Barberino Di Mugello Besozzo Agugliano Appiano sulla strada del vino Barberino Val D’Elsa Biassono Agugliaro Aprilia Barbiano Biella Aicurzio Arce Barchi Bientina Ala Arcene Bardello Bigarello Alano Di Piave Arco Bareggio Binago Alba Arconate Bariano Bioglio Alba Adriatica Arcore Barlassina Boara Pisani Albairate Arcugnano Barone Canavese Bolgare Albano Laziale Ardara Barzago Bollate Albaredo Arnaboldi Ardea Barzanò Bollengo Albaredo D’Adige Arese Basaluzzo Bologna Albavilla Arezzo Baselga Di Pinè Bolsena Albese Con Cassano Argelato Basiano Boltiere Albettone Ariccia Basiliano Bolzano Albiano Arluno Bassano Bresciano Bolzano Vicentino Albiate Arquà Petrarca Bassano Del Grappa Bomporto Albignasego Arquà Polesine Bassano In Teverina Bonate Sotto Albino Arre Bastida Pancarana Bonemerse Albiolo Arsago Seprio Bastiglia Bonorva Albisola Superiore Artegna Battaglia Terme Borghetto S. Spirito Albuzzano Arzachena Battuda Borgo San Dalmazzo Aldeno Arzano Baveno -

Provincia Di Ferrara Comuni Pop.Resid
Provincia di Ferrara Comuni Pop.resid. 1/1/2017 Sup. in Km2 Abitanti per Km2 Argenta 21.683 311,67 69,57 Berra 4.780 68,64 69,64 Bondeno 14.462 174,76 82,75 Cento 35.651 64,74 550,66 Codigoro 11.895 170,01 69,97 Comacchio 22.414 284,13 78,89 Copparo 16.425 157,01 104,61 Ferrara 133.087 405,16 328,48 Formignana 2.733 22,43 121,82 Jolanda di Savoia 2.916 108,34 26,92 Lagosanto 4.888 34,44 141,94 Masi Torello 2.326 22,71 102,43 Mesola 6.860 84,31 81,37 Ostellato 6.130 173,34 35,36 Poggio Renatico 9.881 80,23 123,15 Portomaggiore 11.765 126,64 92,90 Ro 3.250 43,2 75,24 Vigarano Mainarda 7.588 42,02 180,59 Voghiera 3.739 40,33 92,72 Tresigallo 4.434 20,62 214,99 Goro 3.758 33,18 113,27 Fiscaglia 9.018 116,18 77,62 Terre del Reno 10.009 51,03 196,14 Totale 349.692 2.635,12 132,70 Quadro riepilogativo degli ambiti territoriali e delle Unioni di Comuni Distretti sociosanitari Ambiti Territoriali Unioni di Comuni Evoluzione delle Unioni di Popolazione Sup. Abitanti Pr Ferrara Comuni complessiva in per 1/1/2017 Km2 Km2 Ovest Ambito Alto Unione Alto Insediata il settembre 2014 a 77.591 412,79 187,97 Ferrarese Ferrarese seguito della trasformazione Bondeno, (coincidente col distretto) (coincidente con dell’ex Associazione l’ambito) Cento, intercomunale dell’Alto Poggio Ferrarese costituita con gli stessi Comuni; a seguito Renatico, della fusione dei Comuni di Vigarano Mirabello e Sant'Agostino è Mainarda istituito dal 1 gennaio 2017 il Terre del Reno Comune di Terre del Reno Centro-Nord Ambito Terre e Unione dei Costituita il 1/12/2009 a seguito 31.622 -

Elenco Geometri
Geometri GEOMETRI N. Cognome Nome Indirizzo Recapito Comune Recapito Prov Recapito CAP Recapito Telefono Studio Telefono Cellulare EMail PEC 1 ALBIERI ANTONELLA VIA GARIBALDI, 130 FERRARA FE 44121 0532 212282 +393270584190 [email protected] [email protected] 2 ANTOLINI MARCO VIA FERRIERI, 14 S.BIAGIO ARGENTA FE 44011 0532 318593 0532 809625 +393388692405 [email protected] [email protected] 3 AZZAROLI ANTONIO VIA BORGO DEI LEONI, 21 FERRARA FE 44121 0532/55001 0532 770776 +393392804897 [email protected] [email protected] 4 BACCILIERI CATIA VIA UGO BASSI, 13 FERRARA FE 44121 0532/205273 0532 820302 +393389793907 [email protected] [email protected] 5 BARALDI BARBARA VIA BORGOLEONI, 116 FERRARA FE 44121 0532 211246 0532 63725 +393297156334 [email protected] [email protected] 6 BARBANTI GIANRICO VIA VITTORIA, 30 FERRARA FE 44100 0532 763910 +393477360064 [email protected] [email protected] 7 BARICORDI NICOLA VIA DON G. MINZONI, 16 OSTELLATO FE 44020 0533/681862 +393392566533 [email protected] [email protected] 8 BECCARI MASSIMO Viale dei Castagni 30/32 LIDO DEGLI ESTENSI FE 44029 0533 324479 0533325747 +393356118769 [email protected] [email protected] 9 BENINI ELENA VIA COSME' TURA, 39 INT. 8 FERRARA FE 44121 0532472463 0532 792062 +393347486500 [email protected] [email protected] 10 BERTARELLI ANTONIO FRANCESCO VIA C.COLOMBO, 12 LAGOSANTO FE 44023 +393382761787 [email protected] [email protected] 11 BERTAZZINI ANDREA P.TTA SCHIATTI, 8 FERRARA FE 44121 0532 206471 0532 67159 +393358056481 [email protected] [email protected] 12 BERTELLI ALESSANDRA VIA ALBERTO LOLLIO, 7 INT. -

Percorso E Dettaglio Mappe
68 ✶ ✁ ✷✂ Ro Via Tr Pomposa ava SP4 Valcesura glio I se - 4,5 dr rare Po 6 Cornacervina o v ia F er Via d M i atr an V St a o Museo SP68 rada C l ora Medelana St a del Trotto Via Travaglio m rada i in Ze n rt III o Idrovia Ferrarese - Canale Navigabile a rb o A. F ele in ia anu a V Em SP23 .so V. 19 C Migliarino Nigr SP1 Via iso 1 li Ponte ti Via Via Roma tis itale Arzana S at San V 1 tagn Via Cesare B Via ane Via Comac chio o r o g Rovereto i a Alberlungo d 3,5 g o V la i C ia u . d b o ov Bosco i r n Strada Gam r. P e h Raccordo Autostradale St 1,5 c 2 SP39 c Ferrara - Porto Garibaldi a 23 m o i C r e a a i hi i cc b e l arav V San Vito M A ada tr a S Pieve di i San Vito Dogato V 2 1,5 Campolungo ro ada P vinciale di Codigoro SP1 Str Ferrara SP1 Strad a D i a 1,5 Via Pioppa nti hina Cavalieri c 2 1 Via Don G. FE 422 Strada Isac Via Ariosto Via G. Garibaldi Oasi SP68 andrino Museo del Anse Vallive Strada Imola Via Ca’ S Libolla Ostellato Borgo Fornace Territorio di Ostellato o Tresigallo Via Canova nc ro SP15 T II lio SP4 g FE 213 va Ferrara a 3,5 i Tr Via del Mare in ia n V Final di Rero a o sc n SP68 o Pomposa T V A. -

Progetto Definitivo
PROGETTO DEFINITIVO DIPARTIMENTO PER LE INFRASTRUTTURE, GLI AFFARI GENERALI ED IL PERSONALE STRUTTURA DI VIGILANZA SULLE CONCESSIONARIE AUTOSTRADALI Elenco Ditte N. ORDINE : 1 Commessa : 111306 Autostrada : (A13): BOLOGNA - PADOVA Tratto : BOLOGNA - FERRARA Lotto Comune : [H2AU] POGGIO RENATICO (FE) DITTA CATASTALE : DEMANIO PUBBLICO DELLO STATO PER OPERE IDRAULICHE DI II CATEGORIA C.F. (proprieta' 1000/1000) - PROPRIETA’ REALE : DEMANIO PUBBLICO DELLO STATO PER OPERE IDRAULICHE DI II CATEGORIA C.F. (proprieta' 1000/1000) - REFERENTE : OSSERVAZIONI : Terreni Agricoli N.Piano Foglio Mappale Qualità catastale Classe Red. Dom. Red. Agr. Sup. cat. Sup. occ. Titolo Occ. 1 75 171 SEMINATIVO 1 71,84 35,17 8310 348 Sede Autostrada 1 75 172 SEMINATIVO 3 166,24 101,35 24530 1402 Sede Autostrada 1 75 41 SEMINATIVO 1 109,43 53,72 12820 222 Sede Autostrada 1 75 42 SEMINATIVO 3 229,14 139,69 33810 798 Sede Autostrada 1 75 171 SEMINATIVO 1 71,84 35,17 8310 79 Occupazione Temporanea 1 75 172 SEMINATIVO 3 166,24 101,35 24530 300 Occupazione Temporanea 1 75 41 SEMINATIVO 1 109,43 53,72 12820 79 Occupazione Temporanea 1 75 42 SEMINATIVO 3 229,14 139,69 33810 289 Occupazione Temporanea 3517 Totale Superficie occupata mq 3517 Pagina 1 Elenco Ditte N. ORDINE : 2 Commessa : 111306 Autostrada : (A13): BOLOGNA - PADOVA Tratto : BOLOGNA - FERRARA Lotto Comune : [H2AU] POGGIO RENATICO (FE) DITTA CATASTALE : CERIOLI Dino nato a POGGIO RENATICO il 18/11/1946 C.F. CRLDNI46S18G768W (proprieta' 1000/1000) - PROPRIETA’ REALE : CERIOLI Dino nato a POGGIO RENATICO il 18/11/1946 C.F. CRLDNI46S18G768W (proprieta' 1000/1000) - REFERENTE : OSSERVAZIONI : Terreni Agricoli N.Piano Foglio Mappale Qualità catastale Classe Red. -

GUIDA ALLA RACCOLTA DIFFERENZIATA Tutto Quello Che C’È Da Sapere Per Diventare Campioni Di Riciclo
GUIDA ALLA RACCOLTA DIFFERENZIATA Tutto quello che c’è da sapere per diventare campioni di riciclo. Nell’ottica dei princìpi dell’economia Chi è Clara spa circolare, per CLARA è importante coinvolgere attivamente cittadini, istituzioni, soci e dipendenti in un modello Oggi gestisce la raccolta dei rifiuti in 21 dei 23 Comuni di sviluppo sostenibile (socialmente CLARA è la società ed economicamente), favorendo e a totale capitale della provincia di Ferrara: Berra, Bondeno, Cento, Codigoro, Comacchio, Copparo, Fiscaglia, Formignana, promuovendo la partecipazione collettiva pubblico nata nel Goro, Jolanda di Savoia, Lagosanto, Masi Torello, Mesola, verso un interesse comune e premiando i 2017 dalla fusione Ostellato, Poggio Renatico, Portomaggiore, Ro, Terre del comportamenti virtuosi. tra Area e Cmv Reno, Tresigallo, Vigarano Mainarda e Voghiera. Raccolta. Terza società per dimensioni in Emilia-Romagna, CLARA è affidataria del servizio di gestione rifiuti in un bacino d’utenza che conta 120.000 clienti domestici e 13.500 non domestici, su un territorio di quasi 2.000 chilometri I servizi di Clara spa quadrati. Impiega circa 430 dipendenti. Il sistema di raccolta prevalente è quello domiciliare, che prevede in quasi tutto il territorio servito la raccolta porta i ritiri su chiamata di a porta di cinque frazioni materiali ingombranti, grandi potature, inerti domestici, di rifiuti (indifferenziato, pneumatici, eternit umido organico, imballaggi in plastica e lattine, carta e cartone, sfalci e potature). A queste si aggiunge il servizio di raccolta del vetro, perlopiù svolto i Centri comunali o tramite campane stradali, con l’eccezione di alcuni centri storici in intercomunali di raccolta cui anche per il vetro è attivo il servizio domiciliare. -
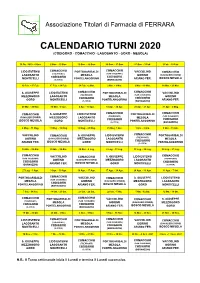
CODIGORO 2020 Etc Modello TURNI
Associazione Titolari di Farmacia di FERRARA CALENDARIO TURNI 2020 (CODIGORO - COMACCHIO - LAGOSANTO - GORO - MESOLA) 30 Dic. 2019 - 6 Gen. 6 Gen. - 13 Gen. 13 Gen. - 20 Gen. 20 Gen. - 27 Gen. 27 Gen. - 3 Feb. 3 Feb. - 10 Feb. COMACCHIO LIDO ESTENSI COMACCHIO PORTOGARIBALDI VACCOLINO COMACCHIO (TREPPONTI) (SAN CASSIANO) LAGOSANTO MESOLA GORINO (CAVALIERI D'ORO) CODIGORO CODIGORO MONTICELLI PONTELANGORINO ARIANO FER. BOSCO MESOLA (S. RITA) (BORNAZZINI) 10 Feb. - 17 Feb. 17 Feb. - 24 Feb. 24 Feb. - 2 Mar. 2 Mar. - 9 Mar. 9 Mar. - 16 Mar. 16 Mar. - 23 Mar. S. GIUSEPPE LIDO ESTENSI COMACCHIO PORTOGARIBALDI COMACCHIO VACCOLINO (SAN CASSIANO) MEZZOGORO LAGOSANTO (TREPPONTI) MESOLA GORINO CODIGORO CODIGORO GORO MONTICELLI PONTELANGORINO ARIANO FER. (S. RITA) (BORNAZZINI) 23 Mar. - 30 Mar. 30 Mar. - 6 Apr. 6 Apr. - 13 Apr. 13 Apr. - 20 Apr. 20 Apr. - 27 Apr. 27 Apr. - 4 Mag. COMACCHIO COMACCHIO S. GIUSEPPE LIDO ESTENSI COMACCHIO PORTOGARIBALDI (TREPPONTI) (SAN CASSIANO) (CAVALIERI D'ORO) MEZZOGORO LAGOSANTO MESOLA CODIGORO CODIGORO BOSCO MESOLA GORO MONTICELLI PONTELANGORINO (S. RITA) (BORNAZZINI) 4 Mag. - 11 Mag. 11 Mag. - 18 Mag. 18 Mag. - 25 Mag. 25 Mag. 1 Giu. 1 Giu. - 8 Giu. 8 Giu. - 15 Giu. VACCOLINO COMACCHIO S. GIUSEPPE LIDO ESTENSI COMACCHIO PORTOGARIBALDI (TREPPONTI) GORINO (CAVALIERI D'ORO) MEZZOGORO LAGOSANTO MESOLA CODIGORO BOSCO MESOLA PONTELANGORINO ARIANO FER. GORO MONTICELLI (S. RITA) 15 Giu. - 22 Giu. 22 Giu. - 29 Giu. 29 Giu. - 6 Lug. 6 Lug. - 13 Lug. 13 Lug. - 20 Lug. 20 Lug. - 27 Lug. COMACCHIO VACCOLINO COMACCHIO S. GIUSEPPE LIDO ESTENSI COMACCHIO (SAN CASSIANO) (TREPPONTI) GORINO (CAVALIERI D'ORO) MEZZOGORO LAGOSANTO CODIGORO CODIGORO ARIANO FER. -

Using the Ecosystem Services Framework for Policy Impact
sustainability Article Using the Ecosystem Services Framework for Policy Impact Analysis: An Application to the Assessment of the Common Agricultural Policy 2014–2020 in the Province of Ferrara (Italy) Parthena Chatzinikolaou 1,* ID , Davide Viaggi 1 ID and Meri Raggi 2 ID 1 Department of Agricultural and Food Sciences, University of Bologna, 40127 Bologna, Italy; [email protected] 2 Department of Statistical Sciences, University of Bologna, 40126 Bologna, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-051-2096-120 Received: 2 February 2018; Accepted: 17 March 2018; Published: 20 March 2018 Abstract: The objective of this study is to test a methodology for the classification of areas according to the provision of ecosystem services and for the evaluation of the effects of different agricultural policy scenarios. The evaluation focuses on the different categories of Ecosystem Services (ES) and applies a set of indicators available from secondary data sources. Two scenarios were compared, represented by the pre-2014 CAP and the CAP 2014–2020, based on the measures of the RDP 2014–2020 focused on enhancing ecosystems. The approach was implemented under two weighting solutions. First, we assumed that all indicators have equal weight. As a further step, the framework was integrated with a weighting procedure in order to account for the different importance of the various ES indicators. All municipalities offer a significant number of provisioning and cultural services, mainly connected to recreational opportunities. The indicators with higher importance in the area represent provisioning, supporting and regulating services, while cultural services have received less attention. -

Ferrara Ostellato
Along the Po di Volano 6 Technical notes Pomposa Ferrara Second stage - From Ostellato to Pomposa Abbey Depart: Ostellato, Piazza Repubblica Ostellato ra st Arrive: Codigoro, Abbazia di Pomposa www.ferrarainfo.com ai M i d Length: 29,910 km Ferrara: o P Difficulty level: suitable for everyone. Level Castello Estense • tel. 0532 299303 Codigoro: route mainly along cycle paths (partly on dirt F Po track). Some stretches along minor roads with Abbazia di Pomposa • tel. 0533 719110 Fium iume e P Berra Serravalle little traffic. o Connections with other routes ia Albersano Po di Venez Guarda Alberone Cologna Railways Ferrarese Ponte 5 Ferrara - Ostellato Oasi Punzetti Ferrara/Codigoro Ariano 7 Ro - Ostellato Mulino del Po BicycleFerrarese transport available. Zerbinate Please check timetables and availability. 8 OstellatoOasi - Argenta Stellata Bosco di Pilastri Info: 800 91 50 30 • www.fer.it 10 MesolaSanta - Lidi di Comacchio - Comacchio Malcantone Zocca Ro Massenzatica Giustina Contane Ponti Oasi Isola Coccanile Spagna Oasi Bonello Pepoli Oasi Bosco Ravalle Codigoro Monticelli Pineta di di Porporana Mesola S. Giustina Fossadalbero Cesta Mesola Ambrogio S. Biagio Porporana Salvatonica RuinaFrom Ostellato, the meetingPonte place S. Pietro of many journeys and an agreeable centre for a born out of the left flankDune Fossiliof the di Po di Volano, more evidence of how everything Mezzogoro Massenzatica Gavello Burana Oasi Isola Pescara Sabbioni Bianca visitCamatte to nature reserves, the route follows the Po di Volano, identified in the Etrus- in the Ferrarese lands is determined by the presence of water. The journeyP arrives Casaglia Zenzalino o d Francolino P i G Francolino Codigoro Jolanda di Savoia ItalbaPomposa Abbey o no Settepolesini can Salettaperiod with the mythical Eridano. -

25,8% 7,0% 6,2% 20,5% 22,5%
Anno 2020 LAGOSANTO over 65 POPOLAZIONE 34 Kmq 27% 138 abitanti per Kmq under 20 226 15% 4511 4.737 stranieri ROMANIA italiani Prima comunita' straniera 247 ogni 100 La media provinciale è anziani giovani 262 ogni 100 > 65 anni < 15 anni Dati InfoCamere - Imprese Attive al 31/12/2020 ATTIVITA' ECONOMICHE 25,8% 92 22 6,2% agricoltura manifattura 3,4% 80 immobiliari 12 16 356 22,5% 4,5% 21 costruzioni altri servizi 8 25 7 5,9% 73 servizi alla persona 2,2% 2,0% 7,0% trasporto e noleggio, alloggio e magazzino 20,5% agenzie viaggi ristorazione commercio IMPRESE 277 31 FEMMINILI GIOVANILI LAGOSANTO 440 22,2% 325 8,7% 79 356 361 Provincia in aumento stabili 34.601 2° Comune per 30.913 31.226 incidenza di artigiane -1,4% 223 Variaz. annuale -1,0% STRANIERE 328 ARTIGIANE -19,1% 28 7,9% 37,4% Variaz. decennale -10,7% 133 2020 2019 2010 2020 2019 2010 in calo in aumento % di imprese di Lagosanto rispetto ATTIVITA' A CONFRONTO ai comuni più specializzati Lagosanto 3,1% Lagosanto 5,1% Bondeno 5,9% Portomaggiore 5,1% Terre del Reno 4,3% Poggio Renatico 5,0% Provincia di Ferrara 2,0% Provincia di Ferrara 4,1% F0 abbricazio2n0e macchin4a0ri e appare6c0 chi 0 10 Serv2i0zi alla3 p0 erson40a 50 Lagosanto 16,0% Lagosanto 6,5% Poggio Renatico 14,8% Jolanda di Savoia 6,5% Terre del Reno 14,4% Comacchio 4,1% Provincia di Ferrara 10,9% Provincia di Ferrara 3,3% 0 Costruz5i0oni speci1a0l0izzate 150 0 Cos2t0ruzioni di4 0edifici 60 Censimento permanente della popolazione 2019 VALORE AGGIUNTO LAVORO 11,4% 10,2% Stima Previsione 100 8,8% Variazione 2020 su 2019 Variazione -

4 56* 34 43 17 68 74* 71 24
Ferrara, 17 aprile 2020 BOLLETTINO AGGIORNAMENTO SITUAZIONE CORONAVIRUS NELLA PROVINCIA DI FERRARA (dati riferiti al 16 aprile 2020) I dati comunicati (raccolti dal Dipartimento di Sanità Pubblica dell’Azienda Usl e dalla Direzione Medica dell’Azienda Ospedaliero-Universitaria di Ferrara) si riferiscono alla fotografia scattata nell’arco delle 24 ore antecedenti questo comunicato (laddove non è indicato diversamente). I decessi di persone positive al coronavirus (elencati in questo bollettino) saranno comunicati all’Unità di Crisi della Provincia di Ferrara e ai mass media il più tempestivamente possibile e sono aggiornati in tempo reale. 1. TOTALE PAZIENTI COVID+ DECEDUTI Numero di persone positive al COVID decedute negli ospedali e territorio della provincia 4 2. TOT. RICOVERI IN OSPEDALE (POSITIVI, SOSPETTI E AL DOMICILIO) Numero complessivo di persone “COVID positive” e sospette ricoverate negli ospedali di Cona e del Territorio + pazienti positivi al domicilio 56* (dato relativo alla giornata del 16 aprile 2020) * 56 (di cui 2 fuori provincia) e 1 caso sospetti a CENTO 3. TOTALE TAMPONI RISULTATI POSITIVI Numero di casi COVID POSITIVI refertati nell’ultimo giorno per l’intera provincia di Ferrara 34 (dato relativo alla giornata del 16 aprile 2020) 4. TOTALE CASI ENTRATI IN ISOLAMENTO DOMICILIARE NELLE ULTIME 24 ORE Persone che sono state a contatto con una persona COVID positiva (o che rientrano 43 dall’estero) ma non hanno ancora fatto il tampone e non hanno sintomi. 5. TOTALE CASI ENTRATI IN SORVEGLIANZA DOMICILIARE NELLE ULTIME 24 ORE Persone che hanno avuto un “contatto di un contatto”, asintomatici, monitorate dal Di- 17 partimento di Sanità Pubblica Usl, tutti i giorni per 14 giorni, con una telefonata quotidia- na al fine di sincerarsi sulle loro condizioni di salute.